- Department of Neurosurgery, University of Rochester, Strong Memorial Hospital, Rochester, United States
- Medical School, Upstate Medical University, Syracuse, United States
- Department of Orthopaedics, University of Rochester, Rochester, New York, United States.
Correspondence Address:
Gabrielle Santangelo, Department of Neurosurgery, University of Rochester, Strong Memorial Hospital, Rochester, United States.
DOI:10.25259/SNI_177_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gabrielle Santangelo1, Prasenjit Saha2, Varun Puvanesarajah3, Emmanuel Menga3, Addisu Mesfin3. Spinal fusion for postlaminectomy kyphosis following intramedullary spinal cord tumor resection: A 34-year follow-up. 07-Apr-2023;14:127
How to cite this URL: Gabrielle Santangelo1, Prasenjit Saha2, Varun Puvanesarajah3, Emmanuel Menga3, Addisu Mesfin3. Spinal fusion for postlaminectomy kyphosis following intramedullary spinal cord tumor resection: A 34-year follow-up. 07-Apr-2023;14:127. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12242
Abstract
Background: Resection of intramedullary spinal cord tumors (IMSCTs) in pediatric patients results in a high incidence of spinal deformity (i.e., kyphoscoliosis often requiring fusion). Here, a 6-year-old male underwent a spinal fusion to correct postlaminectomy thoracic kyphosis following resection of an IMSCT.
Case Description: A 6-year-old male initially underwent multilevel thoracic laminectomies for resection of an IMSCT. Six months later, he presented with the onset of kyphoscoliosis. During adolescence he became increasingly paraparetic due to a thoracic kyphosis that had now progressed to 118°. He underwent a 360 decompression/fusion that included a T1-T9 laminectomy, a T5 to T11 anterior interbody arthrodesis/rib autograft, and posterolateral T2-T12 fusion/iliac crest autograft with Harrington rods placed from T5 to T12. Postoperative radiographs showed the thoracic kyphosis improved to 62°. However, 4.5 years later, X-rays showed the thoracic kyphosis newly progressed to 