- Department of Neurology, Tokushima University Graduate School of Biomedical Sciences, Tokushima, Japan.
- Department of Neurosurgery, Tokushima University Graduate School of Biomedical Sciences, Tokushima, Japan.
Correspondence Address:
Yuki Yamamoto, Department of Neurology, Tokushima University Graduate School of Biomedical Sciences, Tokushima, Japan.
DOI:10.25259/SNI_513_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuki Yamamoto1, Nobuaki Yamamoto1, Tomohiro Matsuda2, Kazutaka Kuroda1, Izumi Yamaguchi2, Shu Sogabe2, Masaaki Korai2, Kenji Shimada2, Yasuhisa Kanematsu2, Yasushi Takagi2, Yuishin Izumi1. Stent retrieval for free-floating thrombus attached to carotid artery stenosis: A report of two cases. 04-Aug-2023;14:274
How to cite this URL: Yuki Yamamoto1, Nobuaki Yamamoto1, Tomohiro Matsuda2, Kazutaka Kuroda1, Izumi Yamaguchi2, Shu Sogabe2, Masaaki Korai2, Kenji Shimada2, Yasuhisa Kanematsu2, Yasushi Takagi2, Yuishin Izumi1. Stent retrieval for free-floating thrombus attached to carotid artery stenosis: A report of two cases. 04-Aug-2023;14:274. Available from: https://surgicalneurologyint.com/surgicalint-articles/12486/
Abstract
Background: We report two cases who underwent mechanical thrombectomy using a stent retriever in advance of urgent carotid artery stenting (CAS) for carotid artery stenosis with free-floating thrombus (FFT).
Case Description: Two patients showing symptomatic carotid artery stenosis with FFT underwent urgent endovascular surgery due to progressive neurological symptoms. The first case showed an FFT with 70% internal carotid artery (ICA) stenosis. After the completion of the common and external carotid artery balloon and distal ICA filter protection, we deployed a 6-mm-diameter stent retriever in the distal part of the stenosis. The white thrombus was retrieved; the angiographic shadow of the FFT disappeared; and CAS was performed. In the second case, due to a 90% severe stenosis lesion with FFT, balloon angioplasty was performed on the lesion using the push wire of the stent retriever. After angioplasty, the stent retriever was smoothly retrieved, and CAS was performed. Postoperative magnetic resonance imaging showed an increase in cerebral embolism in the first case; however, the patient’s neurological symptoms improved. The second case showed in-stent plaque protrusion and required two additional stent placements; the patient showed no worsening of his neurological symptoms.
Conclusion: In cases of carotid artery stenosis with FFT, it is technically possible to retrieve a thrombus with a stent retriever. Although thrombus removal may help reduce the risk of ischemic complications in a series of urgent CAS procedures, there are concerns such as mechanical irritation to the carotid artery plaque, and its indications and alternative treatments should be carefully considered.
