- Department of Neurosurgery, Ibn Sina Hospital, Kuwait.
Correspondence Address:
Faisal T. Sayer, Department of Neurosurgery, Ibn Sina Hospital, Kuwait.
DOI:10.25259/SNI_100_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Faisal T. Sayer, Abdulrahman Khalaf Alanezi, Salem Nabil Zaidan. Spontaneous chronic subdural hematoma associated with arachnoid cyst in a child: A case report and critical review of the literature. 15-Apr-2022;13:156
How to cite this URL: Faisal T. Sayer, Abdulrahman Khalaf Alanezi, Salem Nabil Zaidan. Spontaneous chronic subdural hematoma associated with arachnoid cyst in a child: A case report and critical review of the literature. 15-Apr-2022;13:156. Available from: https://surgicalneurologyint.com/surgicalint-articles/11527/
Abstract
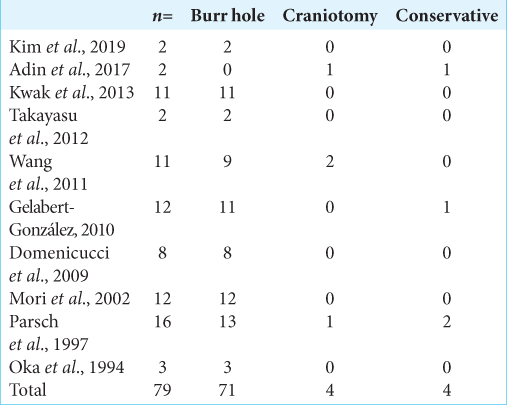
Background: Arachnoid cysts (ACs) are benign, congenital, fluid-filled collection between two layers of the arachnoid membrane accounting for about 1% of all the intracranial space occupying lesions. These lesions are usually asymptomatic and detected incidentally by magnetic resonance imaging (MRI) or computed tomography scan imaging (CT). However, these lesions can present as spontaneous chronic subdural hematoma (CSDH) causing neurological deficits that require neurosurgical intervention.
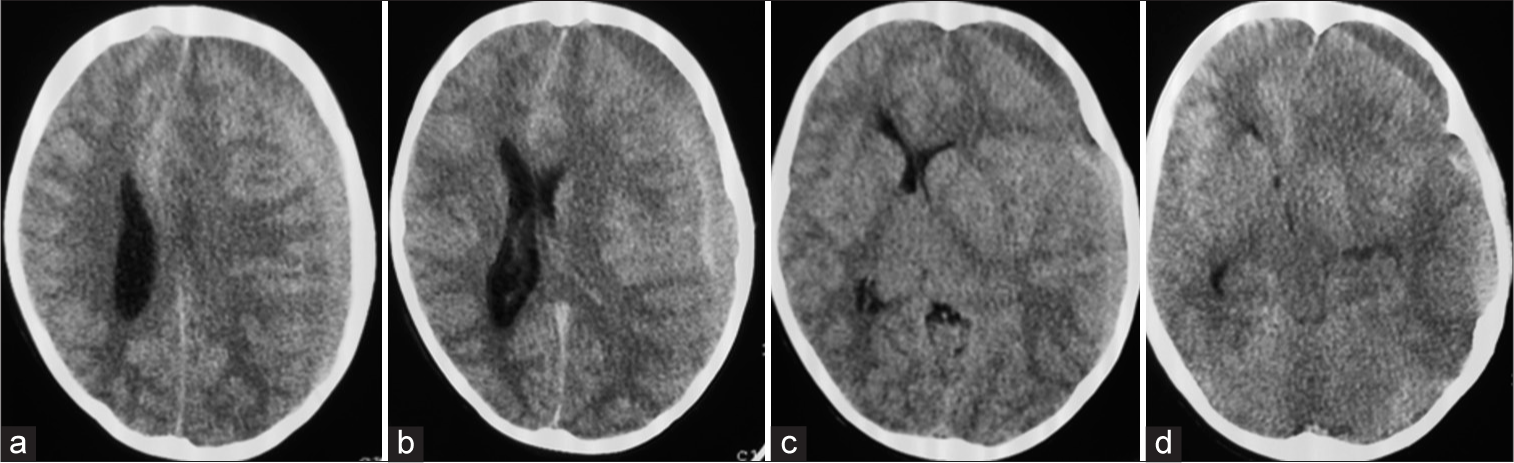
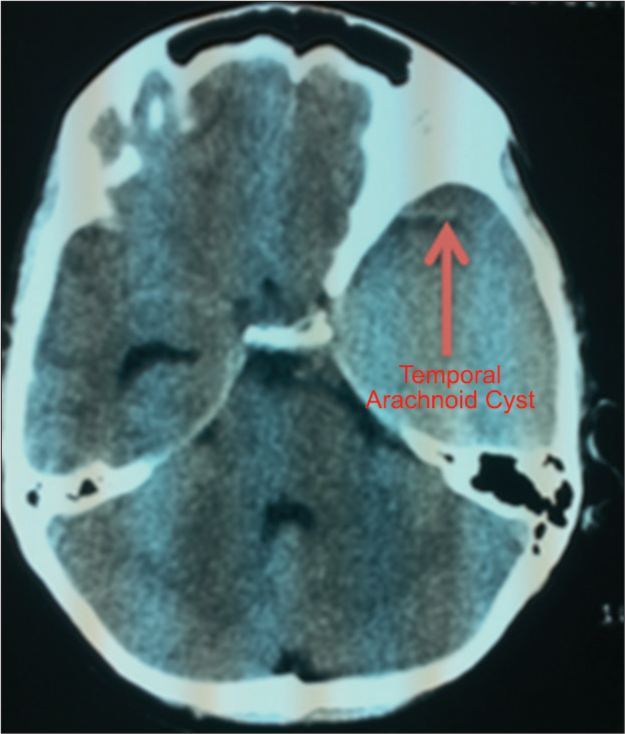
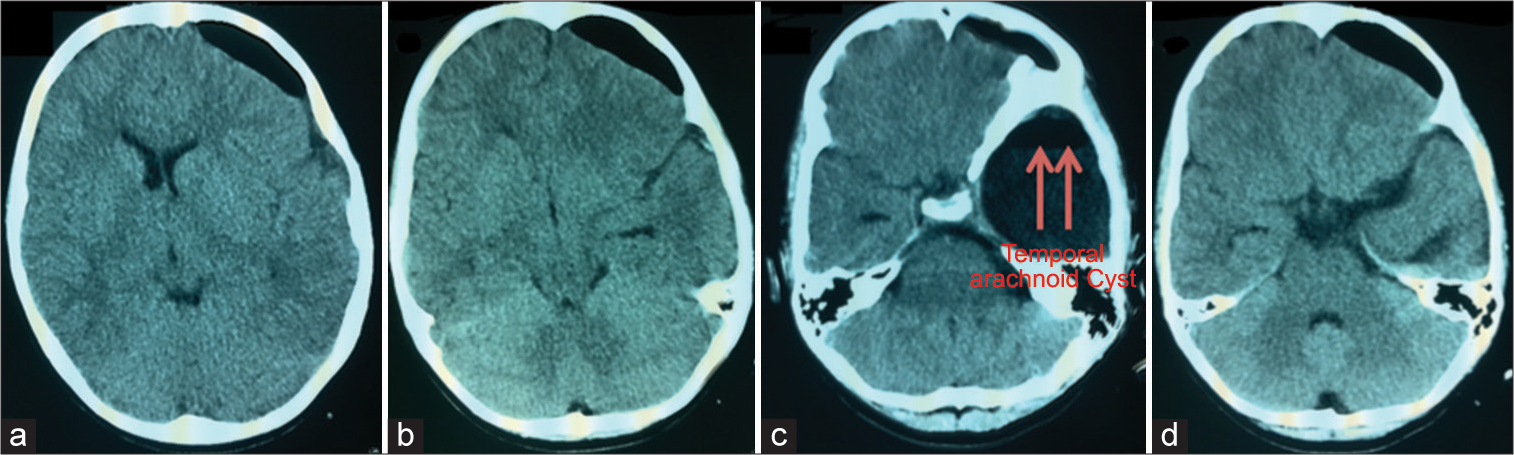
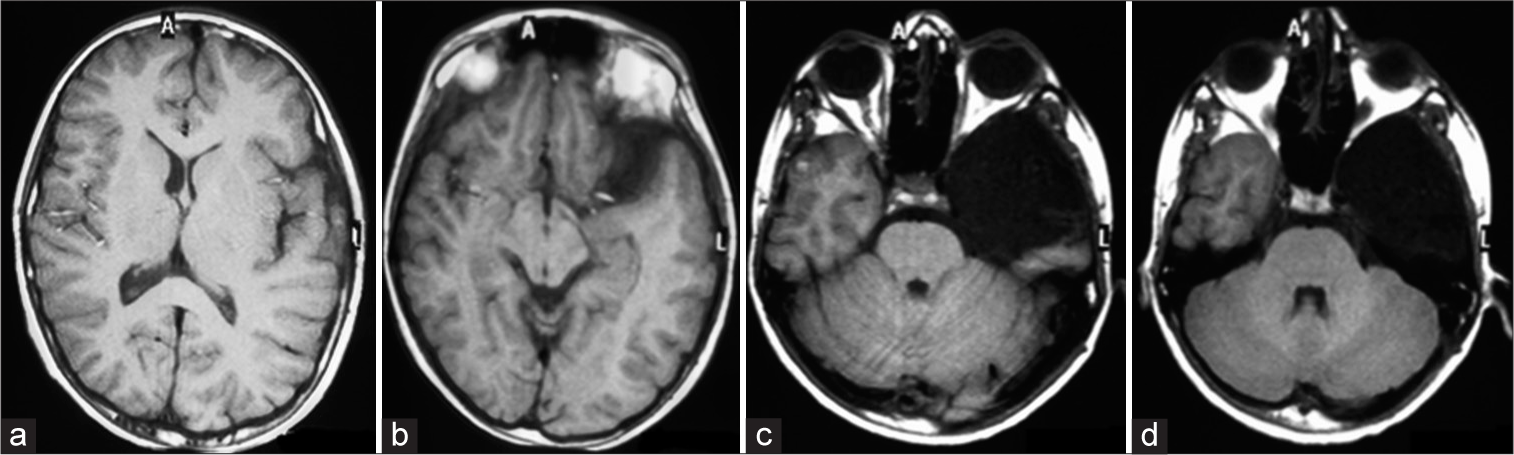
Case Description: We report a case of CSDH associated with AC in a 14-year-old Kuwaiti boy who presented with a 2 weeks history of headache, which was worsening over the time. Brain CT scan demonstrated a left frontotemporal large CSDH in contact with an underlying temporal AC that appeared isodense to the CSF. The patient underwent an emergency surgery to evacuate the CSDH through a burr hole, while the AC was left intact. During the postoperative period, the patient showed good recovery in terms of neurological symptoms. Follow-up MRI showed stable size of the AC with no recurrence of the CSDH.
