- Department of Neurosurgery, Tsukuba Memorial Hospital, Tsukuba, Japan.
- Department of Neurosurgery, University of Tsukuba, Tsukuba, Japan.
Correspondence Address:
Eiichi Ishikawa, Department of Neurosurgery, University of Tsukuba, Tsukuba, Japan.
DOI:10.25259/SNI_279_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sho Hanai1, Kiyoyuki Yanaka1, Hitoshi Aiyama1, Michihide Kajita1, Eiichi Ishikawa2. Spontaneous resorption of a convexity arachnoid cyst associated with intracystic hemorrhage and subdural hematoma: A case report. 30-Jun-2023;14:224
How to cite this URL: Sho Hanai1, Kiyoyuki Yanaka1, Hitoshi Aiyama1, Michihide Kajita1, Eiichi Ishikawa2. Spontaneous resorption of a convexity arachnoid cyst associated with intracystic hemorrhage and subdural hematoma: A case report. 30-Jun-2023;14:224. Available from: https://surgicalneurologyint.com/surgicalint-articles/12387/
Abstract
Background: Intracranial arachnoid cysts (ACs) are developmental anomalies usually filled with cerebrospinal fluid (CSF), rarely resolving throughout life. Here, we present a case of an AC with intracystic hemorrhage and subdural hematoma (SDH) that developed after a minor head injury before gradually disappearing. Neuroimaging demonstrated specific changes from hematoma formation to AC disappearance over time. The mechanisms of this condition are discussed based on imaging data.
Case Description: An 18-year-old man was admitted to our hospital with a head injury caused by a traffic accident. On arrival, he was conscious with a mild headache. Computed tomography (CT) revealed no intracranial hemorrhages or skull fractures but an AC was seen in the left convexity. One month later, follow-up CT scans showed an intracystic hemorrhage. Subsequently, an SDH appeared then both the intracystic hemorrhage and SDH gradually shrank, with the AC disappearing spontaneously. The AC was considered to have disappeared, along with the spontaneous SDH resorption.