Keywords: Carotid artery stenting, Free-floating thrombus, Mechanical thrombectomy, Stent retriever
INTRODUCTION
A free-floating thrombus (FFT) of the carotid artery is a rare condition in which a mobile thrombus adheres to the lesion against the background of plaque rupture and other conditions on the arterial wall.[
CASE DESCRIPTION
Case 1
Case 1 involved a 64-year-old man who began experiencing numbness in the right hand one morning. Scattered infarction in the left hemisphere and a stenotic lesion in the origin of the left internal carotid artery (ICA) were noted [
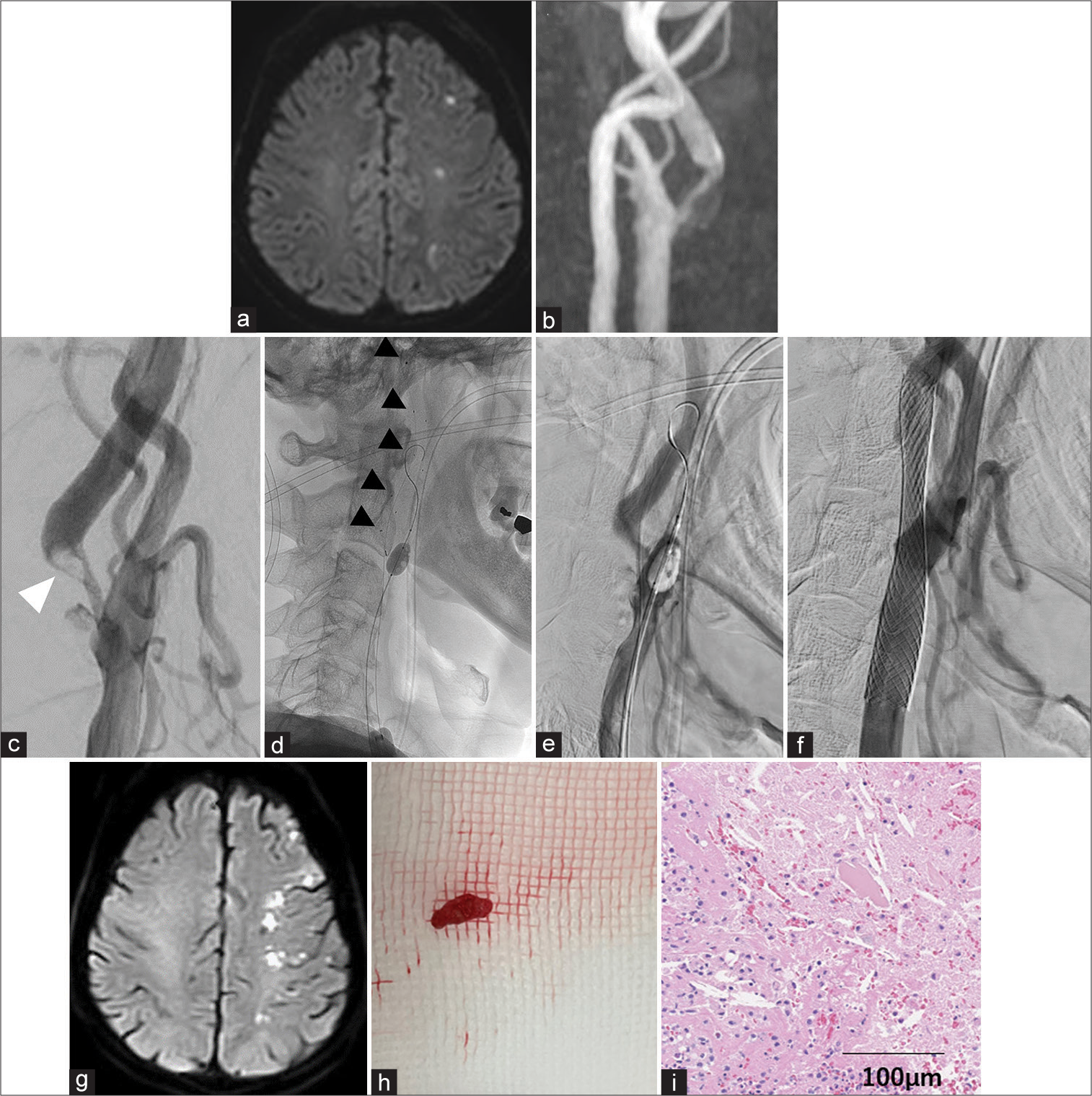
Figure 1:
A 64-year-old man with symptomatic left carotid artery stenosis and free-floating thrombus (FFT). (a) Magnetic resonance imaging (MRI) shows diffuse spotty infarctions in the left hemisphere. (b) MRA shows stenosis in the left internal carotid artery (ICA). (c) Digital subtraction angiography (DSA) shows moderate ICA stenosis with a FFT (white arrow). (d) Tron FX 6 × 50 mm (Microvention, Tustin, CA, USA, black arrows) is deployed to cover the thrombus. (e) After stent retriever retrieval, the thrombus image on DSA disappears. (f) Carotid Wallstent (Stryker, Kalamazoo, MI, USA) is deployed. (g) Postprocedural MRI shows increased diffuse infarcts. (h) White thrombus retrieved by the stent retriever. (i) Microscopic, the retrieved thrombi contain fibrin, red blood cells, inflammatory cells, and cholesteric clefts.
