- Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece
- Radiology Department, Interbalkan European Medical Center, Thessaloniki, Greece
Correspondence Address:
Stylianos Kapetanakis
Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece
DOI:10.4103/sni.sni_125_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Grigorios Gkasdaris, Danai Chourmouzi, Apostolos Karagiannidis, Stylianos Kapetanakis. Spinal cord edema with contrast enhancement mimicking intramedullary tumor in patient with cervical myelopathy: A case report and a brief literature review. 13-Jun-2017;8:111
How to cite this URL: Grigorios Gkasdaris, Danai Chourmouzi, Apostolos Karagiannidis, Stylianos Kapetanakis. Spinal cord edema with contrast enhancement mimicking intramedullary tumor in patient with cervical myelopathy: A case report and a brief literature review. 13-Jun-2017;8:111. Available from: http://surgicalneurologyint.com/surgicalint-articles/spinal-cord-edema-with-contrast-enhancement-mimicking-intramedullary-tumor-in-patient-with-cervical-myelopathy-a-case-report-and-a-brief-literature-review/
Abstract
Background:Cervical myelopathy (CM) is a clinical diagnosis that may be associated with hyperintense areas on T2-weighted magnetic resonance imaging (MRI) scan. The use of contrast enhancement in such areas to differentiate between neoplastic and degenerative disease has rarely been described.
Case Description:We present a 41-year-old female with a 5-month course of progressive CM. The cervical MRI revealed spinal cord swelling, stenosis, and a hyperintense signal at the C5–C6 and C5–C7 levels. Both the neurologic and radiologic examinations were consistent with an intramedullary cervical cord tumor. To decompress the spinal canal, an anterior cervical discectomy and fusion was performed from C5 to C7 level. This resulted in immediate and significant improvement of the myelopathy. Postoperatively, over 1.5 years, the hyperintense, enhancing intramedullary lesion gradually regressed on multiple postoperative MRI scans.
Conclusion:Spinal cord edema is occasionally seen on MR studies of the cervical spine in patients with degenerative CM. Contrast-enhanced MR studies may help differentiate hyperintense cord signals due to edema vs. atypical intramedullary tumors. Routine successive postoperative MRI evaluations are crucial to confirm the diagnosis of degenerative vs. neoplastic disease.
Keywords: Cervical myelopathy, cervical spondylosis, contrast enhancement, intramedullary lesion, spinal cord edema, spinal cord swelling, spinal tumors
INTRODUCTION
Several non-neoplastic intramedullary pathologies can mimic intramedullary tumors; these include edema due to myelopathy, demyelination, granulomatous disease, infections, radiation myelopathy, vascular lesions, and syringomyelia.[
Here, we report the case of a 41-year-old female with cervical spondylosis at the C5–C6 level whose MRI scan revealed spinal cord swelling, atypical enlargement, and hyperintensity of the cord on the T2-weighted image and contrast enhancement with gadolinium (T1-weighted) [
CASE REPORT
Medical history and examination
A 41-year-old female, who had not sustained any trauma, initially presented with weakness/numbness involving all four extremities and progressive sphincter dysfunction over the last 2 months. When the cervical noncontrast MRI showed a hyperintense intramedullary cord signal, the differential diagnoses included cervical spondylotic myelopathy and tumor. She was referred for an open biopsy of the cervical spinal cord to document the pathology of the tumor. At the time of her transfer, her severe spastic quadriparesis was markedly greater in the upper than in the lower extremities. The follow-up MRI revealed cervical spondylosis with C5–C6 and C6–C7 cord compression associated with an extensive intramedullary high cord signal and cord enlargement on the T2-weighted sagittal images extending from C5 to C7 [
Operation and postoperative evaluation
