- Department of Neurosurgery, Dubrava University Hospital,
- Primary respiratory intensive care centre, Dubrava University Hospital,
- Department of Diagnostic and Interventional Radiology, Dubrava University Hospital,
- Department of Surgery, Dubrava University Hospital, University of Zagreb School of Medicine,
- Department of Maxillofacial Surgery, Dubrava University Hospital, University of Zagreb School of Medicine,
- Catholic University of Croatia, School of Medicine, Zagreb, Croatia.
Correspondence Address:
Marina Raguz, Department of Neurosurgery, University Hospital Dubrava, Zagreb, Croatia.
DOI:10.25259/SNI_87_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Domagoj Dlaka1,2, Hrvoje Vavro2,3, Dominik Romić1,2, Fadi Almahariq1,2, Darko Chudy1,2,4, Ivica Lukšić2,5, Marina Raguž1,2,6. Spontaneous spinal subdural hematoma in COVID-19 patient: Croatian national COVID hospital experience. 02-Sep-2022;13:394
How to cite this URL: Domagoj Dlaka1,2, Hrvoje Vavro2,3, Dominik Romić1,2, Fadi Almahariq1,2, Darko Chudy1,2,4, Ivica Lukšić2,5, Marina Raguž1,2,6. Spontaneous spinal subdural hematoma in COVID-19 patient: Croatian national COVID hospital experience. 02-Sep-2022;13:394. Available from: https://surgicalneurologyint.com/surgicalint-articles/11848/
Abstract
Background: Spontaneous spinal subdural hematoma (SSDH) is a rare condition and causes of acute spinal cord compression, with symptoms varying from mild to severe neurological deficit. SSDH could occur as a consequence of posttraumatic, iatrogenic, or spontaneous causes, including underlying arteriovenous malformations, tumors, or coagulation disorder. Due to its rarity, it is difficult to establish standardized treatment. We present a rare case of SSDH in COVID-19 patient and course of treatment in COVID hospital.
Case Description: A 71-year-old female patient was admitted due to instability, weakness of the left leg, and intensive pain in the upper part of thoracic spine as well as mild respiratory symptoms of COVID-19. She was not on pronounced anticoagulant therapy and her coagulogram at admission was within normal range. MRI revealed acute subdural hematoma at the level C VII to Th III compressing the spinal cord. The patient underwent a decompressive Th I and Th II laminectomy and hematoma evacuation. Post-operative MRI revealed a satisfactory decompression and re-expansion of the spinal cord. COVID-19 symptoms remained mild.
Conclusion: SSDH represents a neurological emergency, possibly leading to significant deficit and requires urgent recognition and treatment. One of the main difficulties when diagnosing is to consider such condition when there is no history of anticoagulant treatment or previous trauma. Since high incidence of coagulation abnormalities and thromboembolic events was described COVID-19 patients, when considering the pathology of the central nervous system, the bleeding within it due to COVID-19 should be taken into account, in both brain and spine.
Keywords: COVID-19, Neurosurgery, Spontaneous spinal subdural hematoma
INTRODUCTION
Coronavirus disease 2019 (COVID-19) stands for novel infection that led to worldwide pandemic, caused by Severe Acute Respiratory Syndrome CoronaVirus-2 (SARS-Cov2). Different clinical outcomes have been observed in patients, ranging from asymptomatic, mild or moderate disease to severe, and progressive pneumonia leading to acute respiratory distress syndrome and multisystem organ failure.[
Spontaneous spinal subdural hematoma (SSDH), a rare acute or subacute condition and cause of acute spinal cord compression accounting approximately for 4.1% of spinal hematomas, was firstly reported in 1948 by Schiller et al.[
Hereby, we present a rare case of SSDH in COVID-19 patient and course of treatment in Croatian national COVID hospital.
CASE DESCRIPTION
History
A 71-year-old female patient was admitted due to dizziness, instability, and intensive pain in the upper part of thoracic spine. Initial neurological examination revealed the left leg monoparesis, lower extremity reflexes were lively presented, accompanied with positive Babinski sign on the left. Initial brain CT was unremarkable and initial chest X-ray revealed no inflammation infiltrates; thoracic spine and pelvis CT revealed degenerative changes that corresponded to age.
At the admission, she was tested with fast antigen SARSCoV-2 and SARS-CoV-2 RT PCR test (three sequences), both tests were positive. The patient had mild respiratory symptoms of COVID-19 and was afebrile.
Before admission, the patient was taking acetylsalicylic acid 100 mg due to stents implanted more than 10 years ago, and in hospital 0.3 ml of Clexane was administered daily. Coagulogram at the admission was inside normal range (D-dimers 0.66, CRP 1.8). Within 3 days from admission, she developed left leg plegia, severe right leg paresis, and hypoesthesia at the Th10 level on the left and at the Th8 level on the right side and was not able to control the sphincters.
