- Department of Medicine, Catanduva Medical School (FAMECA-UNIFIPA), Catanduva, São Paulo, Brazil.
- Department of Medicine, Pontifical Catholic University of Goiás, Goiânia, Brazil.
- Department of Medicine, Faculty of Medicine of ABC, Santo André, São Paulo, Brazil.
- Department of Medicine, School of Medicine of Pontifical Catholic University of São Paulo, Sorocaba, São Paulo, Brazil.
- Department of Neurosurgery, Santa Paula Hospital, São Paulo, Brazil.
- Department of Pathology, DASA, São Paulo, Brazil.
- Department of Neurology and Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil.
- Department of Medicine, Division of Neurology, Catholic Pontifical University of São Paulo, Sorocaba, São Paulo, Brazil.
DOI:10.25259/SNI_435_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paulo Eduardo Albuquerque Zito Raffa1, Rafael Caiado Caixeta Vencio2, Andre Costa Corral Ponce3, Bruno Pricoli Malamud3, Isabela Caiado Vencio4, Cesar Cozar Pacheco5, Felipe D’Almeida Costa6, Paulo Roberto Franceschini7, Roger Thomaz Rotta Medeiros5, Paulo Henrique Pires Aguiar8. Spinal intramedullary abscess due to Candida albicans in an immunocompetent patient: A rare case report. 14-Jun-2021;12:275
How to cite this URL: Paulo Eduardo Albuquerque Zito Raffa1, Rafael Caiado Caixeta Vencio2, Andre Costa Corral Ponce3, Bruno Pricoli Malamud3, Isabela Caiado Vencio4, Cesar Cozar Pacheco5, Felipe D’Almeida Costa6, Paulo Roberto Franceschini7, Roger Thomaz Rotta Medeiros5, Paulo Henrique Pires Aguiar8. Spinal intramedullary abscess due to Candida albicans in an immunocompetent patient: A rare case report. 14-Jun-2021;12:275. Available from: https://surgicalneurologyint.com/surgicalint-articles/10892/
Abstract
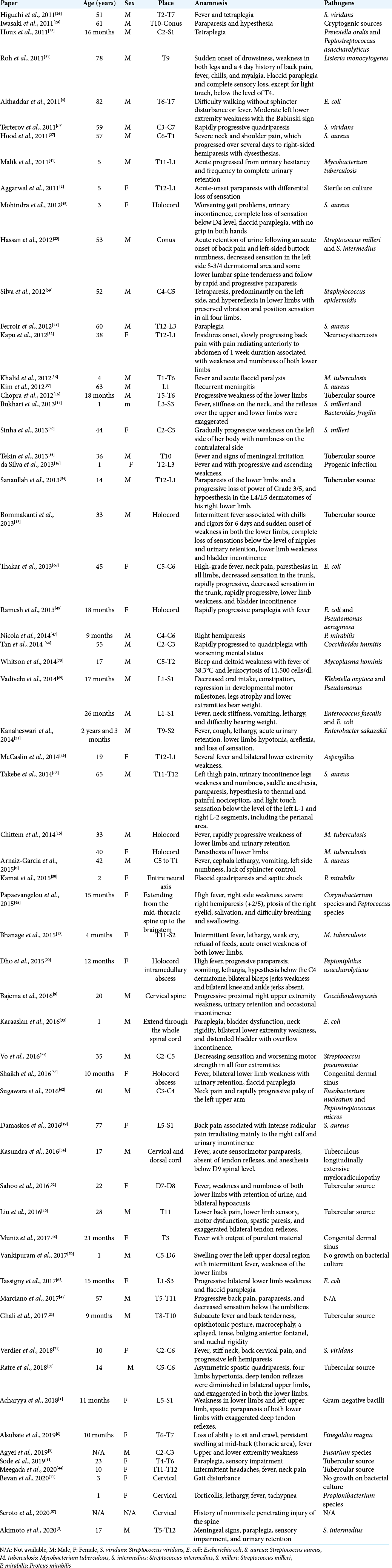
Background: A spinal intramedullary abscess is a rare clinical entity in which patients classically present with a subacute myelopathy and progressive paraplegia, sensory deficits, and/or bowel and bladder dysfunction. We report the second case of spinal intramedullary abscess caused by Candida albicans to ever be published and the first case of its kind to be surgically managed.