The patient underwent an anterior cervical discectomy and fusion from C5 to C7 using PEEK (PolyEtherEtherKetone) intervertebral cages. No histopathologic evidence was finally taken. There was significant postoperative motor/sensory improvement in her spastic quadriparesis and she retained normal in bladder function. The cervical MRI performed 1 month later demonstrated no significant changes in the intramedullary lesion [
Figure 2
Postoperative MRI. (a) One month after surgery, sagittal MRI demonstrated slight decrease of the intramedullary high intensity on T2-weighted images. The high-intensity signal is still atypically extended beyond the point of compression. (b) T1-weighted MRI sagittal scan with persisting contrast enhancement at level C5–C6 1 month after surgery
DISCUSSION
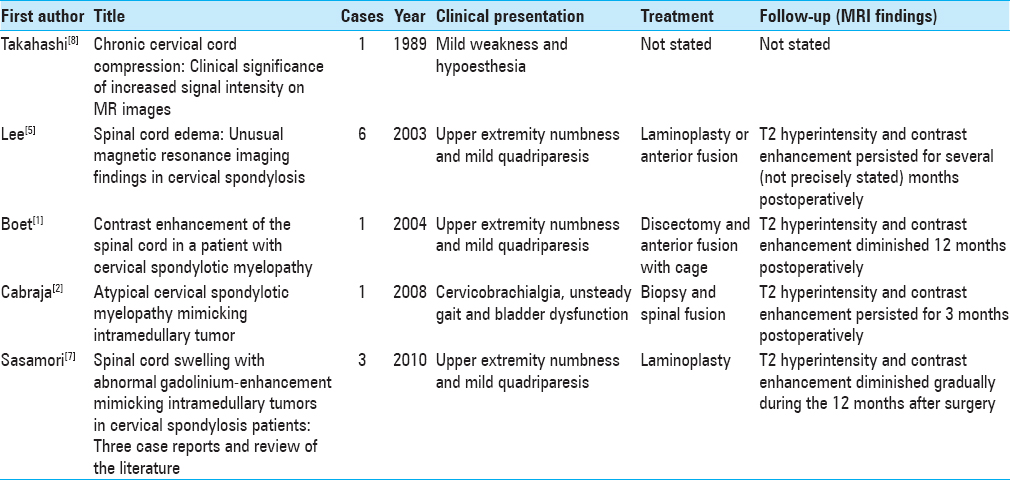
Sasamori et al. reported non-neoplastic lesions mimicking intramedullary tumors on T2-weighted MRI; patients with spondylotic disease may also demonstrate hyperintensity attributed to spinal cord swelling while also showing some gadolinium enhancement.[
Most patients presented with MR-documented hyperintense intramedullary lesions with cord enlargement opposite to levels of maximal compression. In our case, the edema of the spinal cord was larger than it should be, extending the point of maximum compression at C5–C6; and the contrast enhancement was localized directly at the site of the greatest narrowing of the spinal canal. After surgery, patients with degenerative pathology demonstrated extensive clinical improvement, however, MR resolution of cord edema/swelling lagged (e.g., in this case by 18 months).
Surgical decompression may be performed by an anterior or posterior approach depending on the type/location of pathology.[
Magnetic resonance diagnosis of pathology
MRI, particularly the hyperintense intramedullary cord signals with/without gadolinium, best helps differentiate between spinal stenosis/spondylosis/CM and an intramedullary spinal cord tumor. It may reflect whether someone is suffering from CM or tumor. New techniques that use advanced MRI are emerging and providing exciting new tools for assessing the spinal cord in patients with degenerative CM.[
CONCLUSION
Spinal cord edema is occasionally seen with cervical spondylosis/CSM (cervical spondylotic myelopathy). When an intramedullary hyperintense lesion is seen that enhances with gadolinium, differentiating between CSM and tumor may be difficult. In cases where there is rapid clinical deterioration, an initial decompression/fusion should be considered. Successive postoperative MR studies with/without enhancement may then be used to further differentiate between CSM and tumor.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Boet R, Chan Y-L, King A, Mok CT, Poon WS. Contrast enhancement of the spinal cord in a patient with cervical spondylotic myelopathy. J Clin Neurosci. 2004. 11: 512-4
2. Cabraja M, Abbushi A, Costa-Blechschmidt C, van Landeghem FK, Hoffmann KT, Woiciechowsky C. Atypical cervical spondylotic myelopathy mimicking intramedullary tumor. Spine (Phila Pa 1976). 2008. 33: E183-7
3. Hida K, Iwasaki Y. Surgical approach for nonneoplastic intramedullary lesions. Rinsho Shinkeigaku. 2002. 42: 1105-6
4. Joaquim AF, Ghizoni E, Tedeschi H, Hsu WK, Patel AA. Management of degenerative cervical myelopathy-An update. Rev Assoc Med Bras. 2016. 62: 886-94
5. Lee J, Koyanagi I, Hida K, Seki T, Iwasaki Y, Mitsumori K. Spinal cord edema: Unusual magnetic resonance imaging findings in cervical spondylosis. J Neurosurg. 2003. 99: 8-13
6. Nouri A, Martin AR, Mikulis D, Fehlings MG. Magnetic resonance imaging assessment of degenerative cervical myelopathy: A review of structural changes and measurement techniques. Neurosurg Focus. 2016. 40: E5-
7. Sasamori T, Hida K, Yano S, Takeshi A, Iwasaki Y. Spinal cord swelling with abnormal gadolinium-enhancement mimicking intramedullary tumors in cervical spondylosis patients: Three case reports and review of the literature. Asian J Neurosurg. 2010. 5: 1-9
8. Takahashi M, Yamashita Y, Sakamoto Y, Kojima R. Chronic cervical cord compression: Clinical significance of increased signal intensity on MR images. Radiology. 1989. 173: 219-24