- Department of Neurological Surgery, Ohio State University Wexner Medical Center, Ohio, United States.
DOI:10.25259/SNI_160_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kristin Huntoon, Umang Khandpur, David Dornbos, Patrick P Youssef. Spinal dural arteriovenous fistula masquerading as subdural hematoma. 06-Jun-2020;11:142
How to cite this URL: Kristin Huntoon, Umang Khandpur, David Dornbos, Patrick P Youssef. Spinal dural arteriovenous fistula masquerading as subdural hematoma. 06-Jun-2020;11:142. Available from: https://surgicalneurologyint.com/surgicalint-articles/10070/
Abstract
Background: This case highlights an angiographically occult spinal dural AVF presenting with a spinal subdural hematoma. While rare, it is important that clinicians be aware of this potential etiology of subdural hematomas before evacuation.
Case Description: A 79-year-old female presented with acute lumbar pain, paraparesis, and a T10 sensory level loss. The MRI showed lower cord displacement due to curvilinear/triangular enhancement along the right side of the canal at the T12-L1 level. The lumbar MRA, craniospinal CTA, and multivessel spinal angiogram were unremarkable. A decompressive exploratory laminectomy revealed a subdural hematoma that contained blood products of different ages, and a large arterialized vein exiting near the right L1 nerve root sheath. The fistula was coagulated and sectioned. Postoperatively, the patient regained normal function.
Conclusion: Symptomatic subdural thoracolumbar hemorrhages from SDAVF are very rare. Here, we report a patient with an acute paraparesis and T10 sensory level attributed to an SDAVF and subdural hematoma. Despite negative diagnostic studies, even including spinal angiography, the patient underwent surgical intervention and successful occlusion of the SDAVF.
Keywords: Angiographically occult, Arteriovenous fistula, Subdural hematoma, Vascular malformation
INTRODUCTION
Type 1 spinal arteriovenous malformation (AVM), also referred to as dural arteriovenous fistulas (AVF), is the most common type of spinal vascular malformation. They are classically located along the dorsal aspect of the thoracolumbar cord and typically present in patients in their sixth or seventh decade of life. Symptoms and signs may reflect an acute evolving or chronic progressive myelopathy characterized by back/radicular pain, progressive paraparesis, paresthesias, and/or sphincter dysfunction.[
CASE REPORT
History and physical examination
A 79-year-old female with a history of breast cancer and hypertension presented with the 1–2 days of acute-onset lumbar pain, paraparesis, and a T10 sensory level to pin with sphincter dysfunction. The CT of the thoracic and lumbar spine revealed extensive increased density throughout the thoracolumbar spinal canal, consistent with acute hemorrhage. The magnetic resonance imaging confirming the subdural/subarachnoid location of the mostly right-sided hemorrhage (mostly T12-L2) anterior to the spinal cord extending from the L2 up to the T6-7 level. [
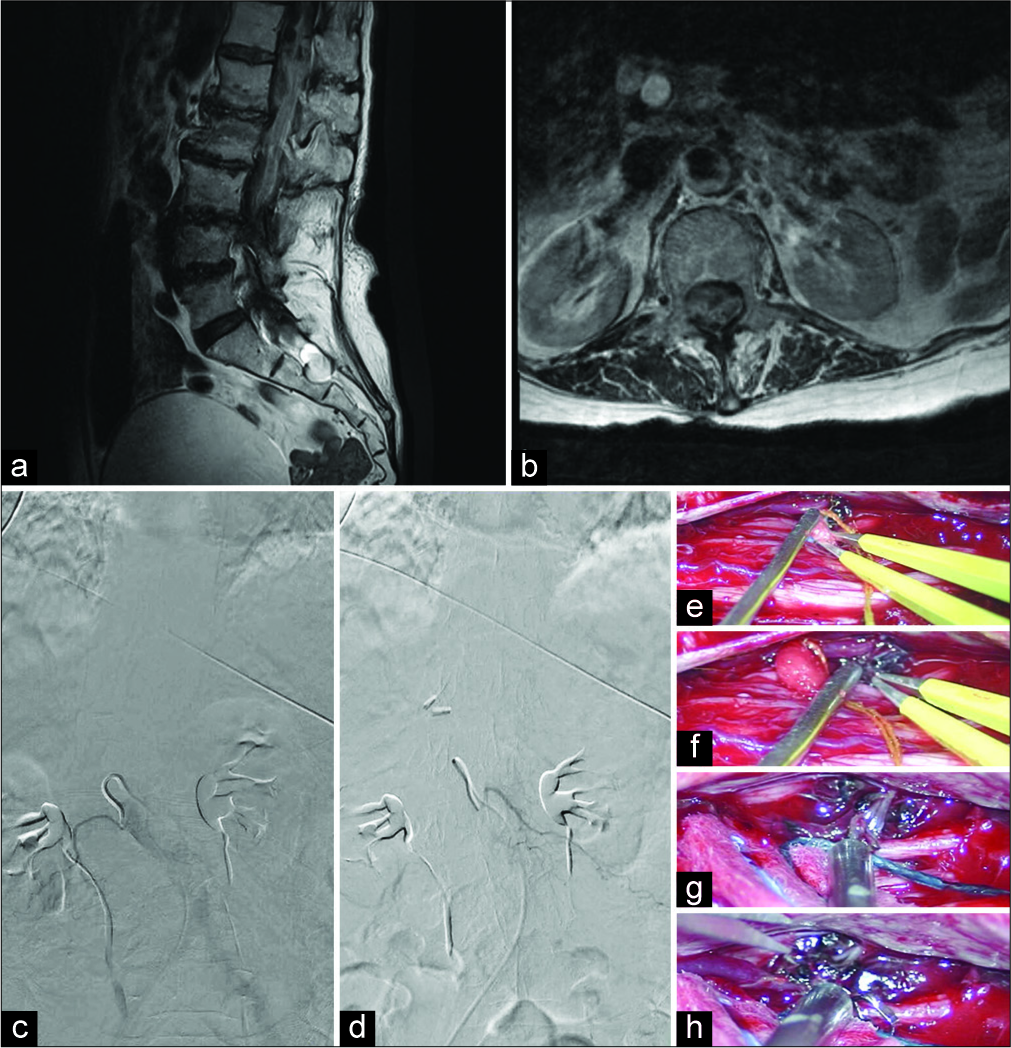
Figure 1:
Lumbar MRI with and without contrast shows mass effect along the right side of the spinal canal from T12 to L2 levels displaces the conus leftward (a). The subcentimeter triangular focus of enhancement at T12-L1 disc can be appreciated (b). The cauda equina shows deformity inferiorly surrounded by blood products in the spinal canal. No typical evidence of flow voids consistent with increased vascularity of spinal SDAVF. Lumbar spine digital subtraction angiography (DSA) shows a contrast injection into the right L1 lumbar segmental artery (c). DSA shows the same for the left L1 lumbar segmental artery (d). There is no evidence of vascular abnormality in any phase of filling or emptying of the radicular artery and vein. Intraoperative images show a radicular artery traveling intradurally and anastomosing with the venous system, as is evident of a spinal fistula (e). Isolated view of SDAVF radicular artery (f). Temporary occlusion of the fistulous artery for extended motor and sensory monitoring for changes (g). The fistulous artery is cauterized and cut (h).