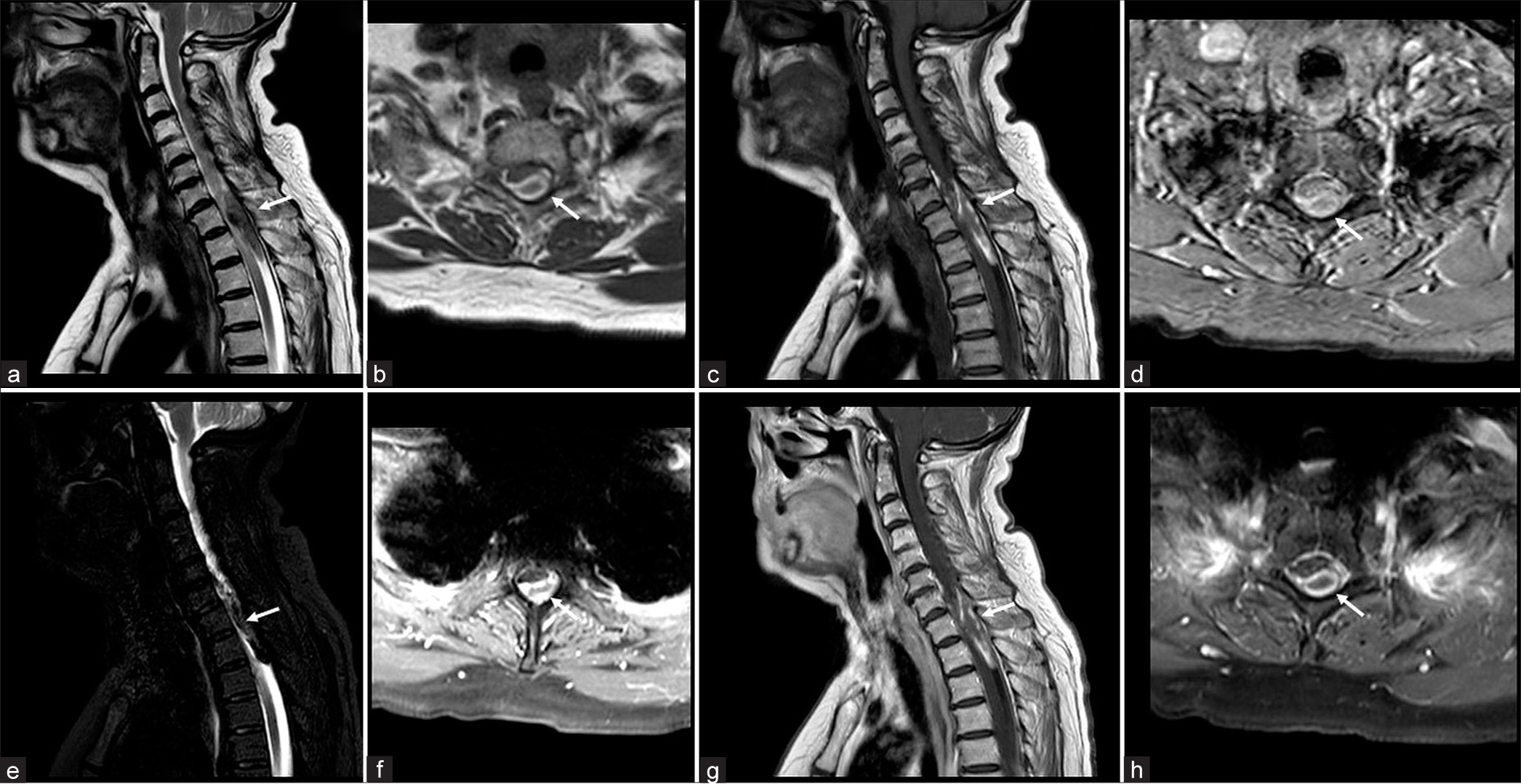
MRI revealed acute subdural hematoma at the level C VII to Th III, length 55 mm and 6 mm thick; in segments C V to Th III the elevated spinal cord signal corresponds to compression myelopathy [
Figure 1:
Initial MRI of the cervical and proximal thoracic spine. Sagittal T2WI (a), axial T2WI (b), sagittal T1WI (c), axial T1WI (d), sagittal STIR (e), and axial STIR (f) images demonstrate an inhomogeneous intradural extramedullary collection in the posterior spinal canal at levels C VII to Th III, compressing the spinal cord. There is also some T1-hyperintense material in the anterior subdural space. Postcontrast sagittal T1wi (g) and axial FS T1WI (h) do not demonstrate any contrast enhancement. The hematoma location is marked with white arrow in all images.
