- Department of Neurosurgery, Texas A&M University College of Medicine, Bryan, Texas, United States,
- Department of Neurosurgery, Cannizzaro Hospital, Catania, Italy.
- Department of Neurosurgery, Highly Specialized Hospital and of National Importance “Garibaldi,” Catania, Italy.
- Department of Radiation Oncology, REM Radioterapia srl, Viagrande, Italy.
Correspondence Address:
Giuseppe E. Umana, Department of Neurosurgery, Cannizzaro Hospital, Catania, Italy.
DOI:10.25259/SNI_1225_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kishore Balasubramanian1, Paolo Palmisciano2, Gianluca Scalia3, Antonio Crea2, Ali S. Haider1, Saverio Fagone2, Gianluca Ferini4, Anna Viola4, Salvatore Cicero2, Giuseppe Emmanuele Umana2. Spontaneous intracerebral pseudoaneurysm rupture and meningiomatosis: A case report and review of the literature. 20-Jan-2022;13:23
How to cite this URL: Kishore Balasubramanian1, Paolo Palmisciano2, Gianluca Scalia3, Antonio Crea2, Ali S. Haider1, Saverio Fagone2, Gianluca Ferini4, Anna Viola4, Salvatore Cicero2, Giuseppe Emmanuele Umana2. Spontaneous intracerebral pseudoaneurysm rupture and meningiomatosis: A case report and review of the literature. 20-Jan-2022;13:23. Available from: https://surgicalneurologyint.com/surgicalint-articles/11354/
Abstract
Background: We report the first case of a spontaneous ruptured anterior cerebral artery pseudoaneurysm in a patient affected by meningiomatosis.
Case Description: A 71-year-old female patient was admitted to our emergency department after acute loss of consciousness. An urgent head CT scan showed third ventricle hemorrhage and a giant extra-axial tumor with associated peritumoral bleeding. A second, smaller, and right-sided tumor was detected at the posterior third of the superior sagittal sinus, indicative of meningiomatosis diagnosis. A following CT angiogram showed an hypervascularized lesion at the right frontal convexity and a ruptured A2 pseudoaneurysm. Tumor removal was performed through right frontal craniotomy. After the initial debulking and removal of the peritumoral hemorrhage, the A2 segment associated with the bleeding pseudoaneurysm was surgically coagulated.
Conclusion: We report the unique occurrence of two relatively rare neurological entities: meningiomatosis and intracranial pseudoaneurysm. In our experience, their simultaneous and acute presentation is associated to poor prognosis.
