- Department of Neurosurgery, Sher-i- Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
- Department of Pathology, Sher-i- Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
Correspondence Address:
Abrar A. Wani
Department of Pathology, Sher-i- Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
DOI:10.4103/2152-7806.196928
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abrar A. Wani, Uday K. Raswan, Nayil K. Malik, Altaf U. Ramzan, Iqbal Lone. Squamous cell carcinoma arising from neglected meningocele. 28-Dec-2016;7:
How to cite this URL: Abrar A. Wani, Uday K. Raswan, Nayil K. Malik, Altaf U. Ramzan, Iqbal Lone. Squamous cell carcinoma arising from neglected meningocele. 28-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/squamous-cell-carcinoma-arising-from-neglected-meningocele/
Abstract
Background:A neural tube defect (NTD) is a common congenital anomaly with an incidence of 6.57–8.21 per 1000 live births. Patients usually present early because of obvious swelling or due to neurological deficit. However, neglecting the obvious cystic swelling on the back till its transformation into malignant tumor is rare.
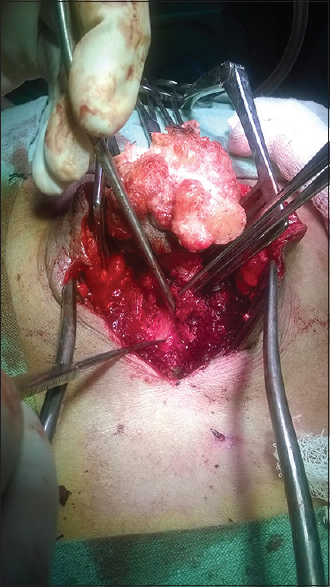
Case Description:We describe a case of malignant transformation of meningocele in a 60-year-old man. Magnetic resonance imaging showed sacral meningocele. Neurological examination revealed intact motor and sensory examination with normal bladder and bowel function. There were no signs of meningitis and hydrocephalus. Excision was done and biopsy revealed it as squamous cell carcinoma.
Conclusion:Meningocele should be treated early and possibility of malignant change should be kept in mind in neglected cases presenting in adulthood.
Keywords: Adult, meningocele, neural tube defects, squamous cell carcinoma
INTRODUCTION
A neural tube defect (NTD) is a common congenital anomaly with an incidence of 6.57–8.21 per 1000 live births.[
CASE REPORT
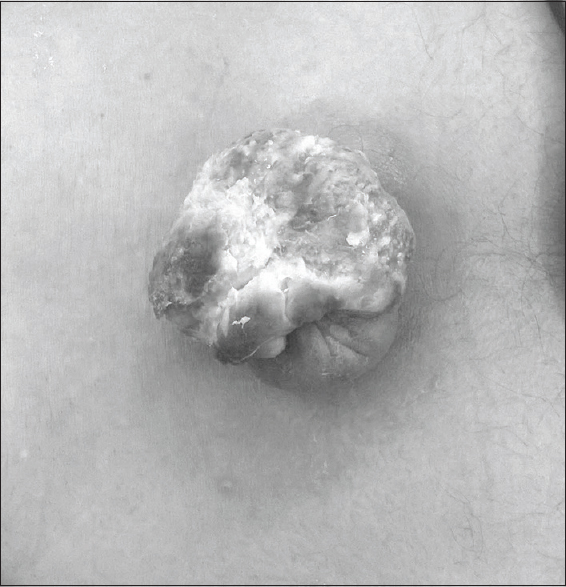
A 60-year-old man presented with complaints of discharge from a swelling in the sacral area. At the time of birth he was noted to have a sacral meningocele for which he was advised surgery, however, his family had refused and the wound surface slowly became abraded and exudated repeatedly over a period of years. One month before the admission, the swelling started discharging foul smelling fluid and increased in size. Inspection showed a swelling in the sacral region of 5 cm in diameter, consisting of cauliflower-shaped swelling with yellowish slough [
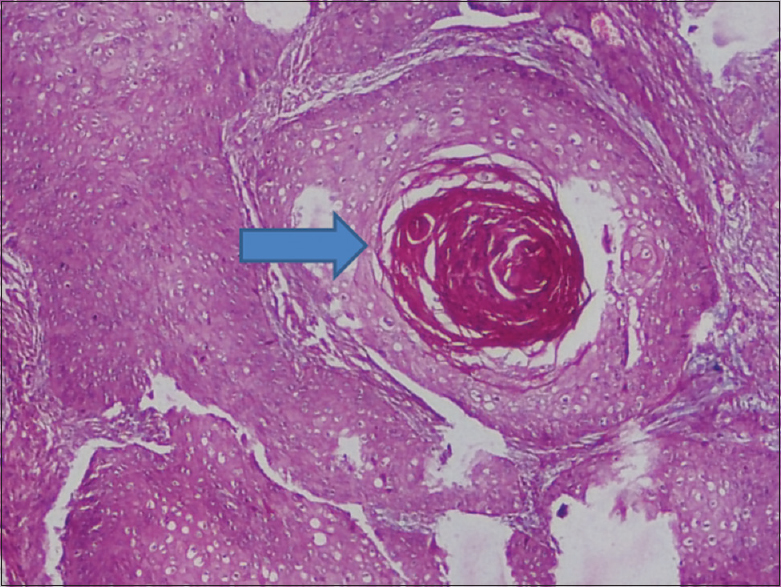
Pathological finding
The tissue sections were stained in hematoxylin and eosin (H and E) stain, and the histopathology study revealed tumor cells arranged in sheets and nests with keratin pearl formation [
Postoperative course
The postoperative recovery was uneventful and the wounds healed by primary intention. Further, the patient was sent to the oncology department for adjuvant therapy. Postoperatively, the patient has been on follow-up for a year without any recurrence.