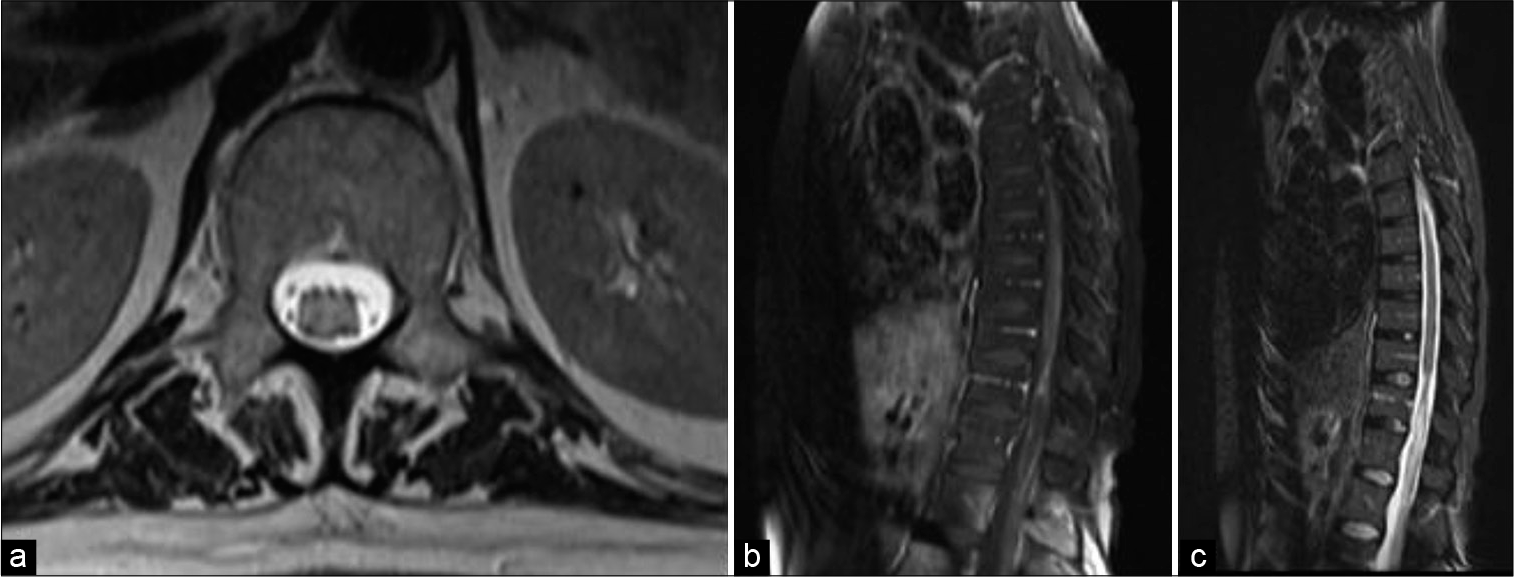
Case Description: A 44-year-old female presented with severe lumbar pain associated with paraparesis, incontinence, and paraplegia. She reported multiple hospital admissions and had a history of seizures, having already undergone treatment for neurotuberculosis and fungal infection of the central nervous system unsuccessfully. Nevertheless, no laboratory evidence of immunosuppression was identified on further investigation. Magnetic resonance imaging showed a D10-D11, well-circumscribed, intramedullary mass within the conus, which was hypointense on T1-weighted imaging and hyperintense on T2/STIR weighted. The patient underwent surgery for removal and biopsy of the lesion, which provided the diagnosis of an intramedullary abscess caused by C. albicans, a very rare condition with only one case reported in literature so far.
Conclusion: C. albicans intramedullary abscess is a very rare clinical entity, especially in immunocompetent patients. We highlight C. albicans as an important etiology that must be considered in differential diagnosis. Critical evaluation of every case, early diagnosis, timely referral and surgical management of the abscess is essential to improve neurological outcome.
Keywords: Abscess, Candida albicans, Central nervous system, Conus medullaris, Intramedullary
INTRODUCTION
Involvement of the central nervous system (CNS) by Candida sp. usually leads to meningitis and cerebral microabscesses, especially in immunocompromised individuals or when anatomic barriers are breached by surgery or implanted devices.[
CASE REPORT
A 44-year-old female patient sought the neurosurgery service at Hospital Santa Paula with a complaint of lower back pain associated with paraparesis for 2 years with progressive worsening of the condition between crises. She reported development of paraplegia in the past year.