Case 2
Case 2 involved an 81-year-old man with a medical history of diabetes mellitus, atrial fibrillation, and coronary artery disease. He presented to our hospital with mild left-sided hemiparesis. MRI showed diffuse infarction in the right cerebral hemisphere and severe stenosis of right ICA origin [
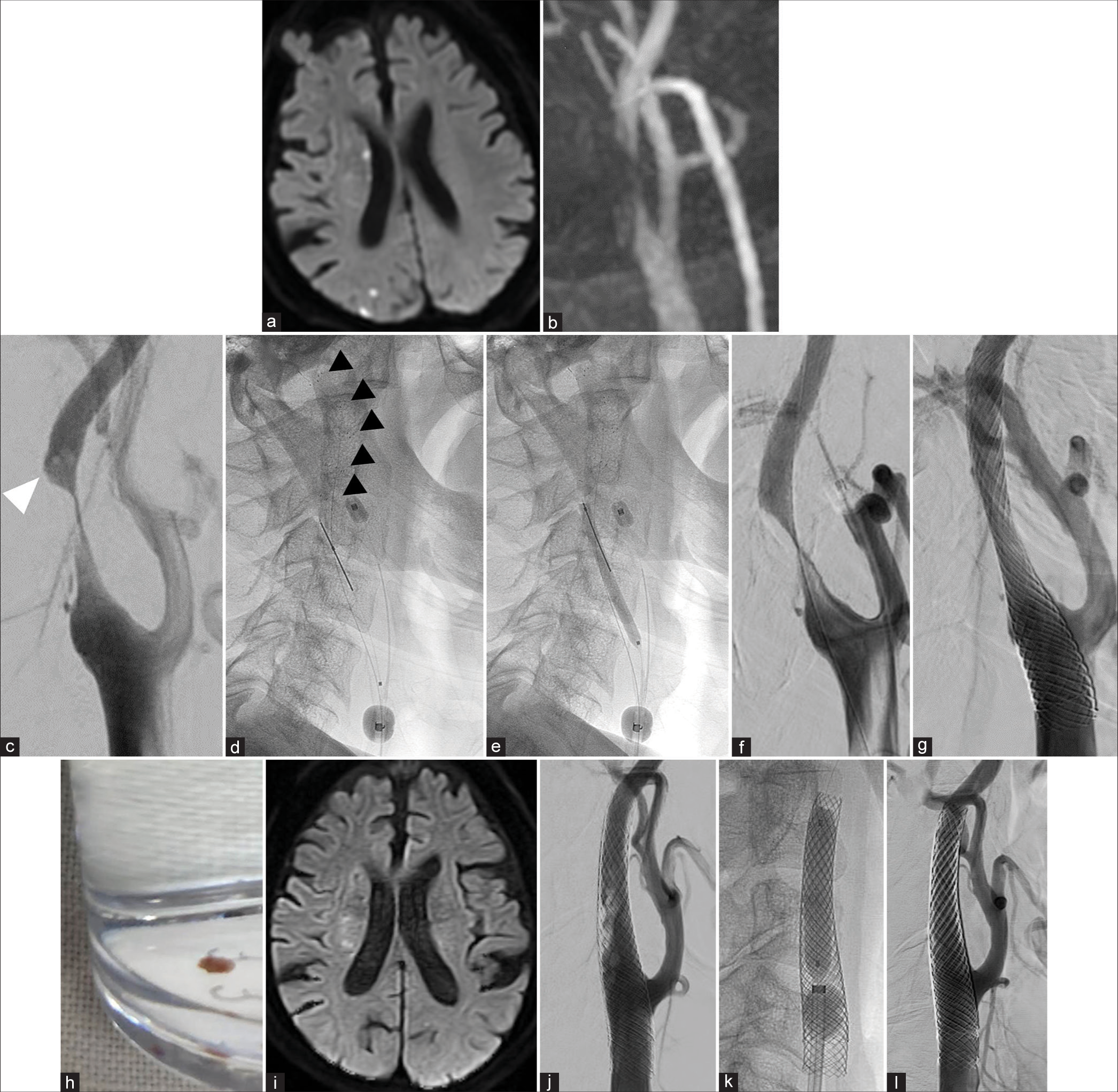
Figure 3:
An 81-year-old man with symptomatic right carotid artery stenosis and free-floating thrombus (FFT). (a) Magnetic resonance imaging (MRI) shows diffuse spotty infarctions in the patient’s right hemisphere. (b) MRA shows stenosis in right internal carotid artery (ICA). (c) Digital subtraction angiography (DSA) shows severe ICA stenosis with FFT (white arrow). (d) EMBOTRAP Ⅲ 6.5 × 44 mm (Johnson and Johnson, Miami, FL, USA, black arrows) is deployed to cover the thrombus. (e) A balloon dilatation catheter guided to the lesion along the push wire of the stent retriever is inflated. (f) After stent retriever retrieval, the thrombus image on DSA disappears. (g) Carotid Wallstent (Stryker, Kalamazoo, MI, USA) is deployed. (h) White thrombus retrieved by the stent retriever. (i) Postoperative MRI shows no increase in infarction. (j) DSA shows recurrence of in-stent plaque protrusion after additional stent placement. (k) Balloon dilation with proximal balloon protection and distal filter protection. (l) Final image after placement of the third stent (10 × 30 mm CASPER Rx, Microvention, Tustin, CA, USA).
