- Department of Neurological Surgery, The Ohio State University Wexner Medical Center,
- Department of Neurological Surgery, The Ohio State University College of Medicine, Columbus, Ohio, United States.
Correspondence Address:
David Gibbs, The Ohio State University College of Medicine, Columbus, Ohio, United States.
DOI:10.25259/SNI_254_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dominic Maggio1, Andrew Grossbach1, David Gibbs2, Robert Moranville2, Nathaniel Toop1, David Xu1, Stephanus Viljoen1. Spinal deformity correction in ankylosing spondylitis. 08-Apr-2022;13:138
How to cite this URL: Dominic Maggio1, Andrew Grossbach1, David Gibbs2, Robert Moranville2, Nathaniel Toop1, David Xu1, Stephanus Viljoen1. Spinal deformity correction in ankylosing spondylitis. 08-Apr-2022;13:138. Available from: https://surgicalneurologyint.com/surgicalint-articles/11511/
Abstract
Background: Ankylosing spondylitis (AS) is a complex, debilitating disease with few available medical therapies in its later stages.
Methods: We reviewed current clinical approaches for caring for AS patients with an emphasis on the risks and outcomes associated with surgical intervention.
Results: It is critical to understand the natural history and surgical outcomes of patient with AS. Surgery is not without risks, as a vertebral body osteotomy is often required to re-establish spinopelvic equilibrium. However, surgery can lead to clinical improvements in pain, disability, cardiac function, respiration, digestion, and sexual activity.
Conclusion: Deformity correction for AS should be carefully considered in symptomatic patients.
Keywords: Ankylosing spondylitis, Deformity, Osteotomy, Spondyarthropathy
INTRODUCTION
Ankylosing spondylitis (AS) is a complex and debilitating disease of the axial skeleton that affects 0.9% of the global population.[
CLINICAL MANIFESTATIONS OF AS
Clinical manifestations of spondyloarthropathies (SpAs) are generally split into articular and extra-articular involvement. Articular symptoms include chronic inflammatory axial back pain, oligoarthritis, and enthesitis. Extra-axial involvement classically includes inflammatory bowel disease, psoriasis, and anterior uveitis.[
NEUROLOGICAL COMPLICATIONS OF AS
Neurologic complications of AS include: spinal cord injury, monophasic myelopathy, cauda equina syndrome, and even transverse myelitis.[
SURGERY
Surgical intervention in AS centers around appendicular joint surgery, stabilization of spinal fractures, and spinal deformity correction to regain physiologic alignment.[
Spinal fractures
Generalized spinal osteopenia is a hallmark of AS, and fractures most commonly occur at the C7-T1 junction. Surgical treatment for fractures is imperative, especially in patients with evidence of instability, pseudoarthrosis, repeated fractures, and/or evidence of neurologic impairment.[
Corrective osteotomies
Corrective osteotomy of the lumbar spine is frequently necessary to restore sagittal balance, and several distinct forms of osteotomies may be used depending on the overall goals of surgery and amount of correction required. These range from posterior column osteotomies such as Smith-Peterson Osteotomies, to more invasive three column osteotomies such as pedicle subtraction osteotomies and vertebral column resections.[
CONCLUSION
AS is a debilitating disease with few available pharmacological therapies. Surgical intervention for AS is associated with improvements in musculoskeletal, pulmonary, cardiac, digestive, and sexual functioning.[
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest or disclosures relevant to any aspect of this submission and manuscript. Listed below are all disclosures: Andrew Grossbach, MD: Research funding from DePuy, Medtronic, 3M/KCI; consultation fees from 3M/KCI Stephanus Viljoen, MD: Research funding from Medtronic David Xu, MD: NuVasive consultation fees.
References
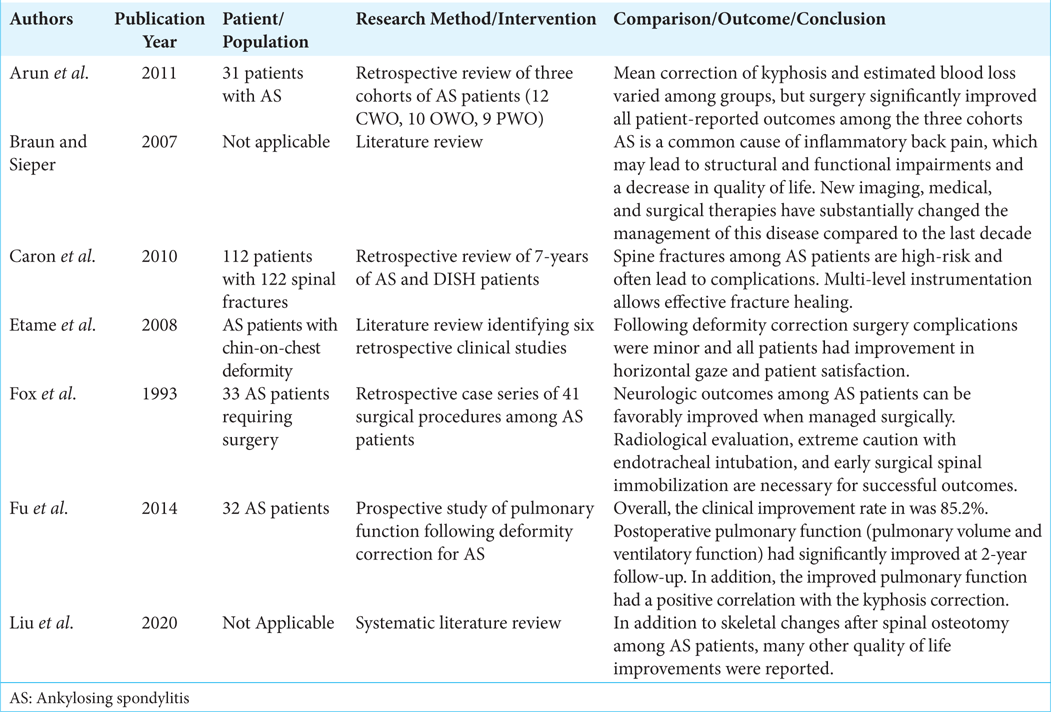
1. Arun R, Dabke HV, Mehdian H. Comparison of three types of lumbar osteotomy for ankylosing spondylitis: A case series and evolution of a safe technique for instrumented reduction. Eur Spine J. 2011. 20: 2252-60
2. Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007. 369: 1379-90
3. Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine. 2010. 35: E458-64
4. Etame AB, Than KD, Wang AC, La Marca F, Park P. Surgical management of symptomatic cervical or cervicothoracic kyphosis due to ankylosing spondylitis. Spine (Phila Pa 1976). 2008. 33: E559-64
5. Fox MW, Onofrio BM, Kilgore JE. Neurological complications of ankylosing spondylitis. J Neurosurg. 1993. 78: 871-8
6. Fu J, Song K, Zhang YG, Zheng GQ, Zhang GY, Liu C. Changes in cardiac function after pedicle subtraction osteotomy in patients with a kyphosis due to ankylosing spondylitis. Bone Joint J. 2015. 97: 1405-10
7. Fu J, Zhang G, Zhang Y, Liu C, Zheng G, Song K. Pulmonary function improvement in patients with ankylosing spondylitis kyphosis after pedicle subtraction osteotomy. Spine. 2014. 39: E1116-22
8. Liu J, Kang N, Zhang Y, Hai Y. Systemic changes associated with quality of life after surgical treatment of kyphotic deformity in patients with ankylosing spondylitis: A systematic review. Eur Spine J. 2020. 29: 794-802