Keywords: Giant meningioma, Intracranial hemorrhage, Meningiomatosis, Pseudoaneurysm
INTRODUCTION
Meningiomas are the most common primary intracranial tumors, representing 37% of all primary brain tumors. Meningiomatosis, however, is a rare neurological phenomenon accounting for <2% of all meningioma cases.[
CASE ILLUSTRATION
Clinical history
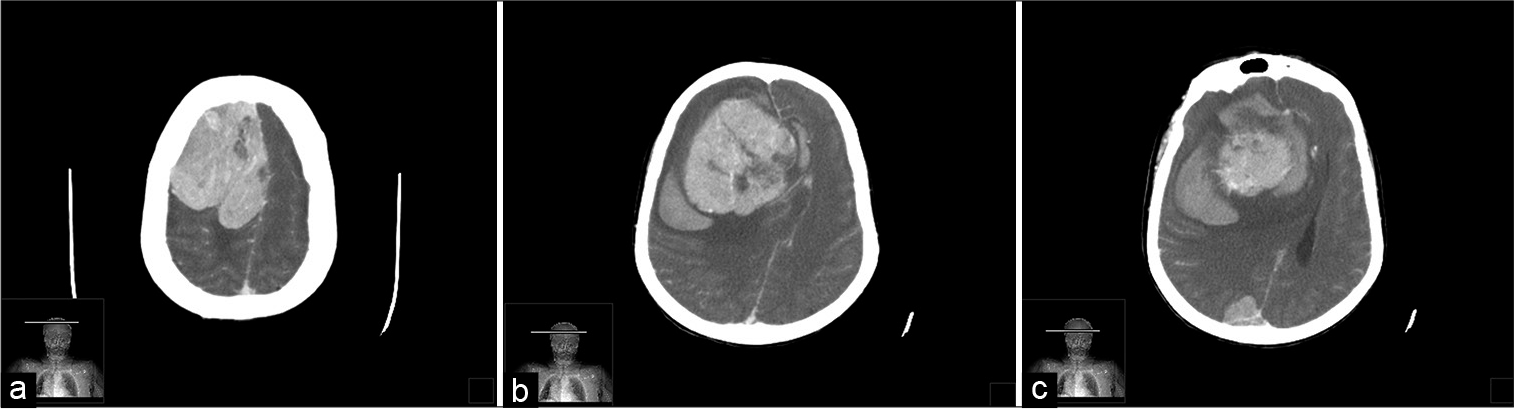
A 71-year-old female patient was admitted to our emergency department after acute loss of consciousness with a Glasgow Coma Scale score of 4/15. Neurological examination revealed anisocoric pupils (right>left), drowsiness, left-sided hemiplegia, and right-sided decerebration. An urgent head CT scan showed third ventricle hemorrhage and a giant extra-axial tumor with associated peritumoral bleeding [
Figure 1:
Axial CT with contrast: (a) right frontal convexity giant meningioma; (b) axial CT scan of the patient showing intracranial hemorrhage concurrent to the giant meningioma. Large peritumor brain edema and midline shift (2.5 cm) are also noted; (c) small 2 cm meningioma on the third posterior of the SSS.
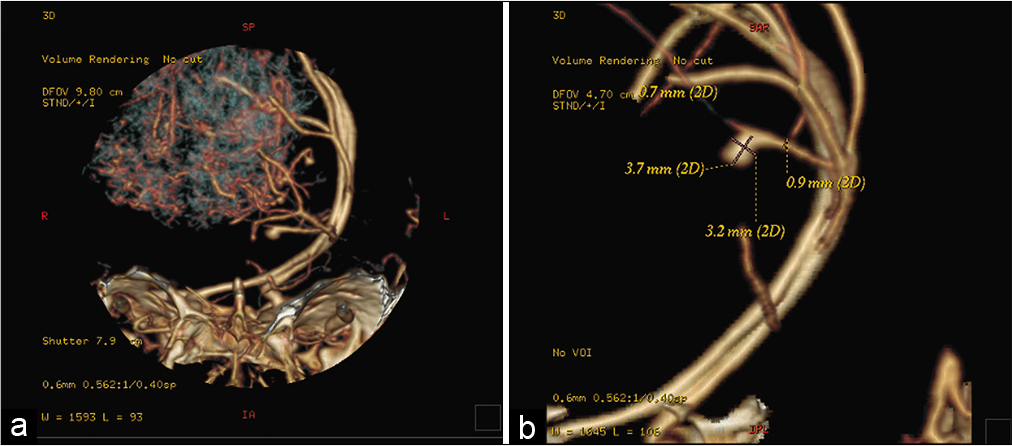
A brain CT angiogram was performed, showing a hypervascularized lesion located at the right frontal convexity, with related mass effect and contralateral midline shift (2.5 cm). A ruptured A2 pseudoaneurysm (93.7 mm × 3.2 mm) was also documented [
A right frontal craniotomy was performed. After the dura mater was opened, the tumor with the associated perilesional bleeding was exposed. The neoplasm was friable in consistence and was easily aspirable using and ultrasonic aspirator, showing macroscopic features concordant with a typical meningioma presentation. Although the macroscopic vascularization was prone to intraoperative bleeding, it was controlled with bipolar cauterization. After the initial debulking and removal of the peritumoral hemorrhage, the frontopolar artery was exposed through an interhemispheric dissection to reach the A2 segment associated with the bleeding pseudoaneurysm, which was then coagulated. We completed the procedure achieving a radical removal of the tumor and a satisfying hemostasis. Bone flap was replaced, and pathological tissue was sent for histological examination.