DISCUSSION
FFT is described by several overlapping terms, such as intraluminal thrombus and mobile thrombus, but is generally defined as an elongated thrombus attached to the arterial wall and showing periodic motion associated with the cardiac cycle. A previous review reported that complete dissolution of the FFT, without any further neurologic progression, occurred in 86% of patients treated medically, including those who received anticoagulation and antiplatelet therapy.[
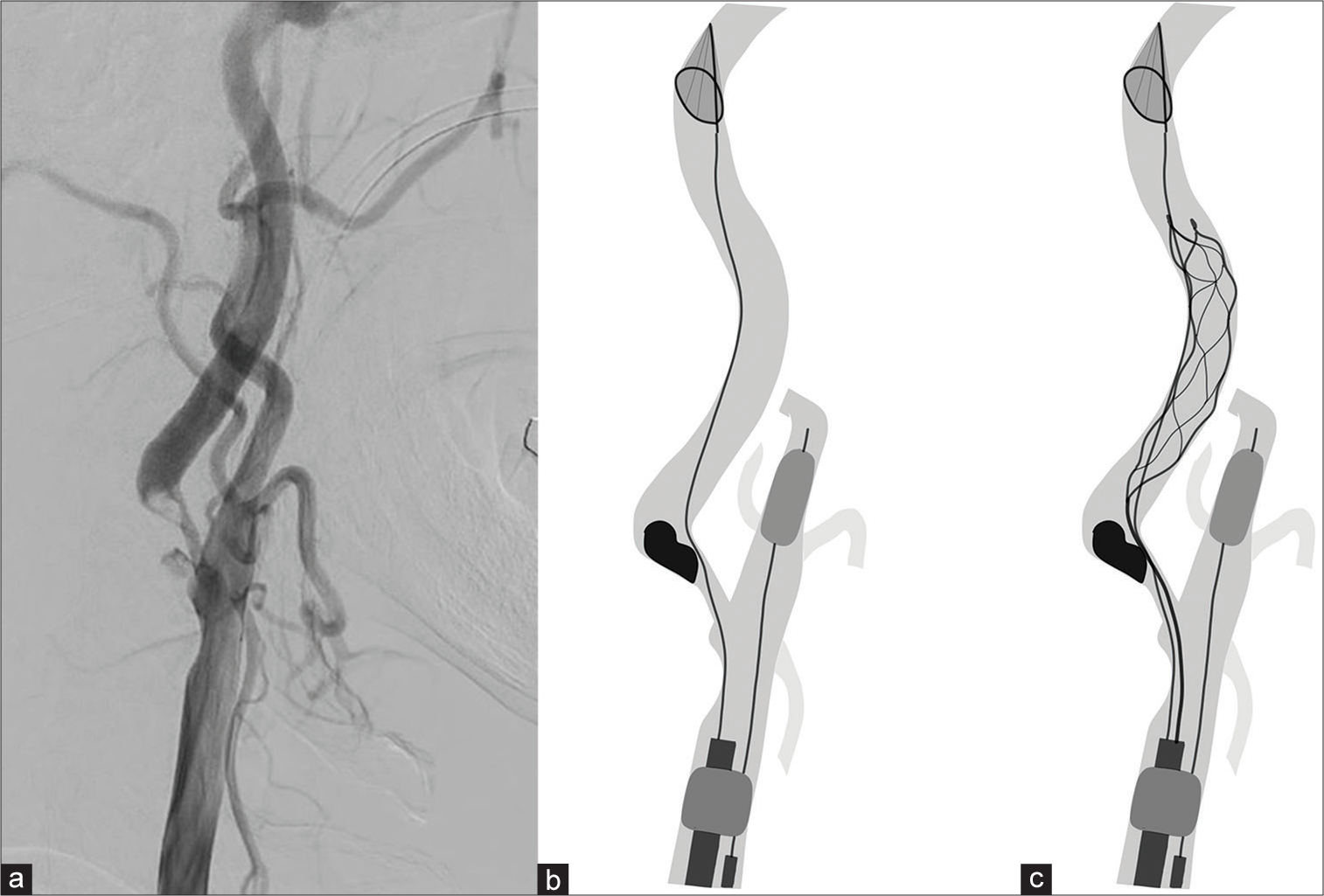
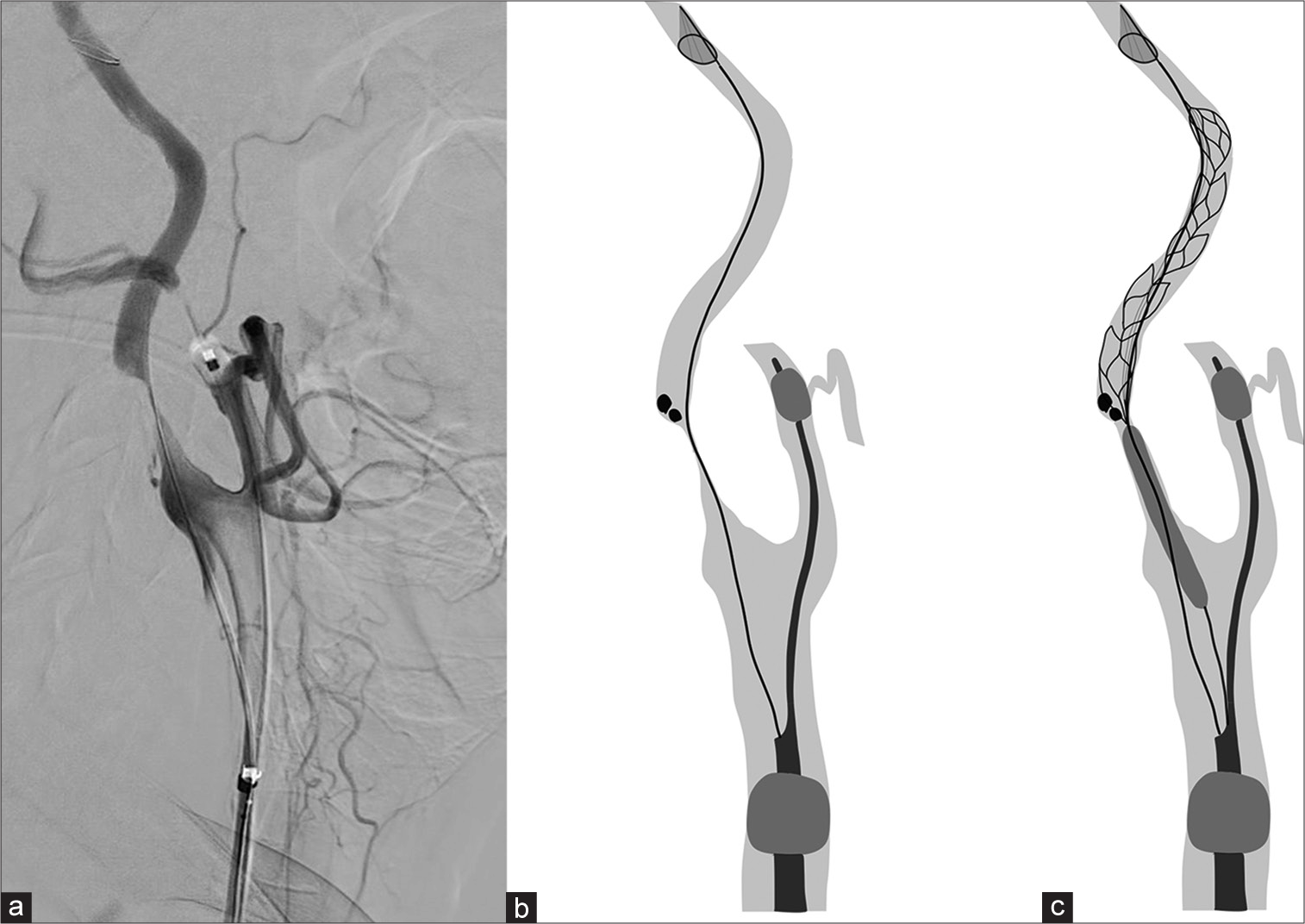
Successful thrombus retrieval using a stent retriever or aspiration catheter has been reported in cases involving FFT without moderate or severe stenotic lesions.[
In case 1, postoperative MRI showed an increase in embolic cerebral infarction compared to the initial image. Since the patient was transferred to digital subtraction angiography (DSA) without MRI after symptom exacerbation, it is possible that the infarction had already increased before the endovascular procedure. We attempted to prevent distal embolism as much as possible by blocking the ECA and CCA. In addition, since the blood flow from the superior thyroid