- Department of Surgery, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe
- Department of Haematology, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe
Correspondence Address:
Kazadi K. N. Kalangu
Department of Surgery, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe
DOI:10.4103/2152-7806.183543
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jokonya L, Musara A, Cakana A, N. Kalangu KK. Spontaneous chronic subdural hematomas in human immunodeficiency virus-infected patients with normal platelet count and no appreciable brain atrophy: Two case reports and review of literature. Surg Neurol Int 03-Jun-2016;7:
How to cite this URL: Jokonya L, Musara A, Cakana A, N. Kalangu KK. Spontaneous chronic subdural hematomas in human immunodeficiency virus-infected patients with normal platelet count and no appreciable brain atrophy: Two case reports and review of literature. Surg Neurol Int 03-Jun-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/spontaneous-chronic-subdural-hematomas-in-human-immunodeficiency-virus%e2%80%91infected-patients-with-normal-platelet-count-and-no-appreciable-brain-atrophy-two-case-reports-and-review-of-literature/
Abstract
Background:Chronic subdural hematomas (CSDHs) usually occur in elderly patients following minor head trauma. Their occurrence is usually linked to cerebral atrophy secondary to alcohol, old age, or human immunodeficiency virus (HIV) infection. Spontaneous CSDHs have also been documented but are rare. They are usually caused by coagulopathies and various pathologies resulting in intracranial hypotension.
Cases:We have observed a number of spontaneous CSDHs in HIV patients with normal platelet counts and no appreciable cerebral atrophy possibly caused by platelet dysfunction, hence we report about two such cases. To the best of our knowledge, no such cases have been reported in literature before.
Conclusion:It is important to include CSDHs in the differential diagnosis of HIV patients presenting with neurological deficits even without a history of trauma.
Keywords: Human immunodeficiency virus coagulopathy, spontaneous chronic subdural hematoma, subdural bleeds
BACKGROUND
The incidence of chronic subdural hematoma (CSDH) is increasing.[
However, with a high prevalence of HIV/acquired immune deficiency syndrome (AIDS) in Sub-Saharan Africa, a significant proportion of younger patients have been noted to develop CSDHs from our observation. This may be attributed to cerebral atrophy occurring at a younger age and also thrombocytopenia,[
CLINICAL PRESENTATIONS
Case 1
A 35-year-old HIV-positive male patient on TenoLam-N (tenofovir, lamivudine, and nevirapine) with CD4 T-cell lymphocyte count of 198 cells/μL (normal 410–1590) presents with a 3-day history of headaches associated with vomiting and a day's history of confusion. He also had an isolated episode of diarrhea but had no history of; trauma, taking alcohol, nonsteroidal anti-inflammatories, herbal medicines, or any other medications other than his antiretrovirals. He works as a school teacher and was otherwise relatively well before this.
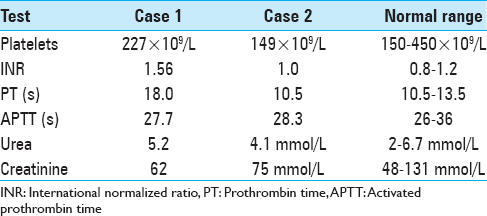
On examination, he was confused, having a Glasgow Comma Scale of 14/15. He had bilateral parotid fullness and was apyrexial with no neck stiffness. He had right-sided hyperreflexia with positive Babinski sign. There were no signs of recent trauma. The rest of the examination was normal. Electrolytes and full blood count were normal.
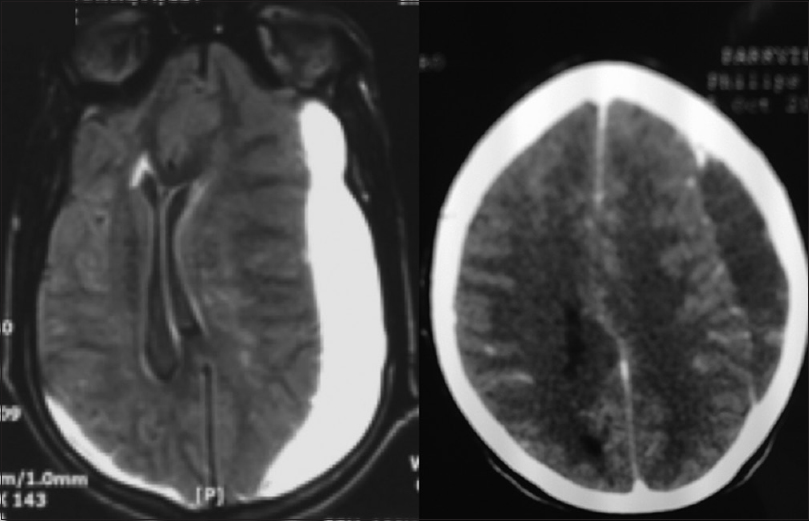
Figure 1
Magnetic resonance imaging (left, Case 1) showed large left-sided fronto-parieto-occipital chronic subdural hematoma, with a small contralateral occipital collection. Computer tomography (right, Case 2) shows left-sided parietal bleed. Both show significant midline shift with compression of the right lateral ventricle but no appreciable brain atrophy
He was taken for emergency evacuation of the hematoma via an enlarged burr hole. The operation and recovery were uneventful. The confusion improved and the patient was discharged fully consciousness on day 6.