Operation
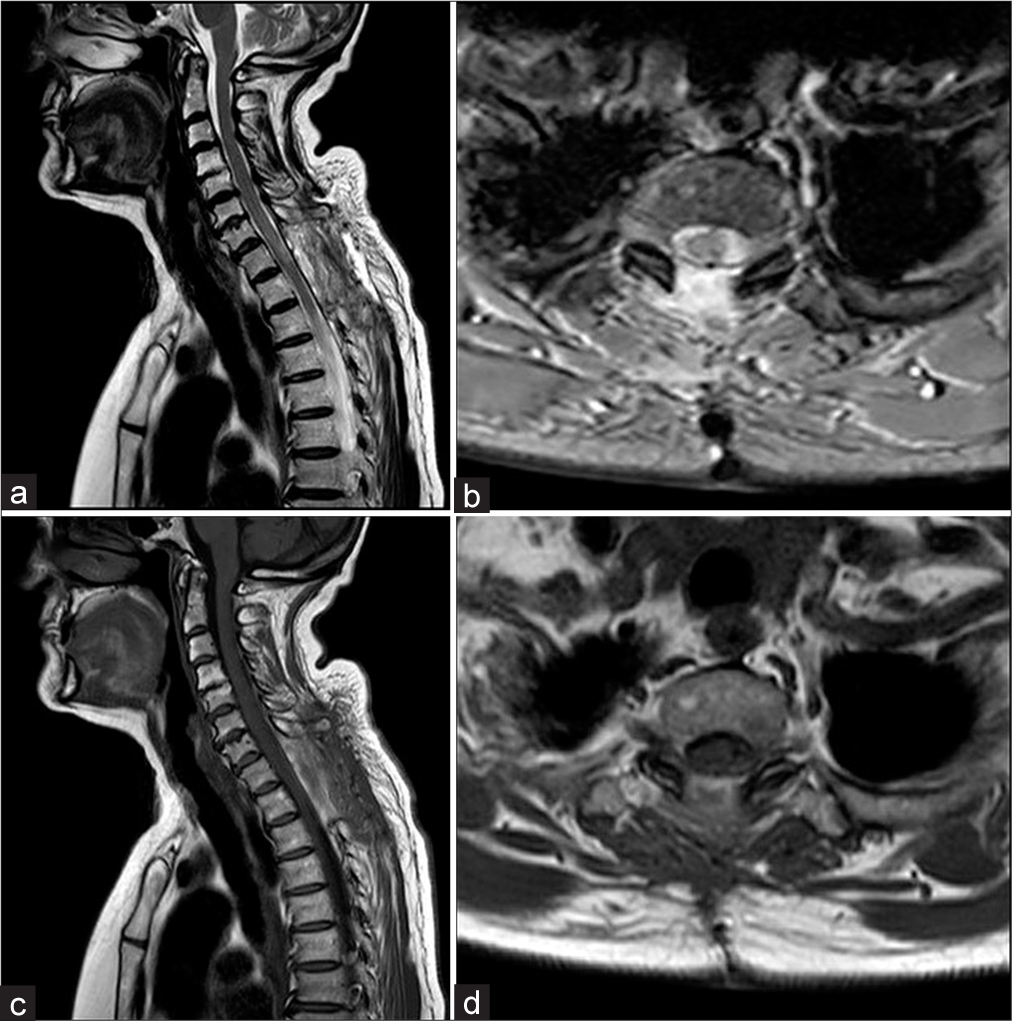
The patient underwent a decompressive laminectomy of levels Th I and Th II. After subdural hemorrhage evacuation, a small coil of thrombosed blood vessels partially adherent to the arachnoid and thoracic roots laterally was completely removed without any damage to the neural structure. The surgery went without any complications. Postoperative MRI revealed a satisfactory postoperative finding, including good decompression and re-expansion of the spinal cord with regression of myelopathy [
Postoperative course
Postoperatively, CRP levels were increased, with peak of 41.9 on 2nd postoperative day, and lowering to 1.8, while the levels of D-dimers were also increased (> 4.37) and persisted until discharge. The left leg was paretic with movements in knee joint and foot, right leg recovered completely, while full control of the sphincters was not regained. COVID-19 symptoms remained mild. The patient was further appointed to stationary medical rehabilitation.