Conclusion: Literature’s review was done to determine the best surgical approach in treating spontaneous CSDH associated with AC. Burr hole evacuation of CSDH with irrigation only, leaving the AC intact, is a successful surgical approach for treatment and was associated with good outcome.
Keywords: Arachnoid cysts, Burr hole, Craniotomy, Rupture, Rupture, Spontaneous chronic subdural hematoma
INTRODUCTION
Arachnoid cysts (ACs) are benign, congenital, fluid-filled compartments between two layers of the arachnoid membrane, comprising 1% of all the intracranial space-occupying lesions.[
We report a case of AC in association with a spontaneous CSDH successfully treated by burr holes and irrigation. We also reviewed the available literature to recommend a surgical approach based on the proposed underlying pathophysiology and the outcome of the different surgical approaches as reported.
CASE REPORT
A 14-year-old Kuwaiti boy presented with 2 weeks history of headache, which was worsening over the time. There was no history of head trauma and physical examination was unremarkable for neurological deficits. Brain computed tomography (CT) scan demonstrated a left frontotemporal large CSDH [
DISCUSSION
The ACs are most often found in children with a male-to-female ratio of 3:1 and involve the middle cranial fossa in 50% of cases with a slight predilection for the left side.[
The first description of an AC in association with CSDH was by Davidoff and Dyke in 1938.[
Although there are a few published cases in which a CSDH associated with an AC was treated conservatively,[
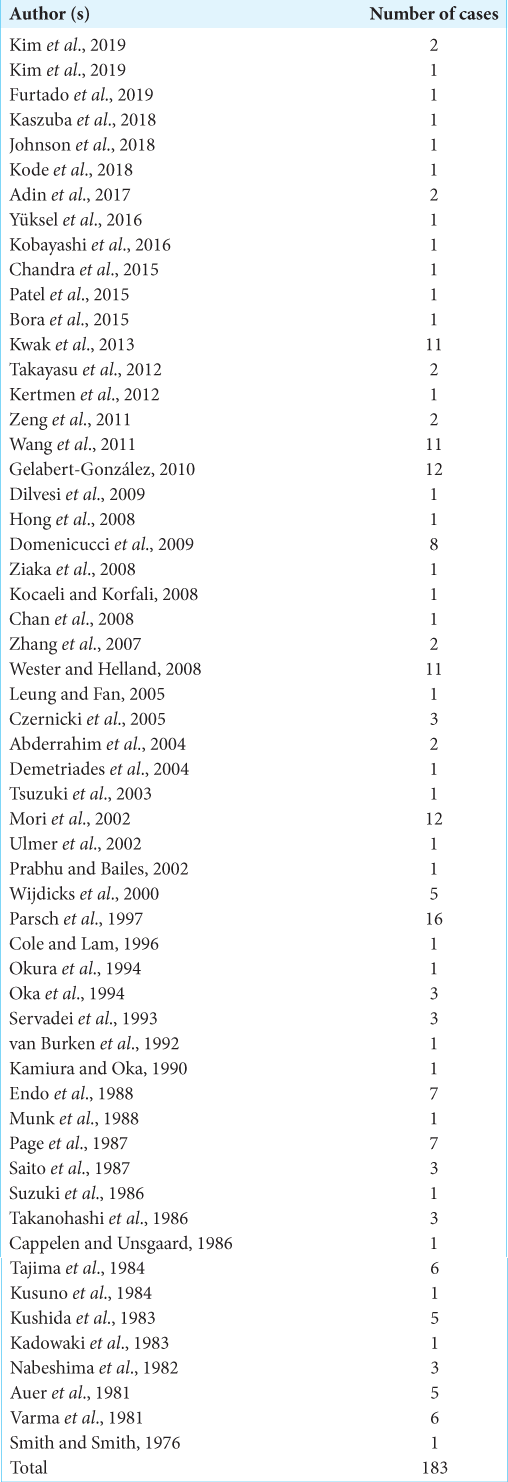
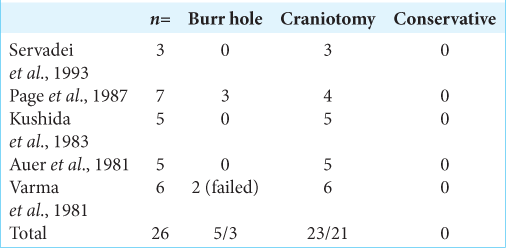
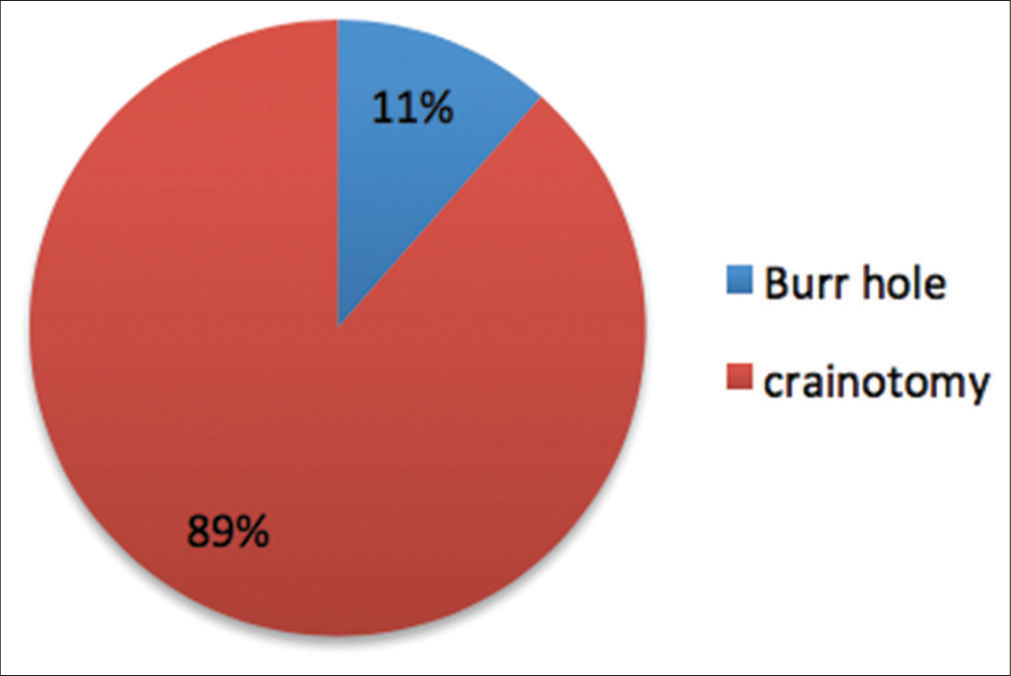
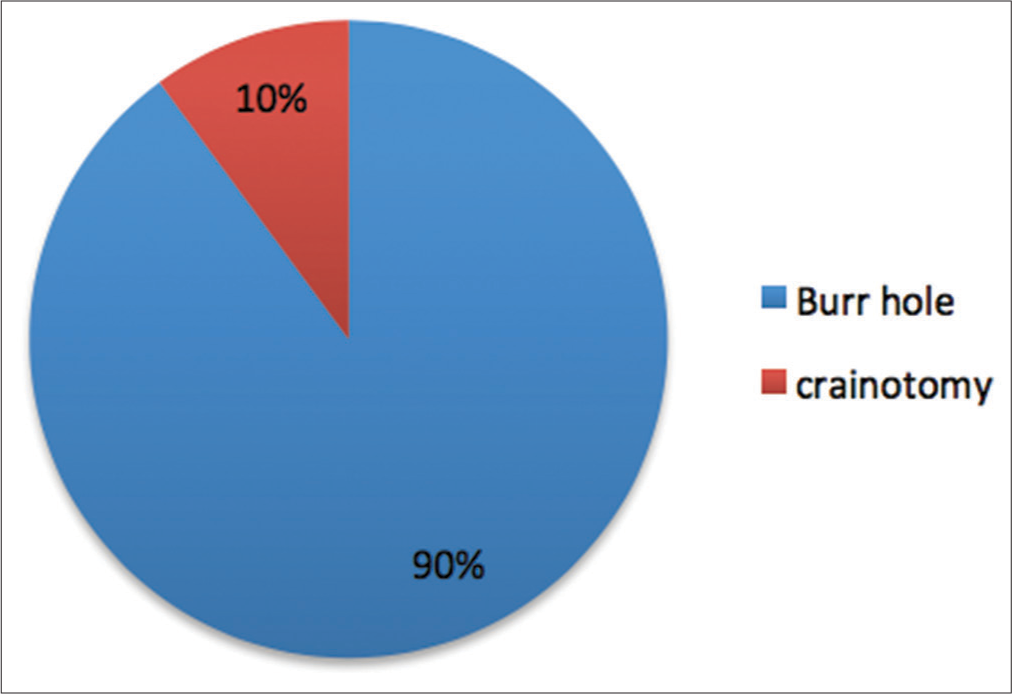
Our review of the literature revealed two interesting findings. First, there was a clear change in the surgical approach for treating CSDH associated with AC over time. Case series published 1981–1993 included a total of 26 patients, of which 23 (88.5%) underwent a craniotomy (21 as first option and two after failed burr hole irrigation) [