Conclusion: We present a rare case where neuroimaging demonstrated spontaneous resorption of an AC combined with intracystic hemorrhage and SDH over time, which may provide new insights into the nature of adult ACs.
Keywords: Arachnoid cyst, Spontaneous resorption, Subdural hematoma
INTRODUCTION
Intracranial arachnoid cysts (ACs) are benign congenital entities filled with cerebrospinal fluid (CSF) but may also contribute to risks of subdural hematoma (SDH) development after head trauma.[
CASE DESCRIPTION
An 18-year-old man experienced a high-speed automobile crash and was transported to our hospital by ambulance. On admission, the patient was alert, with no neurologic deficits, but reported a mild headache and dizziness. He had no remarkable medical or family histories.
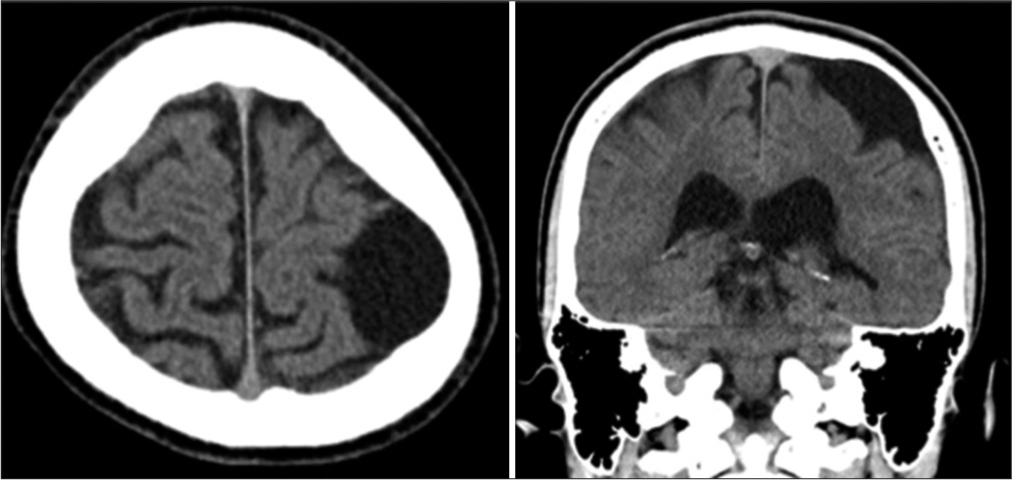
Computed tomography (CT) revealed a low-density cystic lesion with bone thinning on the left convexity [
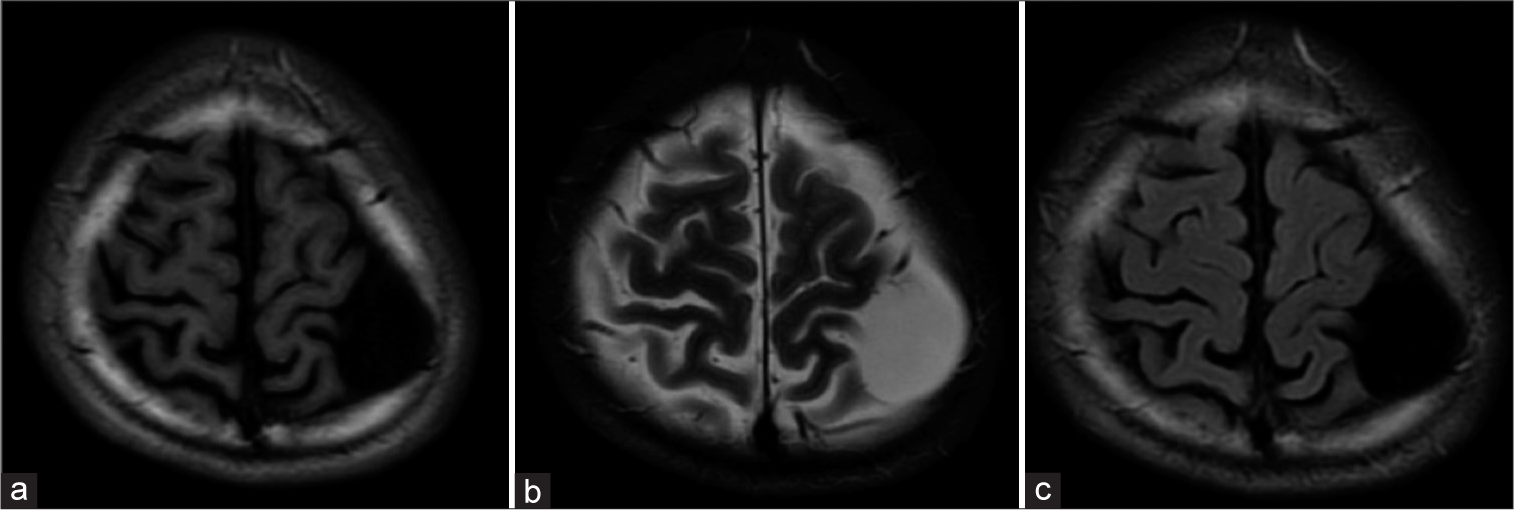
Approximately 1 month post-injury, the patient returned to the outpatient clinic with a mild headache. At that time, the AC appeared as a high-density lesion on CT images, suggesting intracystic hemorrhaging [
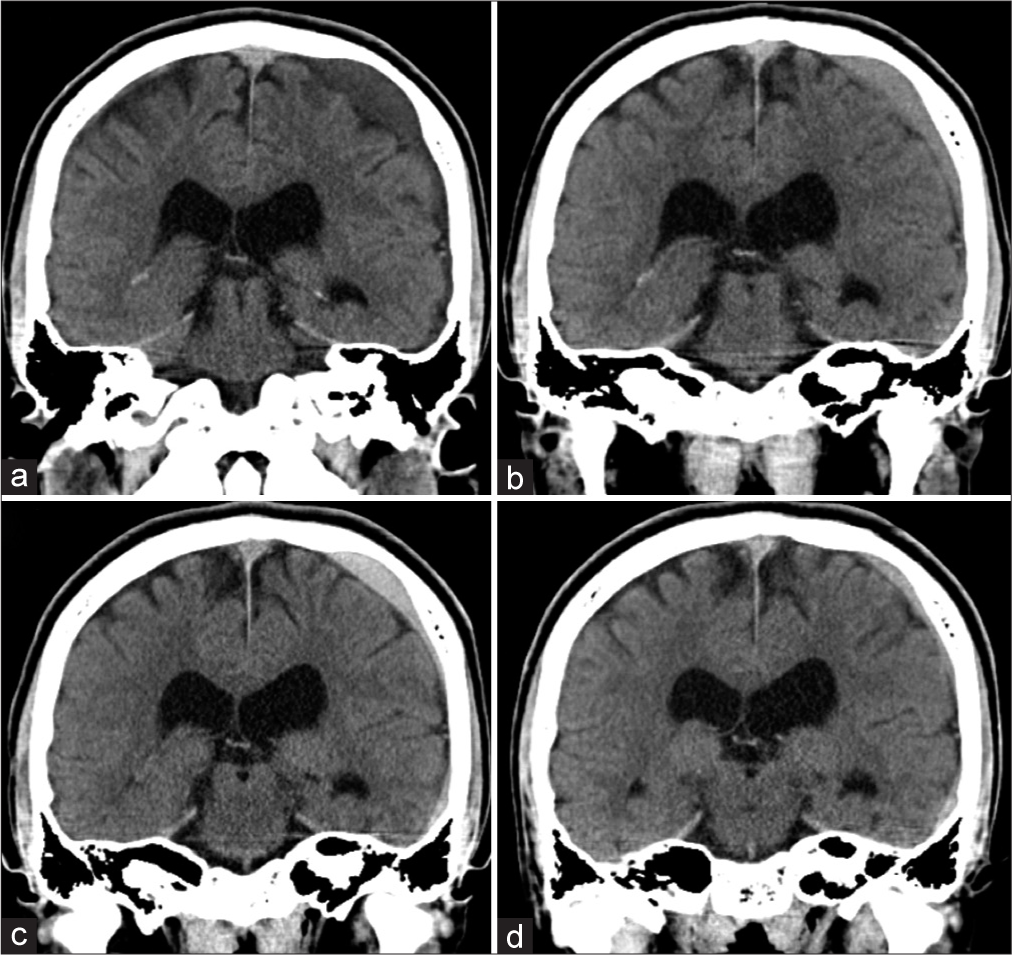
Figure 3:
Computed tomograms, showing changes in arachnoid cysts (ACs), the intracystic hemorrhage, and subdural hematoma (SDH) over time (a: 4 weeks, b: 6 weeks, c: 8 weeks, and d: 10 weeks after injury). The intracystic hemorrhage occurred first and the cystic component spread into the subdural space forming an SDH, where it was gradually absorbed while the AC disappeared simultaneously.