In an investigation of multiple hospital admissions, she previously underwent treatment for CNS fungal infection and neurotuberculosis in late 2020 with amphotericin B (for 6 weeks) followed by voriconazole (for 4 weeks) with an ineffective result. The cerebrospinal fluid (CSF) contained 43 cells (75% lymphocytes, monocytes 22%, macrophages 3%), protein 175 mg/dL; glucose 26 mg/dL; lactic acid 42 mg/dL; lactate dehydrogenase 30 U/L; adenosinedeaminase 6.2 U/L; gamma globulin 31.62%; microbiology negative; antibodies for syphilis, Borrelia burgdorferi, toxoplasmosis, cytomegalovirus (CMV), herpes simplex 1 and 2, herpes zoster, cysticercosis, human immunodeficiency virus (HIV), and human T-lymphotropic virus were not reactive; no cancerous cells were identified. She also presented a history of seizures and meningitis.
On neurological examination, the patient presented with dysarthria, horizontal nystagmus with preservation of extrinsic eye movement, Grade III strength in upper limbs with wrist spasticity, plegia in lower limbs, and anesthesia from the T12 level without proprioception. She also presented with bicipital, tricipital, and styloradial hyperreflexia in upper limbs, with bilateral exaltation points and positive Hoffmann’s sign, besides patellar and aquilean areflexia, and negative Babinski’s sign.
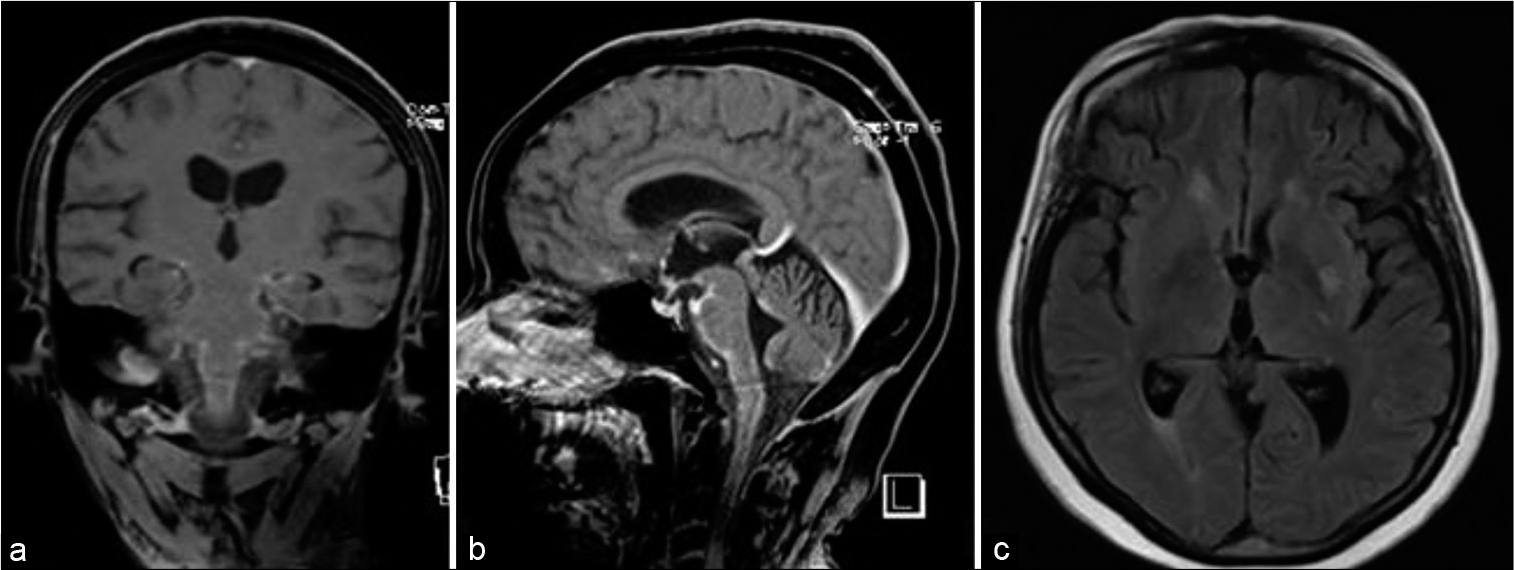
For better evaluation, magnetic resonance imaging (MRI) images of the brain and spine were requested. Brain MRI showed thickening and leptomeningeal impregnation by gadolinium compromising both lateral fissures, insula, and frontotemporal operculum, evidencing diffuse pachymeningitis [
Figure 1:
Preoperative magnetic resonance imaging. (a) Coronal gadolinium-enhanced image, (b) sagittal gadolinium-enhanced image, (c) axial T2/FLAIR-weighted image showing a slight reduction in the thickness of the leptomeningeal impregnation of the lateral fissures and frontotemporal operculum on both sides suggestive of diffuse pachymeningitis.