Histological data from transmission electron microscopy studies indicated the presence of a membrane separating the AC from the CSDH, rendering them two separate a noncommunicating entity.[
CONCLUSION
The available literature suggests that most patients presenting with CSDH and associated AC can be successfully treated with burr hole and irrigation, and only a minority would require craniotomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abderrahim E, Hedri H, Lâabidi J, Raies L, Kheder A, Abdallah TB. Chronic subdural haematoma and autosomal polycystic kidney disease: Report of two new cases. Nephrology (Carlton). 2004. 9: 331-3
2. Adin ME, Yıldız MS, Deniz MA, Behzadi AH, Mata-Mbemba D. Arachnoid cysts with spontaneous intracystic hemorrhage and associated subdural hematoma: Report of management and follow-up of 2 cases. Radiol Case Rep. 2017. 13: 516-21
3. Aicardi J.editors. Diseases of the Nervous System in Childhood. London: Mac Keith Press; 1992. p. 822-6
4. Arai H, Sato K, Wachi A, Okuda O, Takeda N. Arachnoid cysts of the middle cranial fossa: Experience with 77 patients who were treated with cystoperitoneal shunting. Neurosurgery. 1996. 39: 1108-12
5. Auer LM, Gallhofer B, Ladurner G, Sager WD, Heppner F, Lechner H. Diagnosis and treatment of middle fossa arachnoid cysts and subdural hematomas. J Neurosurg. 1981. 54: 366-9
6. Bora A, Yokuş A, Batur A, Bulut MD, Yavuz A, Gülşen İ. Spontaneous rupture of the middle fossa arachnoid cyst into the subdural space: Case report. Pol J Radiol. 2015. 80: 324-7
7. Cappelen J, Unsgaard G. Arachnoid cysts of the middle cranial fossa and traumatic complications. Childs Nerv Syst. 1986. 2: 225-7
8. Chan JY, Huang CT, Liu YK, Lin CP, Huang JS. Chronic subdural hematoma associated with arachnoid cyst in young adults: A case report. Kaohsiung J Med Sci. 2008. 24: 41-4
9. Chandra VV, Prasad BC, Subramanium CS, Kumar R. Spontaneous intracystic hemorrhage complicating an intracranial arachnoid cyst. J Neurosci Rural Pract. 2015. 6: 629-30
10. Chillala S, Read C, Evans PA. An unusual case of subdural haematoma presenting to the accident and emergency department. Emerg Med J. 2001. 18: 308-9