DISCUSSION
ACs are often found incidentally on neuroimaging and their spontaneous enlargement or disappearance is rare.[
It is generally thought that spontaneous resorption may occur due to ruptures of the cyst wall and drainage of cyst components into the subdural space.[
It is well known that AC is sometimes complicated by SDH or subdural hygroma, with Wester and Helland reporting that 4.6% of ACs lead to the development of subdural or intracystic hematomas.[
When an AC is accompanied by hemorrhaging, the hemorrhage can be intracystic only or with SDH; however, the mechanisms of such difference are unknown. Iaconetta et al. reviewed 37 ACs with intracystic hemorrhages, most of which (21/37 cases; 57%) were accompanied by SDHs.[
Once formed, SDHs often increase in size and become symptomatic. Patients with severe brain atrophy, liver and blood diseases, and those taking antiplatelet drugs are most likely to develop symptoms and usually require surgery. In our case, the patient was young and without brain atrophy; the SDH and AC resolved without surgical intervention. Bristol et al. reported that rupture of the middle fossa AC is more likely to be symptomatic, while such ruptures in other areas tend to be asymptomatic and resolve spontaneously.[
Most ACs are stable throughout life and do not require surgical treatment but, in some cases, they can be associated with hematomas and require surgical intervention.[
This report is a case report, so more cases are needed to estimate the guideline for treating the cases like our case. Our case may help the future treatment of ACs.