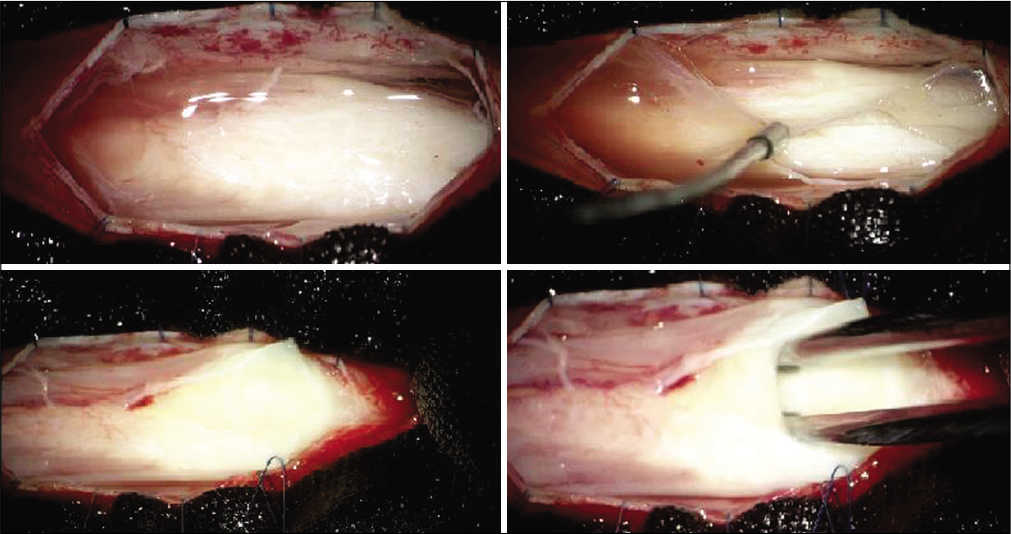
From the imaging findings and their relationship with the clinic, the patient underwent surgery and biopsy of the lesion. A T10-T11 laminectomy was performed and, after straight opening of the dura mater, a whitish lesion was found in the intramedullary region, suggestive of an abscess, being, therefore, drained and biopsied for analysis [
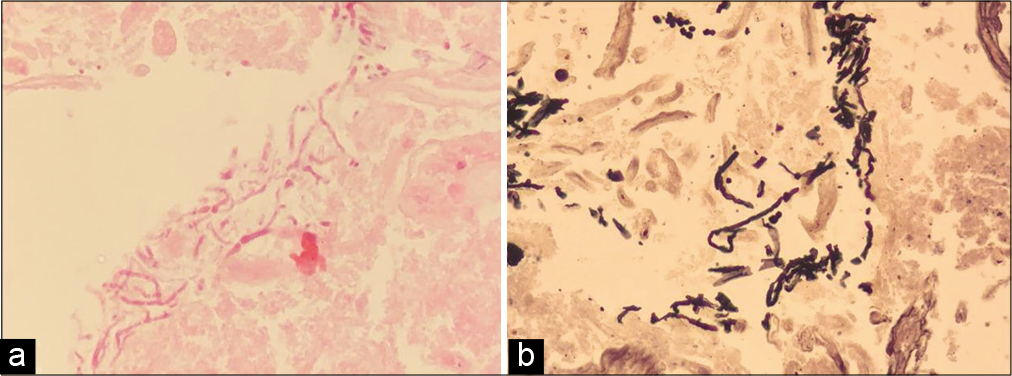
The culture of the surgical specimen tested positive for C. albicans and the histopathological evaluation of the lesion revealed extensive fibrinoid material and presence of hyaline septate pseudohyphae and fungal spores, with strong impregnation by Grocott methenamine silver stain [
DISCUSSION
Candida spp. are considered opportunistic commensal pathogens that promote infection under host predisposing conditions.[
There are a wide array of infectious causes of intramedullary myelitis, most of them caused by B. burgdorferi, Treponema pallidum, Mycobacterium tuberculosis, HIV, herpes simplex virus, varicella-zoster virus, CMV, Epstein-Barr virus), rabies, and schistosomiasis.[
C. albicans spinal infection still configures a challenging diagnostic. MRI is useful in diagnosing medullary abscesses, but those infections may mimic a neoplastic process as myxopapillary ependymoma or leptomeningeal carcinomatosis.[
CONCLUSION
C. albicans intramedullary abscess represents a very rare clinical entity, especially in immunocompetent patients. It must, however, be considered as an important etiology for spinal intramedullary abscesses and as a differential diagnosis in intramedullary pathologies. Critical evaluation of every case, early diagnosis, timely referral and surgical management of the abscess is essential to improve neurological outcome.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Acharyya S, Chakravarty S. Congenital dermal sinus with extensive intramedullary expansion and an infected spinal epidermoid cyst in an infant. J Family Med Prim Care. 2018. 7: 1103-5
2. Aggarwal M, Aggarwal KC, Karamchand L, Aggarwal A. Intramedullary spinal cord abscess masquerading as spinal tumor. Indian Pediatr. 2011. 48: 973-4
3. Agyei JO, Qiu J, Fabiano AJ. Fusarium species intramedullary spinal cord fungus ball: Case report. J Neurosurg Spine. 2019. 31: 440-6
4. Akhaddar A, Boulahroud O, Boucetta M. Chronic spinal cord abscess in an elderly patient. Surg Infect (Larchmt). 2011. 12: 333-4
5. Akimoto T, Hirose S, Mizoguchi T, Yokota Y, Hara M, Ishihara M. Ruptured long intramedullary spinal cord abscess successfully treated with antibiotic treatment. J Clin Neurosci. 2020. 82: 249-51
6. Alsubaie S, Dolgum S, Binkhamis K, Alweijri I, Bugshan A, Alzamil F. Finegoldia magna causing intramedullary thoracic spinal cord abscess in an infant. Anaerobe. 2019. 56: 57-60
7. Argersinger DP, Natkha VP, Shepard MJ, Thomas AA, Oler AJ, Williamson PR, Chittiboina P, Heiss JD. Intradural cauda equina Candida abscess presenting with hydrocephalus: Case report. J Neurosurg Spine. 2019. p. 1-4