11. Cole WG, Lam TP. Arachnoid cyst and chronic subdural haematoma in a child with osteogenesis imperfecta Type III resulting from the substitution of glycine 1006 by alanine in the pro alpha 2(I) chain of Type I procollagen. J Med Genet. 1996. 33: 193-6
12. Czernicki T, Marchel A, Nowak A, Bojarski P. Arachnoid cysts of the middle cranial fossa presented as subdural hematomas. Neurol Neurochir Pol. 2005. 39: 328-34
13. Demetriades AK, McEvoy AW, Kitchen ND. Subdural haematoma associated with an arachnoid cyst after repetitive minor heading injury in ball games. Br J Sports Med. 2004. 38: E8
14. Dilvesi D, Vuleković P, Cigić T, Kojadinović Z, Horvat I, Karan M. Treatment of recurrent chronic subdural hematoma in a patient with arachnoid cyst. Med Pregl. 2009. 62: 469-72
15. Domenicucci M, Russo N, Giugni E, Pierallini A. Relationship between supratentorial arachnoid cyst and chronic subdural hematoma: Neuroradiological evidence and surgical treatment. J Neurosurg. 2009. 110: 1250-5
16. Endo G, Matsumoto M, Yamazaki T, Kuroki T, Seki T, Terao H. Temporal fossa arachnoid cyst associated with chronic subdural hematoma. Clinical analysis of 7 cases. Shinkei Gaisho. 1988. 11: 160-6
17. Furtado LM, Val Filho JA, Ferreira RI, Mariano IG. Intracranial arachnoid cyst rupture after mild TBI in children: Have we underestimated this risk?. BMJ Case Rep. 2019. 12: e228790
18. Galassi E, Piazza G, Gaist G, Frank F. Arachnoid cysts of the middle cranial fossa: A clinical and radiological study of 25 cases treated surgically. Surg Neurol. 1980. 14: 211-9
19. Gelabert-González M, Castro-Bouzas D, Arcos-Algaba A, Santín-Amo JM, Díaz-Cabanas L, Serramito-García R. Chronic subdural hematoma associated with arachnoid cyst. Report of 12 cases. Neurocirugia (Astur). 2010. 21: 222-7
20. Gelabert-González M, Iglesias-Pais M, García-Allut A, Martínez-Rumbo R. Chronic subdural haematoma: Surgical treatment and outcome in 1000 cases. Clin Neurol Neurosurg. 2005. 107: 223-9
21. Hong JC, Kim MS, Chang CH, Kim SH. Arachnoid cyst with spontaneous intracystic hemorrhage and chronic subdural hematoma. J Korean Neurosurg Soc. 2008. 43: 54-6