CONCLUSION
We presented a rare case of AC with intracystic hemorrhage and SDH formation that disappeared spontaneously over time, demonstrated by neuroimaging. This case may provide new insight into the nature of hematoma development associated with ACs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors would like to thank Dr. Alexander Zaboronok of the University of Tsukuba Faculty of Medicine Department of Neurosurgery for professional and language revision and Dr. Bryan J. Mathis of the University of Tsukuba Hospital International Medical Center for language revision.
References
1. Al-Holou WN, Terman S, Kilburg C, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in adults. J Neurosurg. 2013. 118: 222-31
2. Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr. 2010. 5: 578-85
3. Bristol RE, Albuquerque FC, McDougall C, Spetzler RF. Arachnoid cysts: Spontaneous resolution distinct from traumatic rupture. Case report. Neurosurg Focus. 2007. 22: E2
4. Haddad G, Alam R, Atweh LA, Hourani M. What provokes a disappearing arachnoid cyst?-Case study and literature review. Clin Imaging. 2022. 82: 193-7
5. Iaconetta G, Esposito M, Maiuri F, Cappabianca P. Arachnoid cyst with intracystic haemorrhage and subdural haematoma: Case report and literature review. Neurol Sci. 2006. 26: 451-5
6. Kikuchi A, Chernov M, Hagiwara S, Ohbuchi H, Kubota Y, Kasuya H. Resolution of the large middle fossa arachnoid cyst without any identifiable cause: Case report. J Clin Neurosci. 2021. 88: 147-9
7. Kim DY, Lee S, Choi BS, Kim JS. Spontaneous disappearance of an arachnoid cyst after burr hole drainage of chronic subdural hematoma. Korean J Neurotrauma. 2019. 15: 159-63
8. Kwak YS, Hwang SK, Park SH, Park JY. Chronic subdural hematoma associated with the middle fossa arachnoid cyst: Pathogenesis and review of its management. Childs Nerv Syst. 2013. 29: 77-82
9. Lim JW, Choi SW, Song SH, Kwon HJ, Koh HS, Youm JY. Is arachnoid cyst a static disease? A case report and literature review. Childs Nerv Syst. 2019. 35: 385-8
10. Massimi L, Bianchi F, Benato A, Frassanito P, Tamburrini G. Ruptured Sylvian arachnoid cysts: An update on a real problem. Childs Nerv Syst. 2023. 39: 93-119
11. Nadi M, Nikolic A, Sabban D, Ahmad T. Resolution of middle fossa arachnoid cyst after minor head trauma-stages of resolution on MRI: Case report and literature review. Pediatr Neurosurg. 2017. 52: 346-50
12. Park SH, Lee SH, Park J, Hwang JH, Hwang SK, Hamm IS. Chronic subdural hematoma preceded by traumatic subdural hygroma. J Clin Neurosci. 2008. 15: 868-72
13. Patel AP, Oliverio PJ, Kurtom KH, Roberti F. Spontaneous subdural hematoma and intracystic hemorrhage in an arachnoid cyst. Radiol Case Rep. 2009. 4: 298
14. Taillibert S, Le Rhun E, Chamberlain MC. Intracranial cystic lesions: A review. Curr Neurol Neurosci Rep. 2014. 14: 481
15. Wester K, Helland CA. How often do chronic extra-cerebral haematomas occur in patients with intracranial arachnoid cysts?. J Neurol Neurosurg Psychiatry. 2008. 79: 72-5
16. Zhang T, Li Z, Gong W, Sun B, Liu S, Zhang K. Percutaneous fibrin glue therapy for meningeal cysts of the sacral spine with or without aspiration of the cerebrospinal fluid. J Neurosurg Spine. 2007. 7: 145-50