8. Arnáiz-García ME, González-Santos JM, López-Rodriguez J, Dalmau-Sorli MJ, Bueno-Codoñer M, Arévalo-Abascal A. Intramedullary cervical abscess in the setting of aortic valve endocarditis. Asian Cardiovasc Thorac Ann. 2015. 23: 64-6
9. Bajema KL, Dalesandro MF, Fredricks DN, Ramchandani M. Disseminated coccidioidomycosis presenting with intramedullary spinal cord abscesses: Management challenges. Med Mycol Case Rep. 2016. 15: 1-4
10. Bakhsheshian J, Kim PE, Attenello FJ. Intramedullary cervical spinal cord abscess. World Neurosurg. 2017. 106: 1049.e1-2
11. Bevan R, Leach P. Infected congenital cervical dermal sinuses leading to spinal cord abscess: Two case reports and a review of the literature. Childs Nerv Syst. 2021. 37: 225-8
12. Bhanage A, Katkar A, Ghate P, Ratta B. Intra-medullary tubercular abscess with spinal dysraphism: An unusual case. J Pediatr Neurosci. 2015. 10: 73-5
13. Bommakanti K, Alugolu R, Chittem LR, Patil M, Purohit AK. Fulminant holocord intramedullary tubercular abscess with enigmatic presentation. Surg Neurol Int. 2013. 4: 32
14. Bukhari EE, Alotibi FE. Fatal Streptococcus melleri meningitis complicating missed infected intramedullary dermoid cyst secondary to dermal sinus in a Saudi child. J Trop Pediatr. 2013. 59: 246-9
15. Chittem L, Bommanakanti K, Alugolu R. Precipitation sign: A new radiological sign for spinal intramedullary tubercular abscess. Spinal Cord. 2014. 52: S1-2
16. Chopra A, Patra B, Aneja S, Mukherjee S, Maheswari A, Seth A. Spinal congenital dermal sinus presenting as a diagnostic conundrum. Pediatr Neurosurg. 2012. 48: 187-90
17. Crane JK. Intrathecal spinal abscesses due to Candida albicans in an immunocompetent man. BMJ Case Rep 2018. 2018. p. bcr-2017-223326
18. da Silva PS, de Souza Loduca RD. Intramedullary spinal cord abscess as complication of lumbar puncture: A case-based update. Childs Nerv Syst. 2013. 29: 1061-8
19. Damaskos D, Jumeau H, Lens FX, Lechien P. Intramedullary abscess by Staphylococcus aureus presenting as cauda equina syndrome to the emergency department. Case Rep Emerg Med. 2016. 2016: 9546827
20. Dho YS, Kim SK, Wang KC, Phi JH. Catastrophic intramedullary abscess caused by a missed congenital dermal sinus. J Korean Neurosurg Soc. 2015. 57: 225-8
21. Ferroir JP, Lescure FX, Giannesini C, Elghozi D, Marro B. Paraplégie flasque due à des abcès intramédullaires et épiduraux à staphylocoques dorés. Méningite et spondylodiscite associées [Paraplegia associated with intramedullary spinal cord and epidural abcesses, meningitis and spondylodiscitis (Staphylococcus aureus)]. Rev Neurol (Paris). 2012. 168: 868-72
22. Flanagan EP, Pittock SJ. Diagnosis and management of spinal cord emergencies. Handb Clin Neurol. 2017. 140: 319-35
23. Gavino C, Hamel N, Zeng JB, Legault C, Guiot MC, Chankowsky J. Impaired RASGRF1/ERK-mediated GMCSF response characterizes CARD9 deficiency in French-Canadians. J Allergy Clin Immunol. 2016. 137: 1178-88.e7
24. Ghali MG, Srinivasan VM, Kim MJ, Malik A. Spinal intramedullary tuberculosis with concurrent supra-and infratentorial intracranial disease in a 9-month-old boy: Case report and comprehensive review of the literature. World Neurosurg. 2017. 106: 37-45