22. Johnson R, Amine A, Farhat H. Spontaneous acute subdural hematoma associated with arachnoid cyst and intra-cystic hemorrhage. Cureus. 2018. 10: e3383
23. Kadowaki H, Ide M, Takara E, Yamamoto M, Imanaga H, Jimbo M. A case of arachnoid cyst as sociated with chronic subdural hematoma. No Shinkei Geka. 1983. 11: 431-6
24. Kamiura T, Oka H. A case of chronic subdural hematoma associated with arachnoid cyst. Teikyo Igaku Zasshi. 1990. 13: 261-6
25. Kaszuba MC, Tan LA, Moftakhar R, Kasliwal MK. Nontraumatic subdural hematoma and intracystic hemorrhage associated with a middle fossa arachnoid cyst. Asian J Neurosurg. 2018. 13: 116-8
26. Kertmen H, Gürer B, Yilmaz ER, Sekerci Z. Chronic subdural hematoma associated with an arachnoid cyst in a juvenile taekwondo athlete: A case report and review of the literature. Pediatr Neurosurg. 2012. 48: 55-8
27. Kim DU, Park HR, Chang JC, Park SQ, Cho SJ, Park HK. Disappearance of arachnoid cyst after burrhole trephination: Case series. Korean J Neurotrauma. 2019. 15: 170-5
28. Kim DY, Lee S, Choi BS, Kim JS. Spontaneous disappearance of an arachnoid cyst after burr hole drainage of chronic subdural hematoma. Korean J Neurotrauma. 2019. 15: 159-63
29. Kobayashi A, Nagashima G, Noda M, Kato A, Morishima H, Koike J. A case of organized arachnoid cyst with repeated hemorrhage. Clin Case Rep. 2016. 4: 250-254
30. Kocaeli H, Korfali E. Rupture of a small middle cerebral artery aneurysm into middle fossa arachnoid cyst presenting as a chronic subdural haematoma. Acta Neurochir (Wien). 2008. 150: 407-8
31. Kode S, Hegde A, Menon G. Chronic subdural hematoma associated with congenital arachnoid cysts: Management dilemmas. Cureus. 2018. 10: e2550
32. Kushida Y, Terao H, Shibata I, Shishido M, Seiki Y, Tsutsumi S. Chronic subdural hematoma associated with arachnoid cyst-study of the mechanism of its development. No Shinkei Geka. 1983. 11: 1211-7
33. Kusuno K, Yoshida Y, Takahashi A, Ishii S. Chronic subdural hygroma caused by rupture of arachnoid cyst. As a probable course to chronic subdural hematoma: Case report. Neurol Med Chir (Tokyo). 1984. 24: 349-54