artery remains even if the ECA is blocked, a distal ICA filter was used for distal protection in both cases. One of the problems with our method of removing floating thrombi with a stent retriever is the complexity of the procedure and the risk of technical complications. Interference between the distal filter and the stent retriever may make removal of the device difficult, and it is necessary to ensure that the filter can be placed enough distal to the petrous portion of the ICA. In our cases, the position of the filter did not change during stent retrieval; however, interference of both devices during retrieval should be careful. There is also concern that using multiple devices will lead to increased medical costs.
Another critical consideration in this procedure is mechanical damage to the carotid plaque surface due to stent retriever friction. In case 2, despite successful FFT retrieval, in-stent plaque protrusion occurred and required two additional sessions of stent placement. The use of a stent retriever for the case of ICA stenosis with fragile plaque may cause intimal injury and destruction of the fibrous cap which may promote further plaque rupture, plaque protrusion, and thrombosis. Aspiration thrombectomy with a large-bore aspiration catheter may avoid such mechanical damage to the plaque. However, in cases of severe stenosis such as case 2, PTA is required before the aspiration catheter can reach the thrombus. PTA itself causes traumatic damage to the plaque, causing dissection of the intima at the microscopic level, even though it is unnoticeable on angiography.[
No previous studies have compared CEA and CAS for carotid stenosis with FFT. Treatment selection should be performed after considering the factors that increase the risk associated with each procedure, such as the stenosis rate, plaque characteristics, degree of calcification, anatomical conditions, use of antiplatelet drugs, and surgeon proficiency, should be considered, as with normal ICA stenosis. One advantage of choosing CAS is that the operation time can be shortened with minimal vascular manipulation while avoiding general anesthesia. Another benefit of endovascular treatment is the opportunity to immediately perform intracranial mechanical thrombectomy if a distal embolism occurs during the procedure. CEA can safely revascularize carotid stenotic lesions with FFT by directly accessing and occluding the distal ICA and should always be considered as an alternative treatment. Secondary treatment with CEA after endovascular therapy including floating thrombus retrieval and PTA is also a considerable option for high-risk lesions.