25. Hassan MF, Mohamed MB, Kalsi P, Sinar EJ, Bradey N. Intramedullary pyogenic abscess in the conus medullaris. Br J Neurosurg. 2012. 26: 118-9
26. Higuchi K, Ishihara H, Okuda S, Kanda F. A 51-year-old man with intramedullary spinal cord abscess having a patent foramen ovale. BMJ Case Rep. 2011. 2011: bcr1120103512
27. Hood B, Wolfe SQ, Trivedi RA, Rajadhyaksha C, Green B. Intramedullary abscess of the cervical spinal cord in an otherwise healthy man. World Neurosurg. 2011. 76: 361.e15-9
28. Houx L, Brochard S, Peudenier S, Dam Hieu P, Rémy-Néris O. Recovery after tetraplegia caused by dermal sinus infection: Intramedullary abscess and tetraparesis. Pediatr Neurol. 2011. 44: 229-32
29. Iwasaki M, Yano S, Aoyama T, Hida K, Iwasaki Y. Acute onset intramedullary spinal cord abscess with spinal artery occlusion: A case report and review. Eur Spine J. 2011. 20: S294-301
30. Kamat AS, Thango NS, Husein MB. Proteus mirabilis abscess involving the entire neural axis. J Clin Neurosci. 2016. 30: 127-9
31. Kanaheswari Y, Lai C, Raja Lope RJ, Azizi AB, Zulfiqar MA. Intramedullary spinal cord abscess: The result of a missed congenital dermal sinus. J Paediatr Child Health. 2015. 51: 223-5
32. Kapu R, Singh MK, Pande A, Vasudevan MC, Ramamurthi R. Intradural extramedullary cysticercal abscess of spine. Trop Parasitol. 2012. 2: 131-4
33. Karaaslan B, Ülkü G, Ucar M, Demirdağ TB, İnan A, Börcek AÖ. Intramedullary dermoid cyst infection mimicking holocord tumor: Should radical resection be mandatory? -A case report. Childs Nerv Syst. 2016. 32: 2249-53
34. Kasundra GM, Sood I, Bhushan B, Bhargava AN, Shubhkaran K. Distal cord-predominant longitudinally extensive myelitis with diffuse spinal meningitis and dural abscesses due to occult tuberculosis: A rare occurrence. J Pediatr Neurosci. 2016. 11: 77-9
35. Kawakami N, Mimatsu K, Kato F, Sato K, Matsuyama Y. Intraoperative ultrasonographic evaluation of the spinal cord in cervical myelopathy. Spine (Phila Pa 1976). 1994. 19: 34-41
36. Khalid M, Khalid S, Mittal S, Ahmad U. Intramedullary tubercular abscess with syrinx formation. J Pediatr Neurosci. 2012. 7: 61-3
37. Kim MS, Ju CI, Kim SW, Lee HY. Recurrent bacterial meningitis accompanied by a spinal intramedullary abscess. J Korean Neurosurg Soc. 2012. 51: 380-2
38. Kumar S, Kaza RC, Tandon A, Nayar M. Subdural spinal fungal granuloma due to Candida tropicalis. Case report. J Neurosurg. 1979. 50: 395-6
39. Lindner A, Becker G, Warmuth-Metz M, Schalke BC, Bogdahn U, Toyka KV. Magnetic resonance image findings of spinal intramedullary abscess caused by Candida albicans Case report. Neurosurgery. 1995. 36: 411-2
40. Liu J, Zhang H, He B, Wang B, Niu X, Hao D. Intramedullary tuberculoma combined with abscess: Case report and literature review. World Neurosurg. 2016. 89: 726.e1-4
41. Malik N, Behari S, Ansari MS, Jaiswal AK, Gupta P, Jain M. An intramedullary tuberculous abscess of the conus in a 5-year-old child presenting with urinary dysfunction. World Neurosurg. 2011. 76: 592.e15-8
