- Departamento de Neurocirurgia, Centro Hospitalar de Lisboa Central EPE, Lisboa, Portugal
- Departamento de Neurocirurgia, Centro Hospitalar do Algarve, Hospital de Faro, Portugal
Correspondence Address:
Gonçalo Novais
Departamento de Neurocirurgia, Centro Hospitalar de Lisboa Central EPE, Lisboa, Portugal
DOI:10.4103/sni.sni_179_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gonçalo Novais, Bernardo Ratilal, Lia Pappamikail, Pedro Branco, Nuno Reis. Spontaneous pseudomeningocele associated with lumbar spondylolisthesis: A case report and review of the literature. 07-Sep-2017;8:221
How to cite this URL: Gonçalo Novais, Bernardo Ratilal, Lia Pappamikail, Pedro Branco, Nuno Reis. Spontaneous pseudomeningocele associated with lumbar spondylolisthesis: A case report and review of the literature. 07-Sep-2017;8:221. Available from: http://surgicalneurologyint.com/surgicalint-articles/spontaneous-pseudomeningocele-associated-with-lumbar-spondylolisthesis-a-case-report-and-review-of-the-literature/
Abstract
Background:Pseudomeningocele, an extradural collection of cerebrospinal fluid (CSF), has only been rarely reported to occur spontaneously in conjunction with isthmic spondylolisthesis (with lysis) in the lumbar spine.
Case Description:A 68-year-old male presented with low back pain and neurogenic claudication of several years duration without any history of trauma, epidural spine injections, or spine surgery. Lumbosacral magnetic resonance imaging (MRI) revealed a grade-I L4–L5 isthmic spondylolisthesis with spinal canal narrowing and a posterior paravertebral collection consistent with CSF. The patient underwent a spinal decompression consisting of a complete L4 and partial L5 laminectomy, a bilateral L4–L5 instrumented fusion (due to the lysis defect), and closure of the CFS fistula. The histology analysis was compatible with a pseudomeningocele.
Conclusion:Lumbar isthmic spondylolisthesis may lead to changes in the elastic properties of the underlying dura mater. Rarely, this may lead to meningeal tears and formation of a pseudomeningocele. Historically, one must always check for a prior epidural injection that could have resulted in this complication. Additionally, as most likely the case here, the lysis defect was responsible for the foraminal dural laceration resulting in the pseudomeningocele.
Keywords: Cerebrospinal fluid fistula, spondylolisthesis, spontaneous lumbar pseudomeningocele
INTRODUCTION
Pseudomeningocele, an abnormal extradural collection of cerebrospinal fluid (CSF), is attributed to a dural/arachnoidal tear seen in conjuction with isthmic spondylolisthesis/lysis. This lysis-zone tissue is highly organized with collagen bundles and fibrocartilaginous enthesis, some of which are calcified.[
Here, we present a patient with a lumbar pseudomeningocele associated with isthmic spondylolisthesis/lysis and discuss the pathophysiologic mechanisms potentially responsible for this CSF fistula.
CASE HISTORY
A 68-year-old male presented with long standing and increasing low back pain characterized by neurogenic claudication. Within the last 7 months, he was able to walk less than 100 m at a time. There was no history of trauma, epidural injections, or lumbar surgery.
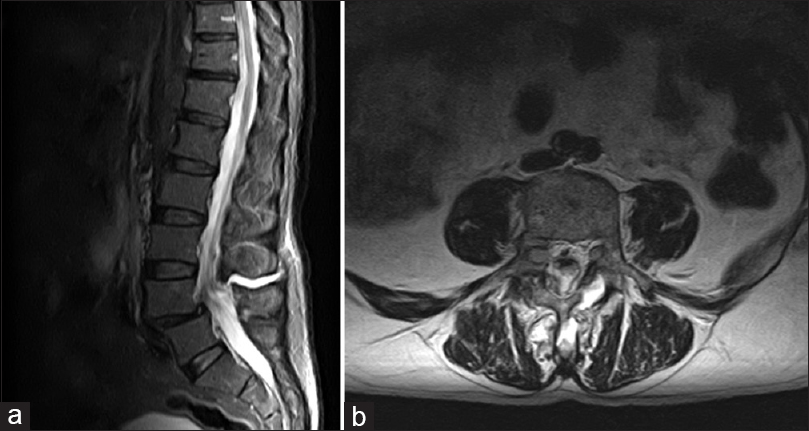
His neurological examination was normal. Plain X-ray images of the lumbar spine revealed grade-I Meyerding L4–L5 chronic spondylolisthesis/lysis. Magnetic resonance imaging (MRI) showed an L4–L5 isthmic spondylolisthesis/lysis with an interspinous and posterior paravertebral collection consistent with a CSF fistula/pseudomeningocele [
The patient underwent an L4 and partial L5 laminectomy. A CSF-filled cavity with a fibrous wall was located posteriorly in the paravertebral muscles (left-sided).
