- Department of Neurosurgery, University of Illinois at Chicago, Chicago, Illinois, USA
Correspondence Address:
Sergey Neckrysh
Department of Neurosurgery, University of Illinois at Chicago, Chicago, Illinois, USA
DOI:10.4103/2152-7806.194518
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gerald S. Oh, Hussam Abou-Al-Shaar, Gregory D. Arnone, Ashley L. Barks, Ziad A. Hage, Sergey Neckrysh. Spinal epidural abscess in a patient with piriformis pyomyositis. 21-Nov-2016;7:
How to cite this URL: Gerald S. Oh, Hussam Abou-Al-Shaar, Gregory D. Arnone, Ashley L. Barks, Ziad A. Hage, Sergey Neckrysh. Spinal epidural abscess in a patient with piriformis pyomyositis. 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/spinal-epidural-abscess-in-a-patient-with-piriformis-pyomyositis/
Abstract
Background:Spinal epidural abscess resulting from piriformis pyomyositis is extremely rare. Such condition can result in serious morbidity and mortality if not addressed in a timely manner.
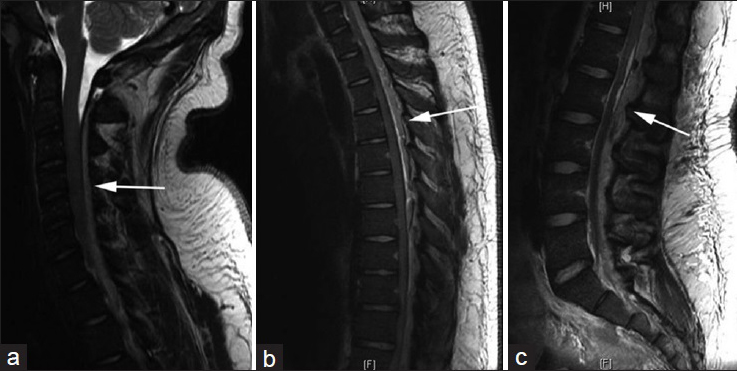
Case Description:The authors describe the case of a 19-year-old male presenting with a 2-week history of fever, low back pain, and nuchal rigidity. When found to have radiographic evidence of a right piriformis pyomyositis, he was transferred to our institution for further evaluation. Because he demonstrated rapid deterioration, cervical, thoracic, and lumbar magnetic resonance imaging scans were emergently performed. They revealed an extensive posterior spinal epidural abscess causing symptomatic spinal cord compression extending from C2 to the sacrum. He underwent emergent decompression and abscess evacuation through a dorsal midline approach. Postoperatively, he markedly improved. Upon discharge, the patient regained 5/5 strength in both upper and lower extremities. Cultures from the epidural abscess grew methicillin-sensitive Staphylococcus aureus warranting a 6-week course of intravenous nafcillin.
Conclusion:A 19-year-old male presented with a holospinal epidural abscess (C2 to sacrum) originating from piriformis pyomyositis. The multilevel cord abscess was emergently decompressed, leading to a marked restoration of neurological function.
Keywords: Piriformis pyomyositis, spinal epidural abscess, surgical decompression
INTRODUCTION
Extensive spinal epidural abscess (SEA) may occur due to direct extension into the epidural space through hematogenous spread, prior spinal procedures, or other etiologies.[
CASE REPORT
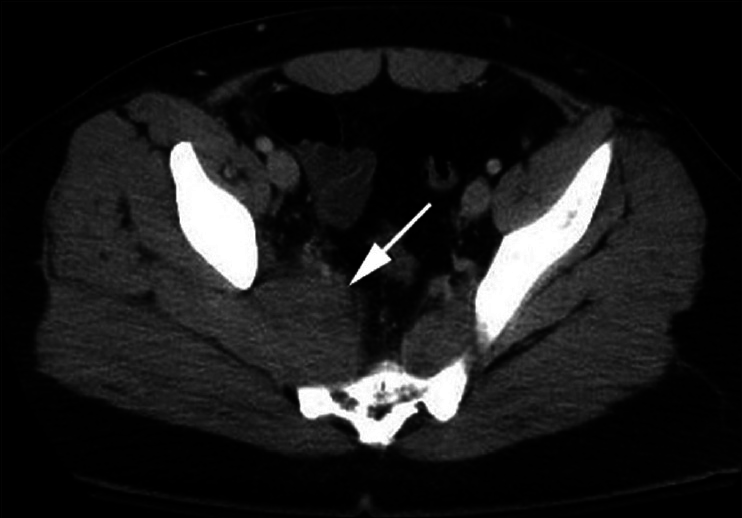
A healthy 19-year-old male with a 2-week history of low back pain, nuchal rigidity, fever, and chills presented to an outside facility. Diagnostic studies revealed a peripheral white blood cell count of 30000, and on computed tomography (CT) of the abdomen/pelvis, an abnormal heterogeneous fluid collection involving the right piriformis muscle was detected [
Figure 2
Sagittal T2-weighted magnetic resonance imaging (MRI) scan depicting spinal epidural abscess compressing the cervical cord posteriorly with blockage of cerebrospinal fluid flow (a). Sagittal T2-weighted MRI scan demonstrating spinal epidural abscess extending down the thoracic (b), and lumbar (c) vertebrae compressing the cord posteriorly
Multiple skip-laminectomies without instrumentation were performed at the C3-7, T11, and L2-4 levels. Cultures were obtained and purulent SEA was washed out at every level and between levels utilizing red rubber catheter that was passed rostrally and caudally in the epidural space; two drains were left in place.