42. Marciano R, Ahammad Z, Awuor V. Thoracic spinal cord glioblastoma mimicking epidural abscess: Case report and literature review. Cureus. 2017. 9: e1631
43. McCaslin AF, Lall RR, Wong AP, Lall RR, Sugrue PA, Koski TR. Thoracic spinal cord intramedullary aspergillus invasion and abscess. J Clin Neurosci. 2015. 22: 404-6
44. Meegada S, Gyamfi R, Muppidi V, Dandu V, Challa T. Multiple intracranial tuberculomas with an intra-medullary spinal cord tuberculoma in a pediatric patient. Cureus. 2020. 12: e7248
45. Mohindra S, Sodhi HS, Aggarwal A. Management problems of intramedullary holocord abscess: An illustration in a pediatric case. Childs Nerv Syst. 2012. 28: 637-40
46. Muniz BC, Ribeiro BN, Mufarrej G, Wilner NV, Gasparetto EL. Cervical spinal dermal sinus associated with intramedullary spinal cord abscess. Arq Neuropsiquiatr. 2017. 75: 133
47. Nicola Z, Antonio C, De Tommasi A. Cervical dermal sinus complicated with intramedullary abscess in a child: Case report and review of literature. Eur Spine J. 2014. 23: 192-6
48. Papaevangelou G, Tsitsopoulos PP, Flaris N, Iliadis C, Tsonidis C. Dermal sinus tract of the thoracic spine presenting with intramedullary abscess and cranial nerve deficits. Pediatr Neurosurg. 2015. 50: 339-43
49. Ramesh VG, Karthikeyan KV, Kitchanan S, Sriraman B. Holocord abscess in association with congenital dermal sinus. J Pediatr Neurosci. 2013. 8: 198-200
50. Ratre S, Choudhary S, Yadav Y, Parihar V, Bajaj J, Pateriya A. Concurrent intramedullary and intracranial tuberculomass. J Assoc Physicians India. 2018. 66: 72-4
51. Roh JE, Lee SY, Cha SH, Cho BS, Jeon MH, Kang MH. Sequential magnetic resonance imaging finding of intramedullary spinal cord abscess including diffusion weighted image: A case report. Korean J Radiol. 2011. 12: 241-6
52. Sahoo L, Mallick AK, Mohanty G, Swain KP, Nayak S, Sahu AK. Concurrent intramedullary spinal cord and multiple intracranial tuberculomas with tuberculous optic neuritis: A rare case report. Indian J Tuberc. 2017. 64: 337-40
53. Sakayama K, Kidani T, Matsuda Y, Fujibuchi T, Miyazaki T, Takada K. Subdural spinal granuloma resulting from Candida albicans without immunosufficiency: Case report. Spine (Phila Pa 1976). 2002. 27: E356-60
54. Sanaullah M, Mumtaz S, Memon AA, Hashim AS, Bashir S. Intramedullary dermoid cyst with relatively atypical symptoms: A case report and review of the literature. J Med Case Rep. 2013. 7: 104
55. Sanches MD, Mimura LA, Oliveira LR, Ishikawa LL, Garces HG, Bagagli E. Differential behavior of nonalbicans Candida species in the central nervous system of immunocompetent and immunosuppressed mice. Front Microbiol. 2019. 9: 2968
56. Sánchez-Portocarrero J, Pérez-Cecilia E, Corral O, RomeroVivas J, Picazo JJ. The central nervous system and infection by Candida species. Diagn Microbiol Infect Dis. 2000. 37: 169-79
57. Seroto PM, Harrington BM, Lombard C, Vlok AJ. The role of tertiary neurosurgical intervention in non-missile penetrating injuries of the spine. Eur Spine J. 2020. p.