Histological examination
The histological analysis reported a fibrous meningioma (WHO Grade I) with diffuse intraparenchymal hemorrhage, without a brain parenchyma infiltration (EMA + and progesterone +).
Postoperative course and postoperative imaging
After surgery, the patient was isochoric, and a further postoperative CT scan demonstrated common postoperative findings, including improvement of the midline shift and right frontal hypodensity related to the malacic brain parenchyma next to the meningioma [
DISCUSSION
Meningiomatosis is a rare entity occurring in 1–2% of all meningiomas cases. It is defined as two or more meningiomas occurring simultaneously in different locations without an association with neurofibromatosis, as in the case of our patient. The pathophysiology of meningiomatosis is still not well understood. One theory suggests that the multiple tumors are a result of tumor cell migration through cerebrospinal fluid. In contrast, other studies have found evidence that points toward the independent evolution of the tumors.[
The case we presented is the first association between pseudoaneurysms and meningiomatosis in an adult patient. The only other published case of pseudoaneurysms in association with meningiomatosis occurred in a pediatric patient.[
Individually, meningiomatosis and cerebral pseudoaneurysms have relatively straightforward management strategies with reasonable outcomes. However, as seen in the case we describe, the simultaneous presentation can necessitate rapid and complex surgical interventions, and yet still result in rapid clinical depression and dismal prognosis.
In the present case, the giant convexity meningioma may have contributed to the rupture of the adjacent A2 pseudoaneurysm. Indeed, the mass effect of the tumor caused increased intracranial pressure, responsible for a consequent rise in the intracranial blood pressure to maintain a constant brain perfusion. The process likely started a vicious cascade that leads to the bradycardia and irregular breathing seen in our patient (Cushing reflex). The rupture of the A2 pseudoaneurysm contributed to the intraventricular and peritumoral bleeding, further worsening the rise in the intracranial pressure and causing the sudden loss of consciousness and anisocoria that required urgent treatment.
Pseudoaneurysms are most frequently associated with trauma, but other etiologies include iatrogenic injuries, infectious disease, and connective tissue disease. The specific incidence of tumor-related pseudoaneurysms, such as the case we describe, is not known. The majority of intracranial pseudoaneurysms reported in the literature result from complications of tumor resection surgery.[
CONCLUSION
We report the unique simultaneous occurrence of two relatively rare neurological entities in one patient, namely, cerebral meningiomatosis and intracranial pseudoaneurysm. Based on our experience, their simultaneous and acute presentation should be promptly managed but is still associated with poor prognosis.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brilakis E.editors. Vascular access complications. Manual of Percutaneous Coronary Interventions. Amsterdam, Netherlands: Elsevier; 2021. p. 471-84
2. Ohla V, Scheiwe C. Meningiomatosis restricted to the left cerebral hemisphere with acute clinical deterioration: Case presentation and discussion of treatment options. Surg Neurol Int. 2015. 6: 64
3. Settecase F, Nicholson AD, Amans MR, Higashida RT, Halbach VV, Cooke DL. Onyx embolization of an intraosseous pseudoaneurysm of the middle meningeal artery in a patient with meningiomatosis, McCune-Albright syndrome, and gray platelet syndrome. J Neurosurg Pediatr. 2016. 17: 324-9
4. Tsermoulas G, Turel MK, Wilcox JT, Shultz D, Farb R, Zadeh G. Management of multiple meningiomas. J Neurosurg. 2018. 128: 1403-9
5. Umana GE, Cristaudo C, Scalia G, Passanisi M, Corsale G, Tomarchio L. Chronic epidural hematoma caused by traumatic intracranial pseudoaneurysm of the middle meningeal artery: Review of the literature with a focus on this unique entity. World Neurosurg. 2020. 136: 198-204