Once the dura was exposed beneath the lysis defect (pars interarticularis) on the left side, a “cavity neck protruded from the thecal sac.” The cavity was widely opened and a wall biopsy was obtained (note that there was no neural tissue within this defect). We performed closure with 3-0 absorbable sutures and fibrin glue. Segmental L4–L5 bilateral pedicle screw fixation was performed for spinal stabilization.
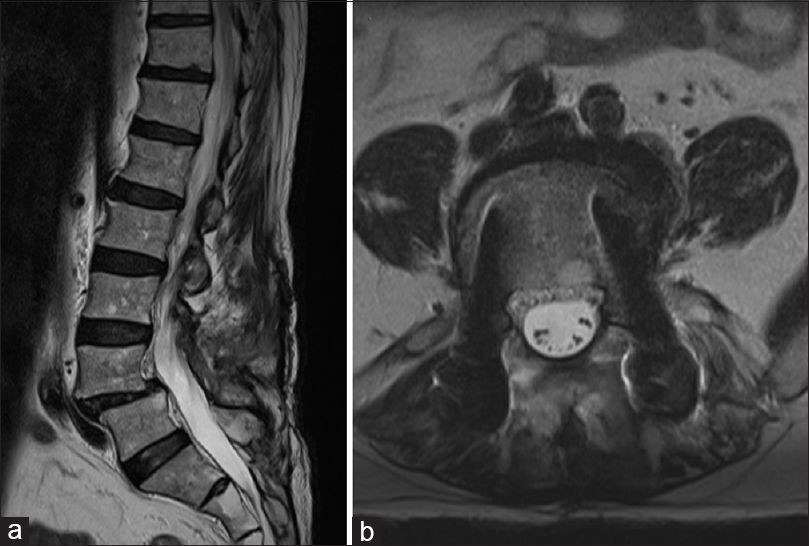
The postoperative course was uneventful. The patient was discharged on the third postoperative day. Histology was compatible with pseudomeningocele. Two months postoperatively, the patient reported full relief of neurogenic claudication and considerable improvement in back pain. One year later, the MRI examination showed complete resolution of the pseudomeningocele and fusion at the L4–L5 level was confirmed (on dynamic X-rays) [
DISCUSSION
Typically, pseudomeningoceles are classified as congenital, traumatic, or iatrogenic. The most common are iatrogenic, resulting from unintended dural tear during surgery.[
Although this patient had a spontaneous CSF lumbar fistula in onset, in fact, it likely resulted from dural laceration ocurring below the left-sided lysis defect.
There are multiple other etiologies of pseudomeningoceles. Shimazakiet al. suggested that iatrogenic pseudomeningoceles may occur after lumbar laminectomies.[
In this case, the pseudomeningocele was, therefore, attributable to a defect of well-organized collagenous/fibrocartilaginous enthesis, with possible calcifications and bony spurs,[
CONCLUSION
A patient presented with a spontaneous CSF fistula that occurred beneath a left-sided L4–L5 lysis defect.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arnold PM, Teuber J. Marfan syndrome and symptomatic sacral cyst: Report of two cases. J Spinal Cord Med. 2013. 36: 499-503
2. Banno T, Ohishi T, Suzuki D, Honda Y, Kobayashi S, Matsuyama Y. Traumatic sacral pseudomeningocele with spina bifida occulta. J Neurosurg Spine. 2012. 16: 78-81
3. Boszczyk BM, Boszczyk AA, Boos W, Korge A, Mayer HM, Putz R. An immunohistochemical study of the tissue bridging adult spondylolytic defects-the presence and significance of fibrocartilaginous entheses. Eur Spine J. 2006. 15: 965-71
4. Couture D, Branch CL. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003. 15: E6-
5. Shimazaki K, Nishida H, Harada Y, Hirohata K. Late recurrence of spinal stenosis and claudication after laminectomy due to an ossified extradural pseudocyst. Spine. 1991. 16: 221-4
6. Solomon P, Sekharappa V, Krishnan V, David KS. Spontaneous resolution of postoperative lumbar pseudomeningoceles: A report of four cases. Indian J Orthop. 2013. 47: 417-21
7. Tsuji H, Handa N, Handa O, Tajima G, Mori K. Postlaminectomy ossified extradural pseudocyst. Case report. J Neurosurg. 1990. 73: 785-7