58. Shaikh S, Joshi R. Pyomyelia presenting as acute flaccid paralysis. Oxf Med Case Reports. 2016. 2016: omw052
59. Silva RT, Souza HC, de Amoreira Gepp R, Batista GR, Horan TA, Oliveira PC. Penetrating cervical spine injury and spinal cord intramedullary abscess. Arq Neuropsiquiatr. 2012. 70: 308-9
60. Sinha P, Parekh T, Pal D. Intramedullary abscess of the upper cervical spinal cord. Unusual presentation and dilemmas of management: Case report. Clin Neurol Neurosurg. 2013. 115: 1845-50
61. Sode HC, Ibrahim A, Beranger HS, Soong-Meenga NH, Aminath K, Samuila S. Abcès pottique intra médullaire: À propos d’un cas [Intramedullary Pott’s abscess: A case study]. Pan Afr Med J. 2019. 34: 186
62. Sugawara A, Ishigaki D, Isu T, Ogasawara K. Intramedullary abscess of the cervical spinal cord caused by advanced periodontitis: Case report. No Shinkei Geka. 2016. 44: 685-9
63. Takebe N, Iwasaki K, Hashikata H, Toda H. Intramedullary spinal cord abscess and subsequent granuloma formation: A rare complication of vertebral osteomyelitis detected by diffusion-weighted magnetic resonance imaging. Neurosurg Focus. 2014. 37: E12
64. Tan LA, Kasliwal MK, Nag S, O’Toole JE, Traynelis VC. Rapidly progressive quadriparesis heralding disseminated coccidioidomycosis in an immunocompetent patient. J Clin Neurosci. 2014. 21: 1049-51
65. Tassigny D, Fomekong E, Koerts G, Raftopoulos C. Intramedullary holocord abscess secondary to infected dermoid cyst. Acta Neurochir (Wien). 2018. 160: 209-12
66. Tekin R, Kaçar E, Çevik FC, Çinar K, Çevik R. Intracranial and intramedullary tuberculoma with intravertebral abscess manifestation under anti-tuberculous treatment: A case report. Clin Neurol Neurosurg. 2013. 115: 1858-60
67. Terterov S, Taghva A, Khalessi AA, Kim PE, Liu C. Intramedullary abscess of the spinal cord in the setting of patent foramen ovale. World Neurosurg. 2011. 76: 361.e11-4
68. Thakar S, Rao A, Mohan D, Hegde A. Metachronous occurrence of an intramedullary abscess following radical excision of a cervical intramedullary pilocytic astrocytoma. Neurol India. 2013. 61: 322-4
69. Vadivelu S, Desai SK, Illner A, Luerssen TG, Jea A. Infected lumbar dermoid cyst mimicking intramedullary spinal cord tumor: Observations and outcomes. J Pediatr Neurosci. 2014. 9: 21-6
70. Vankipuram S, Sahoo SK, Srivastava C, Ojha BK. Spinal cord abscess secondary to infected dorsal dermal sinus in an infant: Uncommon presentation of a known entity. BMJ Case Rep. 2017. 2017: bcr2017222366
71. Verdier EP, Konsol O, Portillo S. Intramedullary cervical abscess mimicking a spinal cord tumor in a 10-year-old girl: A case-based review. Childs Nerv Syst. 2018. 34: 2143-7
72. Vo DT, Cravens GF, Germann RE. Streptococcus pneumoniae meningitis complicated by an intramedullary abscess: A case report and review of the literature. J Med Case Rep. 2016. 10: 290
73. Whitson WJ, Ball PA, Lollis SS, Balkman JD, Bauer DF. Postoperative Mycoplasma hominis infections after neurosurgical intervention. J Neurosurg Pediatr. 2014. 14: 212-8