34. Kwak YS, Hwang SK, Park SH, Park JY. Chronic subdural hematoma associated with the middle fossa arachnoid cyst: Pathogenesis and review of its management. Childs Nerv Syst. 2013. 29: 77-82
35. LaCour F, Trevor R, Carey M. Arachnoid cyst and associated subdural hematoma, Observations on con ventional roentgenographic and computerized tomographic diagnosis. Arch Neurol. 1978. 35: 84-9
36. Leung GK, Fan YW. Chronic subdural haematoma and arachnoid cyst in autosomal dominant polycystic kidney disease (ADPKD). J Clin Neurosci. 2005. 12: 817-9
37. Mooij JJ, Go KG, Vecht CJ.editors. Cysts, cyst-like tumors and other maldevelopmental tumors. Handbook of Clinical Neurology. Neuro-Oncology Part 2. Amsterdam: Elsevier Science; 1997. p. 310-4
38. Mori K, Yamamoto T, Horinaka N, Maeda M. Arachnoid cyst is a risk factor for chronic subdural hematoma in juveniles: Twelve cases of chronic subdural hematoma associated with arachnoid cyst. J Neurotrauma. 2002. 19: 1017-27
39. Munk PL, Robertson WD, Durity FA. Middle fossa arachnoid cyst and subdural hematoma: CT studies. J Comput Assist Tomogr. 1988. 12: 1073-5
40. Nabeshima S, Makita Y, Motomochi M, Itagaki T, Tei T, Keyaki A. Three cases of arachnoid cysts associated with chronic subdural hematoma (author’s transl). No To Shinkei. 1982. 34: 173-8
41. Oka Y, Kumon Y, Ohta S, Sakaki S, Ohue S, Takeda S. Chronic subdural hematoma associated with middle fossa arachnoid cysts-three case reports. Neurol Med Chir (Tokyo). 1994. 34: 95-9
42. Okura A, Noguchi S, Yuge T, Maruiwa H, Matsunaga M, Shigemori M. A case of convexity arachnoid cyst associated with chronic subdural hematoma and intracystic hemorrhage. No Shinkei Geka. 1994. 22: 273-7
43. Page A, Paxton RM, Mohan D. A reappraisal of the relationship between arachnoid cysts of the middle fossa and chronic subdural haematoma. J Neurol Neurosurg Psychiatry. 1987. 50: 1001-7
44. Parsch C, Krau J, Hoffman E, Meixensberger J, Roosen K. Arachnoid cysts associated with subdural hematomas and hygromas. Follow-up, and review of the literature. Neurosurgery. 1997. 40: 483-90
45. Patel AP, Oliverio PJ, Kurtom KH, Roberti F. Spontaneous subdural hematoma and intracystic hemorrhage in an arachnoid cyst. Radiol Case Rep. 2015. 4: 298