Immediately postoperatively, upper extremity function returned to 4+/5 strength and lower extremity strength to 4/5. Blood cultures and operative wound cultures grew methicillin-sensitive Staphylococcus aureus (MSSA), and he was placed on a long-term nafcillin treatment for a period of 6 weeks. The patient's piriformis abscess did not require drainage and was managed solely with antibiotics. Notably, by postoperative day 10, the patient was neurologically intact with full motor strength in all muscle groups.
DISCUSSION
Location and etiology of spinal epidural abscess
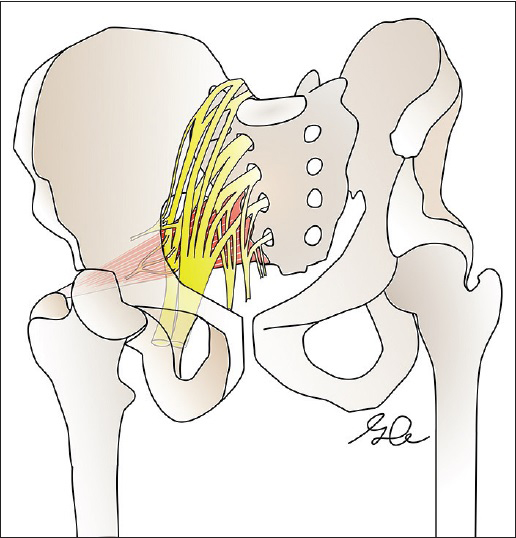
The case uniquely presents a C2-sacrum SEA that originated from a spontaneous piriformis abscess. Pyriformis pyomyositis due to Staphylococcus, Streptococcus, and Brucella spp. occurs particularly in patients with Crohn's disease (i.e., fistula formation) but may also occur spontaneously. In addition, previous case reports have described an association between piriformis pyomyositis and sciatic nerve irritation.[
Treatment options
Although treatment options for SEA can include medical management alone with appropriate antibiotic therapy, those presenting with acute neurological compromise and extensive SEA should undergo early decompression/surgery with/without stabilization.[
CONCLUSION
Extensive SEA due to a piriformis muscle abscess is rare. Prompt surgical decompression for SEA is often indicated to avoid irreversible neurological deficits. In this case, the C2-sacrum SEA was successfully evacuated utilizing multiple skip laminectomies accompanied by posterior epidural catheter irrigation between levels with significant neurologic improvement noted postoperatively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Berkelhammer C, Debre M, Gutti P. Piriformis Muscle Abscess Complicating Crohn's Ileitis. Inflamm Bowel Dis. 2005. 11: 1028-9
2. Burton DJ, Enion D, Shaw DL. Pyomyositis of the piriformis muscle in a juvenile. Ann R Coll Surg Engl. 2005. 87: W9-12
3. Chong KW, Tay BK. Piriformis pyomyositis: A rare cause of sciatica. Singapore Med J. 2004. 45: 229-31
4. Deshmuck VR. Midline trough corpectomies for the evacuation of an extensive ventral cervical and upper thoracic spinal epidural abscess. J Neurosurg Spine. 2010. 13: 229-33
5. Giebaly DE, Horriat S, Sinha A, Mangaleshkar S. Pyomyositis of the piriformis muscle presenting with sciatica in a teenage rugby player. BMJ Case Rep. 2012. pii: bcr1220115392-
6. González-López JJ, Górgolas M, Muñiz J, López-Medrano F, Barnés PR, Fernández Guerrero ML. Spontaneous epidural abscess: Analysis of 15 cases with emphasis on diagnostic and prognostic factors. Eur J Intern Med. 2009. 20: 514-7
7. Kraniotis P, Marangos M, Lekkou A, Romanos O, Solomou E. Brucellosis presenting as piriformis myositis: A case report. J Med Case Rep. 2011. 5: 125-
8. Lam KS, Pande KC, Mehdian H. Surgical decompression: A life-saving procedure for an extensive spinal epidural abscess. Eur Spine J. 1997. 6: 332-5
9. Panagiotopoulos V, Konstantinou D, Solomou E, Panagiotopoulos E, Marangos M, Maraziotis T. Extended cervicolumbar spinal epidural abscess associated with paraparesis successfully decompressed using a minimally invasive technique. Spine. 2004. 29: E300-3
10. Payer M, Walser H. Evacuation of a 14-vertebral-level cervico-thoracic epidural abscess and review of surgical options for extensive spinal epidural abscesses. J Clin Neurosci. 2008. 15: 483-6
11. Pradilla G, Nagahama Y, Spivak A, Bydon A, Rigamonti D. Spinal epidural abscess: Current diagnosis and management. Curr Infect Dis Rep. 2010. 12: 484-91
12. Smoll NR. Variations of the Piriformis and Sciatic Nerve With Clinical Consequence: A Review. Clin Anat. 2010. 23: 8-17
13. Urrutia J, Claudio R. Extensive epidural abscess with surgical treatment and long term follow up. Spine J. 2007. 7: 708-11