CONCLUSION
We reported successful two cases of ICA stenosis with FFT in which thrombectomy with a stent retriever was performed before urgent CAS. Although its indications and alternative treatments should be carefully considered due to some concerns such as mechanical irritation to the carotid artery plaque, this procedure may help reduce the risk of distal embolization of thrombus and ischemic complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bhatti AF, Leon LR, Labropoulos N, Rubinas TL, Rodriguez H, Kalman PG. Free-floating thrombus of the carotid artery: Literature review and case reports. J Vasc Surg. 2007. 45: 199-205
2. Bhogal P, AlMatter M, Pérez MA, Bäzner H, Henkes H, Hellstern V. Carotid stenting as definitive treatment for free floating thrombus-review of 7 cases. Clin Neuroradiol. 2021. 31: 449-55
3. Fitzpatrick N, Motyer R, Gibney B, Duffy S, Murphy S, O’Brien P. Expanding the role of stent-retriever endovascular thrombectomy: A case series of free-floating thrombus. J Neurointerv Surg. 2018. 10: 1164-7
4. Giragani S, Balani A, Agrawal V. Stentriever thrombectomy with distal protection device for carotid free floating thrombus: A technical case report. J Neurointerv Surg. 2017. 9: e33
5. Naruko T, Ueda M, Becker AE, Tojo O, Teragaki M, Takeuchi K. Angiographic-pathologic correlations after elective percutaneous transluminal coronary angioplasty. Circulation. 1993. 88: 1558-68
6. Omae T, Senbokuya N, Yanagisawa T. Angiography of cervical carotid plaque rupture due to percutaneus transluminal balloon arterioplasty. World Neurosurg. 2018. 115: 245-6
7. Paul AR, Entezami P, Nourollahzadeh E, Dalfino J, Boulos AS. Simultaneous revascularization of the occluded internal carotid artery using the Solitaire as a workhorse wire during acute ischemic stroke intervention. Interv Neuroradiol. 2020. 26: 205-10
8. Tatsuta Y, Ogino T, Matsuda M, Okamura N, Sakurai S, Shindo K. A case of internal carotid artery occlusion caused by en bloc distal embolization of carotid free-floating thrombus treated by mechanical thrombectomy. J Neuroendovasc Ther. 2022. 16: 93-9
9. Tomoyose R, Tsumoto T, Hara K, Miyazaki Y, Tokunaga S, Yasaka M. Mechanical thrombectomy and carotid artery stenting for stenosis of the internal carotid artery with free-floating thrombosis: Illustrative case. J Neurosurg Case Lessons. 2021. 2: Case21338
10. Tsumoto T, Terada T, Tsuura M, Matsumoto H, Masuo O, Yamaga H. Carotid artery stenting for stenosis with intraluminal thrombus. Neuroradiology. 2006. 48: 54-9
11. Yamamoto N, Yamamoto Y, Korai M, Shimada K, Kanematsu Y, Izumi Y. Simultaneous approach to tandem occlusion in acute ischemic stroke patients: Percutaneous transluminal angioplasty (PTA) using push wire of stent retriever. J Neuroendovasc Ther. 2019. 13: 257-61
12. Yamaoka A, Miyata K, Iihoshi S, Mikuni N. Endovascular treatment of asymptomatic free-floating thrombus in the carotid artery bifurcation: A direct aspiration first-pass technique under double balloon protection. BMJ Case Rep. 2019. 12: e230295