46. Prabhu VC, Bailes JE. Chronic subdural hematoma complicating arachnoid cyst secondary to soccer-related head injury: Case report. Neurosurgery. 2002. 50: 195-7
47. Rengachary SS, Watanabe I. Ultrastructure and pathogenesis of intracranial arachnoid cysts. J Neuropathol Exp Neurol. 1981. 40: 61-83
48. Saito A, Nakazawa T, Matsuda M, Handa J. Association of subdural hematoma and middle fossa arachnoid cyst: Report of 3 cases and a review. No Shinkei Geka. 1987. 15: 689-93
49. Sato K, Shimoji T, Yaguchi K, Sumie H, Kuru Y, Ishii S. Middle fossa arachnoid cyst: Clinical, neuroradiological, and surgical features. Childs Brain. 1983. 10: 301-16
50. Schachenmayr W, Friede RL. Fine structure of arachnoid cysts. J Neuropathol Exp Neurol. 1979. 38: 434-46
51. Servadei F, Vergani G, Fratarelli M, Pasini A, Arista A, Fagioli L. Arachnoid cyst of middle cranial fossa and ipsilateral subdural haematoma: Diagnostic and therapeutic implications in three cases. Br J Neurosurg. 1993. 7: 249-53
52. Smith RA, Smith WA. Arachnoid cysts of the middle cranial fossa. Surg Neurol. 1976. 5: 246-52
53. Starkman SP, Brown TC, Linell EA. Cerebral arachnoid cysts. J Neuropathol Exp Neurol. 1958. 17: 484-500
54. Suzuki M, Takahashi S, Sonobe M, Kuwayama N. Arachnoid cyst of the middle cranial fossa combined with ipsilateral multiple chronic subdural hematomas. Case report. Neurol Med Chir (Tokyo). 1986. 26: 240-4
55. Tajima K, Saito Y, Nagai K, Takeda Y, Miwa T, Hasue M. Clinical analysis of six cases of arachnoid cysts associated with chronic subdural hematomas or intracystic hemorrhage. Shinkei Gaisho. 1984. 7: 123-30
56. Takanohashi M, Amano Y, Mizutani T, Tanoi C, Akabane A. Three cases of arachnoid cyst of the middle cranial fossa associated with subdural hematoma. Shizuoka Saiseikai Byoin Igaku Zasshi. 1986. 4: 9-18
57. Takayasu T, Harada K, Nishimura S, Onda J, Nishi T, Takagaki H. Chronic subdural hematoma associated with arachnoid cyst. Two case histories with pathological observations. Neurol Med Chir (Tokyo). 2012. 52: 113-7