90° (i.e., from T3 to T12). Thirty-four years after this corrective surgery, he remained neurologically intact with only mild complaints of balance changes, and bladder/bowel urgency while radiographs confirmed continued stability. Further, the thoracic magnetic resonance imaging showed only chronic thoracic spine/cord changes.
Conclusion: A 6-year-old child originally underwent a thoracic laminectomy for an IMSCT. As an adolescent, due to progressive postlaminectomy kyphosis, he underwent a successful secondary thoracic 360° decompression/ fusion. Notably, 34 years later, he did not require any surgical revision.
Keywords: Cerebrospinal fluid, Intramedullary spinal cord tumor, Postlaminectomy kyphosis, Scoliosis, Kyphosis
INTRODUCTION
Intramedullary spinal cord tumors (IMSCTs) make up 2–5% of all primary spinal cord tumors; gliomas accounting for 80% of these lesions.[
CASE REPORT
Initial presentation
A 6-year-old male, diagnosed with a IMSCT, underwent an initial thoracic laminectomy and radiation therapy for partial tumor resection (i.e., “glioma”). Postoperatively, he was fully plegic with a T6 sensory level and thoracic kyphosis from T1 to T12 (45°). By 6.5 years of age, the scoliosis progressed [
Corrective surgery
After traction in a halo in a wheelchair, he underwent an anterior fusion (i.e. a thoracotomy with discectomies and interbody rib graft fusions from T5 to T11). Notably, 39 days later he underwent a circumferential decompression/fusion; T1 to T9 laminectomy/posterolateral T2-T12 fusion with iliac crest autograft, and placement of T5 to T12 Harrington rods (i.e., hooks of placed on the transverse processes of T5 through T7 and T10 through 12 bilaterally). A dural tear at the T6 level was immediately repaired intraoperatively. On postoperative day 8, the patient’s cerebrospinal fluid leak resolved with conservative treatment and he was placed in a halo cast for several months. Postoperative radiographs showed continued improvement after both surgeries [
Postoperative course