DISCUSSION
A meningocele is a congenital anomaly of neural arch fusion in association with an open neural tube defect, and is characterized by protrusion of spinal meninges which contain cerebrospinal fluid without involvement of the neural tissue. Most meningoceles are surgically repaired during the new-born period or at least in childhood. The incidence of survival is low without intervention, and hence, adult meningoceles are rarely seen. Life expectancy at birth is shorter in myelomeningocele patients, although effective treatment for hydrocephalus and intermittent catheterization for the management of the neurogenic bladder can improve the quality of life for these patients. Posterior lumbosacral meningocele cases have rarely been reported. The long-term follow up results for adults with sacral myelomeningocele are not as good as in children because other neurological abnormalities such as hydromyelia, syringomyelia, tethered cord, Chiari malformations, and hydrocephalus accompany this lesion.[
A search of the literature revealed four cases similar to the one we have described. Saskun et al.[
MRI is a good investigation choice for evaluating the meningocele sac in the sagittal plane, and to observe the spinal cord itself, as well as the possible congenital anomalies associated with it.[
One must be aware of possible neoplastic change in untreated meningomyelocele after years of mechanical irritation and chronic bacterial infection. This seems to be a probable cause in our case. The defect, lacking a protective epithelial cover, must be viewed regularly with a high degree of suspicion, as with other chronic ulcers. Squamous cell carcinoma is a well-known complication of burn and chronic venous ulcer, pilonidal sinuses, longstanding bacterial and fungal infections, vaccination scars, and even tattoos.[
Once change is noted, biopsies should be done to establish a histological diagnosis. If malignancy is established, an intensive search for metastases, lymph node involvement, and local invasion must be made for proper staging and subsequent treatment.[
CONCLUSION
In conclusion, meningocele should be treated as soon as diagnosed and possibility of malignant change should be kept in mind in neglected cases presenting in adulthood.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cherian A, Serena S, Bullock RK, Antony AC. Incidence Of Neural Tube Defects In The Least-Developed Area Of India: A Population-Based Study. Lancet. 2005. 366: 930-1
2. Duan HZ, Zhang Y, Zhang JY, Bao SD, Zhou CQ. A Case Report of Squamous Cell Carcinoma Arising In a Patient with Meningomyelocele. Beijing Da Xue Xue Bao. 2009. 41: 489-91
3. Laharwal MA, Sarmast AH, Ramzan AU, Wani AA, Malik NK, Arif SH. Epidemiology of the neural tube defects in Kashmir valley. Surg Neurol Int. 2016. 7: 35-
4. Ozdemir NG, Atci IB, Antar V, Yllmaz H, Bitirak G, Katar S. Lumbosacral Meningocele In Adulthood. Cukurova Med J. 2015. 40: 131-5
5. Pope M, Todorov AB. Cutaneous squamous cell carcinoma as a rare complication of cervical meningocele. Birth Defects. 1975. 11: 336-
6. Saskun JM, Fisher BK. Squamous Cell Carcinoma Arising In a Meningomyelocele. Can Med Assoc J. 1978. 119: 739-41
7. Thorp RH. Carcinoma Associated With Myelomeningocele. Case Report. J Neurosurg. 1967. 27: 446-8