58. Tsuzuki N, Katoh H, Ohtani N. Chronic subdural hematoma complicating arachnoid cyst secondary to soccer-related head injury: Case report. Neurosurgery. 2003. 53: 242-3
59. Ulmer S, Engellandt K, Stiller U, Nabavi A, Jansen O, Mehdorn MH. Chronic subdural hemorrhage into a giant arachnoidal cyst (Galassi classification Type III). J Comput Assist Tomogr. 2002. 26: 647-53
60. Van Burken MM, Sarioglu AC, O’Donnell HD. Supratentorial arachnoid cyst with intracystic and subdural haematoma. Neurochirurgia (Stuttg). 1992. 35: 199-203
61. Varma TR, Sedzimir CB, Miles JB. Post-traumatic complications of arachnoid cysts and temporal lobe agenesis. J Neurol Neurosurg Psychiatry. 1981. 44: 29-34
62. Voss M, Knottenbelt JD, Peden MM. Patients who reattend after head injury: A high risk group. BMJ. 1995. 311: 1395-8
63. Wang KD, Zhao JZ, Li JS, Zhang Y. Clinical study of patients of arachnoid cyst associated with chronic subdural hematoma. Zhonghua Yi Xue Za Zhi. 2011. 91: 460-3
64. Wester K, Helland CA. How often do chronic extracerebral haematomas occur in patients with intracranial arachnoid cysts?. J Neurol Neurosurg Psychiatry. 2008. 79: 72-5
65. Wester K. Gender distribution and sidedness of middle fossa arachnoid cysts: A review of cases diagnosed with computed imaging. Neurosurgery. 1992. 31: 940-4
66. Wijdicks EF, Torres VE, Schievink WI. Chronic subdural hematoma in autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2000. 35: 40-3
67. Yüksel MO, Gürbüz MS, Senol M, Karaarslan N. Spontaneous subdural haematoma developing secondary to arachnoid cyst rupture. J Clin Diagn Res. 2016. 10: PD05-6
68. Zeng T, Shi SS, Lin YF. Chronic subdural hematoma associated with sylvian arachnoid cyst in juvenile athletes: Report of two cases and literature review. Chin J Traumatol. 2011. 14: 174-7
69. Zhang H, Zhang J, Chen G. Chronic subdural hematoma associated with arachnoid cyst: Report of two cases. Chin Med J. 2007. 120: 2339-40
70. Ziaka DS, Kouyialis AT, Boviatsis EJ, Sakas DE. Asymptomatic massive subdural hematoma in a patient with bitemporal agenesis and bilateral temporal arachnoid cysts. South Med J. 2008. 101: 324-6