Nine months later, (i.e., age 13 years 9 mos.), he developed a wound dehiscence and required removal of the right-sided instrumentation with debridement followed by placement of a Milwaukee brace. At ages 18 and 23, he remained neurologically normal and the thoracic kyphosis had largely stabilized [
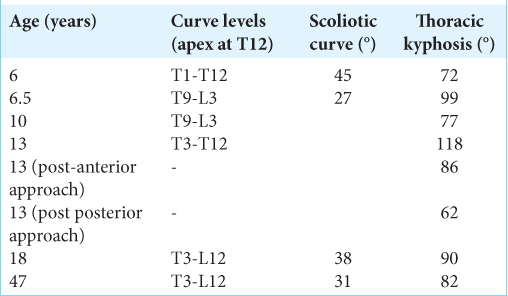
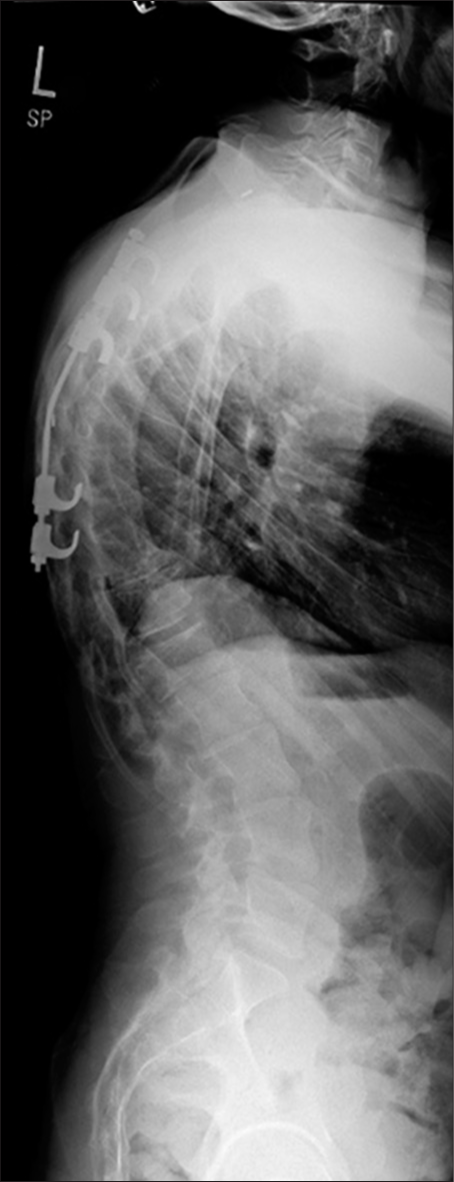
Figure 1:
Standing posteroanterior (left) and lateral (right) scoliosis plain films. There is a right-side scoliotic curve from T8 to L3 (apex at T12) of 31° and thoracic kyphosis from T3 to T12 of 82°. The size of the thoracic vertebral bodies appears small given the size of the lumbar vertebral bodies, and the thorax is proportionally small.
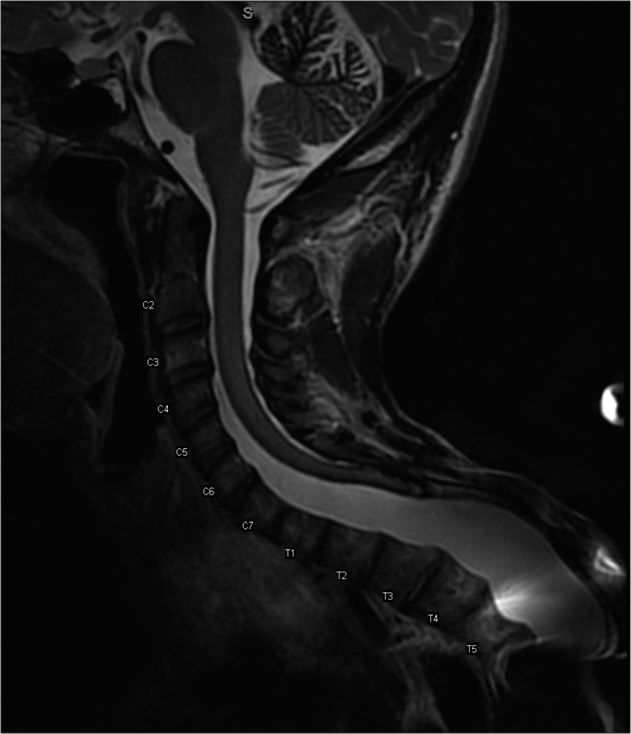
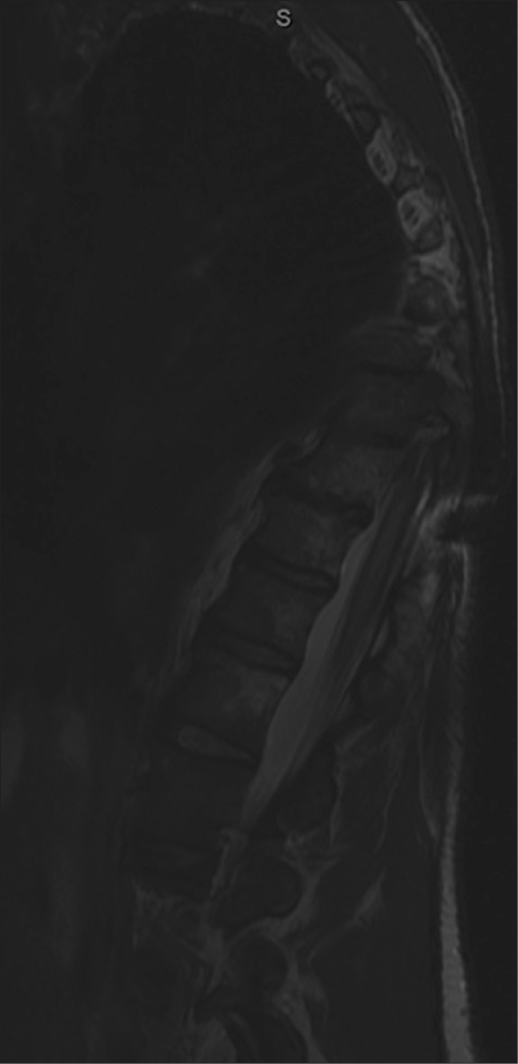
Figure 2:
A T2-weighted sagittal magnetic resonance imaging of cervical and upper thoracic spine demonstrating dural ectasia in the upper thoracic spine associated with an apparent extensive laminectomy defect that begins at T2 and extends distally. The visualized thoracic spinal cord is markedly atretic and adherent to the posterior aspect of the thecal sac. There is considerable artifact from instrumentation at T6.
DISCUSSION
Pediatric surgery for IMSCT
Surgical resection is the mainstay of IMSCT treatment in the pediatric age group [
MSCT resection in the pediatric population
Pediatric patients undergoing initial IMSCT resection for tumor recurrence/progression will typically demonstrate progressive postoperative kyphosis warranting posterolateral fusion. One study evaluated kyphoscoliosis resulting in paraplegia 42 years after a childhood laminectomy for a IMSCT.[
CONCLUSION
A 6-year-old child underwent a thoracic laminectomy for an IMSCT requiring subsequent revision circumferential decompression/fusion. Notably, 34 years later, the patient presented with mild hyperreflexia and did not warrant repeated surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
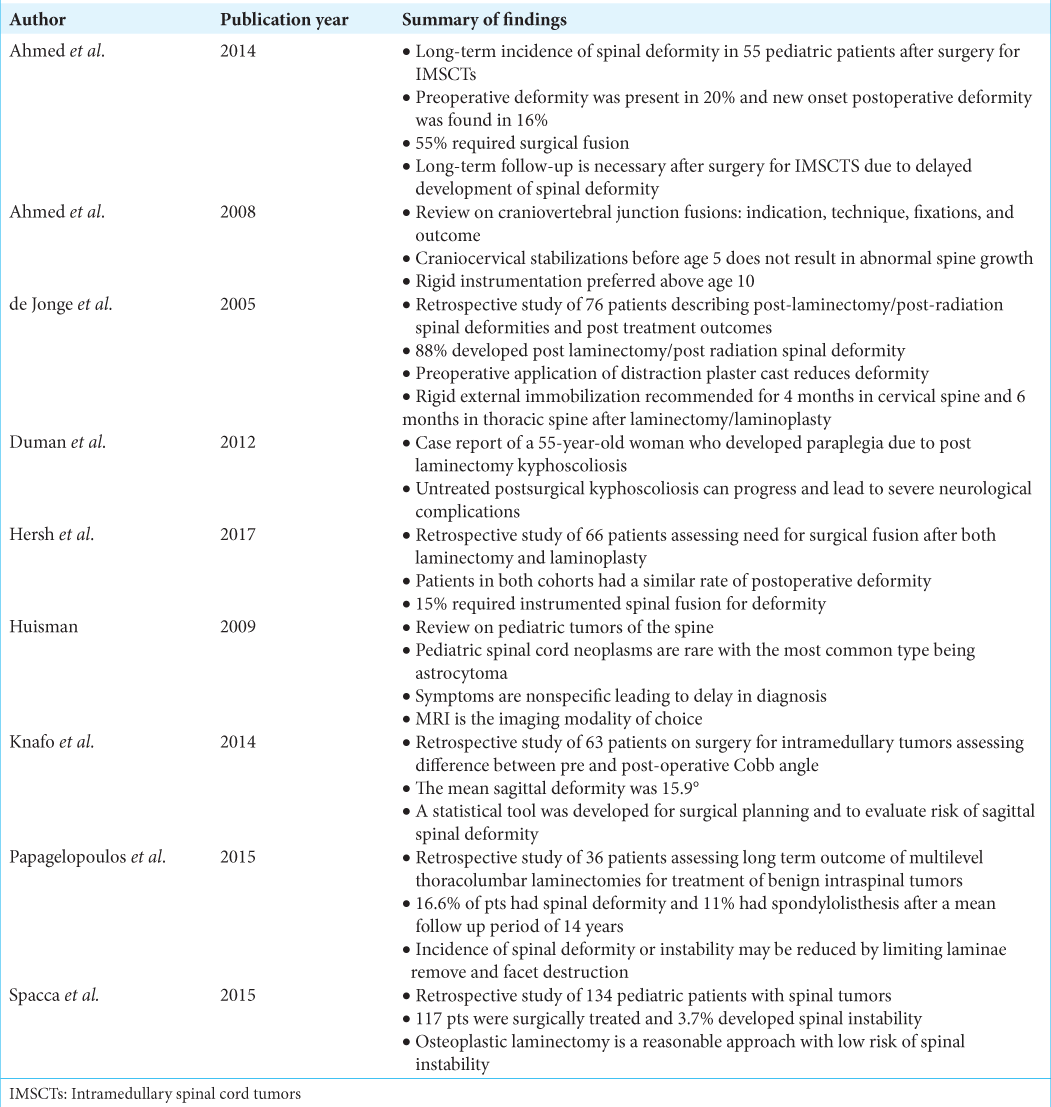
References