Case 2
A 42-year-old HIV-positive female patient on TenoLam-N with a CD4 T-cell lymphocyte count of 49 cells/μL presented with a month's history of gradually worsening headaches and 2-day history of confusion with right-sided weakness. Her baseline CD4 T-cell lymphocyte count had been 240 cells/μL before commencing antiretrovirals about 1 year ago. She had no history of taking anticoagulants, nonsteroidal anti-inflammatories, herbal medicines, alcohol use, or any other medications other than her antiretrovirals. No history of trauma could be elicited even after recovery.
On examination, she was drowsy and confused. Her left pupil was dilated with sluggish response to light. She had right-sided hemiparesis with no facial involvement. She had no physical signs of trauma. The rest of the examination was noncontributory. The full blood count, urea, and electrolytes were unremarkable.
The patient was taken for emergency burr hole evacuation of the CSDH. Operation and recovery were uneventful, and the patient was discharged on day 5. On follow-up, at 2 weeks, the level of consciousness was 15/15. She was referred to the physicians for possible HIV treatment failure on account of her diminishing CD4 cell count.
DISCUSSION
The most common cause of CSDH is trauma, in a predisposed brain. Two-thirds of CSDH patients recall some type of minor trauma.[
However, spontaneous CSDHs are recognized in literature.[
In our two patients, there was no history of trauma that could be elicited. The patients were of sober habits, hence alcoholism could not be considered as a possible cause. The imaging did not show any appreciable cerebral atrophy that could have predisposed our patients to subdural bleeds. The patients were quite young to fit the generally accepted age group of chronic subdural bleeds. Some rarer documented causes include also straining[
Cases of spontaneous CSDH without an identifiable cause have been documented in literature.[
HIV infection predisposes to both hemorrhage and thrombosis, and the mechanisms are believed to be multifactorial with some still to be elucidated ranging from blood vessel vasculitis to true blood coagulopathies.
Although relatively rare, vasculitides are important complications of all stages of HIV infection. The vasculitides seen in HIV-infected patients represent the full spectrum of disease, ranging from that caused by specific infective agents to nonspecific vasculitis, and affecting large, medium, and small vessels. A wide range of pathogenic mechanisms are involved in the development of necrotizing vasculitis, many of which remain to be elucidated, but all of which are linked by an underlying inflammation of the vessel wall.
Liver dysfunction, caused by the viral infection itself or the effects of antiretrovirals, may lead to coagulation factor deficiencies. Further, the presence of antibodies is believed to coat the platelets interfering with their function. In some cases, high immunoglobulin proteins are believed to interfere with coagulation factors leading to hemorrhage.[
CONCLUSION
HIV has many neurological manifestations. Given the hematological effects of retroviral infection, CSDHs need to be considered early in the differentials of an HIV patient even if history of trauma cannot be elicited. Brain imaging should be done early in HIV-positive patients with symptoms suggestive of CSDH. This will allow prompt diagnosis, early appropriate intervention with generally good prognosis in retroviral infected patients without significant comorbidity. Further studies need to be done with regards to bleeding abnormalities in HIV infection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adhiyaman V, Asghar M, Ganeshram KN, Bhowmick BK. Chronic subdural haematoma in the elderly. Postgrad Med J. 2002. 78: 71-5
2. de Noronha RJ, Sharrack B, Hadjivassiliou M, Romanowski CA. Subdural haematoma: A potentially serious consequence of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2003. 74: 752-5
3. Guillevin L. Vasculitides in the context of HIV infection. AIDS. 2008. 22: S27-33
4. Jacome DE, Yanez GF. Subdural haematoma upon straining. J Neurol Neurosurg Psychiatry. 1989. 52: 134-
5. Kunz U, Panning B, Stolke D. Chronic subdural hematoma following spinal anesthesia. Reg Anaesth. 1989. 12: 34-7
6. Lavie F, Hervé D, Le Ber I, Brault JL, Sangla S, de Broucker T. Bilateral intracranial subdural hematoma following lumbar puncture: Report of a case. Rev Neurol (Paris). 1998. 154: 703-5
7. Manuel A, Victório T, Gomes C, Martins T, Dias Neto A. Vasculitis: An unusual manifestation in an HIV-infected patient. Braz J Infect Dis. 2015. 19: 439-41
8. Mori K, Maeda M. Risk factors for the occurrence of chronic subdural haematomas after neurosurgical procedures. Acta Neurochir (Wien). 2003. 145: 533-9
9. Moscote-Salazar LF, Alvis-Miranda HR, Calderón-Miranda W, Alcala-Cerra G, Rubiano AM. Spontaneous chronic subdural hematoma in a young male patient: Case report. Rom Neurosurg. 2014. 2: 230-5
10. Pagnoux C, Cohen P, Guillevin L. Vasculitides secondary to infections. Clin Exp Rheumatol. 2006. 24: S71-81
11. Richard Winn H.editors. Youmans Neurological Surgery. New York: Elsevier Saunders; 2013. 1: 532-6
12. Scaradavou A. HIV-related thrombocytopenia. Blood Rev. 2002. 16: 73-6
13. Wang HS, Kim SW, Kim SH. Spontaneous chronic subdural hematoma in an adolescent girl. J Korean Neurosurg Soc. 2013. 53: 201-3