Operation
T11-L1 laminectomies were performed. On opening the dura, a large, cylindrical, and well-organized subdural hematoma was encountered with blood products of varying chronicity these markedly distorted the spinal cord (e.g., right to left compression) [
Postoperative course
The patient tolerated the procedure well and within the first several days experienced improved bilateral lower extremity motor and sensory function along with sphincter improvement. Six months later, she was neurologically intact.
DISCUSSION
While several previous reports have described spinal patients presenting with subarachnoid hemorrhage[
Selective spinal arteriography (SSA) is the gold standard for diagnosis and potential endovascular treatment, providing the ability to define the angioarchitecture of the fistula. Further, SSA allows for the artery of Adamkiewicz to be located to protect it during treatment.
This case highlights an angiographically occult spinal dural AVF presenting with a spinal subdural hematoma. While rare, it is important that clinicians be aware of this potential etiology of subdural hematomas before surgical hematoma evacuation. Although this entity was radiographically occult, angiography should be strongly considered in cases where patients present with spontaneous spinal subdural hematomas. Most critically, operative intervention despite negative vascular studies should be performed to relieve cord compression as well as determine the presence of underlying vascular anomalies is critical to identify occult vascular malformations (e.g., in this case, SDAVF).
CONCLUSION
This case describes a rare presentation of a patient that had angiographically occult dural AVF with a symptomatic spinal subdural hematoma. Nevertheless, if the patient is symptomatic, exploratory surgery may be warranted to remove the subdural hematoma and to identify its source. Surgical planning should include neuromonitoring and use of indocyanine green to localize abnormal vasculature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cenzato M, Versari P, Righi C, Simionato F, Casali C, Giovanelli M. Spinal dural arteriovenous fistulae: Analysis of outcome in relation to pretreatment indicators. Neurosurgery. 2004. 55: 815-22
2. Han PP, Theodore N, Porter RW, Detwiler PW, Lawton MT, Spetzler RF. Subdural hematoma from a Type I spinal arteriovenous malformation. Case report. J Neurosurg. 1999. 90: 255-7
3. Koch C, Gottschalk S, Giese A. Dural arteriovenous fistula of the lumbar spine presenting with subarachnoid hemorrhage. Case report and review of the literature. J Neurosurg. 2004. 100: 385-91
4. Minami M, Hanakita J, Takahashi T, Kitahama Y, Onoue S, Kino T. Spinal dural arteriovenous fistula with hematomyelia caused by intraparenchymal varix of draining vein. Spine J. 2009. 9: e15-9
5. Spetzler RF, Detwiler PW, Riina HA, Porter RW. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002. 96: 145-56
6. Steinmetz MP, Chow MM, Krishnaney AA, Andrews-Hinders D, Benzel EC, Masaryk TJ. Outcome after the treatment of spinal dural arteriovenous fistulae: A contemporary single-institution series and meta-analysis. Neurosurgery. 2004. 55: 77-87