1. Ahmed R, Menezes AH, Awe OO, Mahaney KB, Torner JC, Weinstein SL. Long-term incidence and risk factors for development of spinal deformity following resection of pediatric intramedullary spinal cord tumors. J Neurosurg Pediatr. 2014. 13: 613-21
2. Ahmed R, Traynelis VC, Menezes AH. Fusions at the craniovertebral junction. Childs Nerv Syst. 2008. 24: 1209-24
3. de Jonge T, Slullitel H, Dubousset J, Miladi L, Wicart P, Illés T. Late-onset spinal deformities in children treated by laminectomy and radiation therapy for malignant tumours. Eur Spine J. 2005. 14: 765-71
4. Duman I, Guzelkucuk U, Yilmaz B, Tan AK. Post-laminectomy rotokyphoscoliosis causing paraplegia in long term: Case report. J Spinal Cord Med. 2012. 35: 175-7
5. Hersh DS, Iyer RR, Garzon-Muvdi T, Liu A, Jallo GI, Groves ML. Instrumented fusion for spinal deformity after laminectomy or laminoplasty for resection of intramedullary spinal cord tumors in pediatric patients. Neurosurg Focus. 2017. 43: E12
6. Huisman TA. Pediatric tumors of the spine. Cancer Imaging. 2009. 9: S45-8
7. Kelley BJ, Johnson MH, Vortmeyer AO, Smith BG, Abbed KM. Two-level thoracic pedicle subtraction osteotomy for progressive post-laminectomy kyphotic deformity following resection of an unusual thoracolumbar intradural extramedullary tumor. J Neurosurg Pediatr. 2012. 10: 334-9
8. Knafo S, Court C, Parker F. Predicting sagittal deformity after surgery for intramedullary tumors. J Neurosurg Spine. 2014. 21: 342-7
9. Papagelopoulos PJ, Peterson HA, Ebersold MJ, Emmanuel PR, Choudhury SN, Quast LM. Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults. Spine (Phila Pa 1976). 1997. 22: 442-51
10. Spacca B, Giordano F, Donati P, Genitori L. Spinal tumors in children: Long-term retrospective evaluation of a series of 134 cases treated in a single unit of pediatric neurosurgery. Spine J. 2015. 15: 1949-55
11. Tobin MK, Geraghty JR, Engelhard HH, Linninger AA, Mehta AI. Intramedullary spinal cord tumors: A review of current and future treatment strategies. Neurosurg Focus. 2015. 39: E14