DISCUSSION
SSDH is a rare, uncommon condition characterized by a sudden onset of headache, back pain, or radicular pain and has rapid progression of spinal cord compression symptoms such as sensorimotor change, autonomous function, and neurogenic bladder.[
Although only several spontaneous cases were described in literature, to the best of our knowledge, this is the one of a very few cases described in COVID-19 patient.[
The determination of the SSDH pathogenesis is very challenging. Although several different theories were previously suggested, it has been generally accepted that SSDH may originate from within the subdural space, or due to subarachnoid vessels rupture in the subdural space, following an acute rise of abdominal or intrathoracic pressure, such as yawning or coughing.[
It has been described that approximately 70% of COVID-19 treated patients developed coagulation abnormalities and autopsy revealed almost 58% of patients died due to venous thrombosis and pulmonary embolism.[
Although the detailed molecular mechanism of SARS-CoV-2-mediated hypercoagulation is unclear, it has been discussed that COVID-19 infection could induce coagulation disorder leading to overt clot formation, pulmonary embolism, and serious effects on patient recovery and survival[
When symptoms suggest a spinal cord compression due to a spinal hematoma, MRI appears to be the gold standard and the modality of choice, providing information on the exact level of the hematoma, degree of nervous structures compression, and consequence for the spinal cord.[
CONCLUSION
SSDH represents a neurological emergency, possibly leading to significant deficit and requires urgent recognition and treatment. One of the main difficulties when diagnosing is to consider such condition when there is no history of anticoagulant treatment or the previous trauma. Since it has been shown that COVID-19 increases the incidence of thromboembolic incidents, when considering the pathology of the central nervous system, the bleeding within it due to COVID-19 should be taken into account, not only in the brain but also in the spine.
Compliance with ethical standards
The patient has given informed consent for participation in this paper.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Samkari H, Leaf RS, Dzik WH, Carlson JC, Fogerty AE, Waheed A. COVID-19 and coagulation: Bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020. 136: 489-500
2. Biswas I, Khan GA. Coagulation disorders in COVID-19: Role of toll-like receptors. J Inflamm Res. 2020. 13: 823-28
3. Benyaich Z, Laghmari M, Lmejjati M, Aniba K, Ghannane H, Benali SA. Acute lumbar spinal subdural hematoma inducing paraplegia after lumbar spinal manipulation: Case report and literature review. World Neurosurg. 2019. 128: 182-85
4. Chen N, Zhou M, Dong X, Qui J, Yu T, Liu Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020. 395: 507-13
5. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020. 135: 2033-40
6. De Beer MH, Smeets MM, Koppen H. Spontaneous spinal subdural hematoma. Neurologist. 2017. 22: 34-9
7. Domenicucci M, Ramieri A, Paolini S, Russo N, Occhiogrosso G, Di Biasi C. Spinal subarachnoid hematomas: Our experience and literature review. Acta Neurochir (Wien). 2005. 147: 741-50
8. Faiek S, Wazzan NI, Sompalli S, Bansal A, Hota P. A rare case presentation of apixaban-induced nontraumatic spinal subdural hematoma. Cureus. 2020. 12: e6743
9. Goyal J, Mishra V, Sharma M, Bullagan A. Spontaneous spinal sub-dural hematoma: A rare complication in severe Covid-19 disease. Int J Curr Res. 2021. 13: 18131-3
10. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. 395: 497-06
11. Jimbo H, Asamoto S, Mitsuyama T, Hatayama K, Iwasaki Y, Fukui Y. Spinal chronic subdural hematoma in association with anticoagulant therapy: A case report and literature review. Spine (Phila Pa 1976). 2006. 31: E184-7
12. Joubert C, Gazzola S, Sellier A, Dagain A. Acute idiopathic spinal subdural hematoma: What to do in an emergency?. Neurochirurgie. 2019. 65: 93-7
13. Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020. 191: 145-47
14. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003. 26: 1-49
15. Lim SW, Wong E. Spontaneous epidural hematoma of the cervical spine in an elderly woman with recent COVID-19 infection: A case report. Am J Case Rep. 2020. 21: e926784
16. Pereira BJ, De Almeida AN, Muio VM, De Oliveira JG, De Holanda CV, Fonseca NC. Predictors of outcome in nontraumatic spontaneous acute spinal subdural hematoma: Case report and literature review. World Neurosurg. 2016. 89: 574-7
17. Rettenmaier LA, Holland MT, Abel TJ. Acute, nontraumatic spontaneous spinal subdural hematoma: A case report and systematic review of the literature. Case Rep Neurol Med. 2017. 2017: 2431041
18. Schiller F, Neligan G, Budtz-Olsen O. Surgery in haemophilia: A case of spinal subdural haematoma producing paraplegia. Lancet. 1948. 2: 842-5
19. Vastani A, Mirza AB, Lavrador JP, Boardman TM, Khan MF, Malik I. Risk factor analysis and surgical outcomes of acute spontaneous spinal subdural hematoma. An institutional experience of four cases and literature review. World Neurosurg. 2021. 146: e384-97
20. Wang B, Liu W, Zeng X. Idiopathic cervical spinal subdural haematoma: A case report and literature review. J Int Med Res. 2019. 47: 1365-72
21. Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A. Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Intern Med. 2020. 173: 268-77