- Department of Neurological Surgery, Rutgers New Jersey Medical School, Newark, United States
- Epilepsy Institute of New Jersey, Jersey City, New Jersey, United States.
Correspondence Address:
Luke D. Tomycz, Epilepsy Institute of New Jersey, Jersey City, New Jersey, United States.
DOI:10.25259/SNI_711_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Markosian C1, Tomycz LD2. Steps toward narrowing the surgical epilepsy treatment gap through private practice. Surg Neurol Int 19-Jan-2024;15:18
How to cite this URL: Markosian C1, Tomycz LD2. Steps toward narrowing the surgical epilepsy treatment gap through private practice. Surg Neurol Int 19-Jan-2024;15:18. Available from: https://surgicalneurologyint.com/surgicalint-articles/12713/
Dear Editor,
Unlike spinal degenerative disease, which is painful and may prompt patients to self-refer to a neurosurgeon, and unlike stroke, which causes dramatic and acute-onset disability, drug-resistant epilepsy (DRE) does not cause somatic pain, yet its morbidity in multiple aspects of life (physical, psychosocial, personal, and professional) can be profound and insidious. Repeated seizures can lead to gradual and incremental worsening of memory, cognition, mood, executive processing, behavior, and psychosocial function. And while epilepsy mortality rates are increasing in the United States,[
At this point, a plethora of academic papers laments the underutilization of epilepsy surgery. The salient points are as follows: (1) epilepsy surgery is effective for patients with DRE, leading to seizure freedom or substantial palliation in the vast majority,[
Given that 1.2% of the population suffers from active epilepsy[
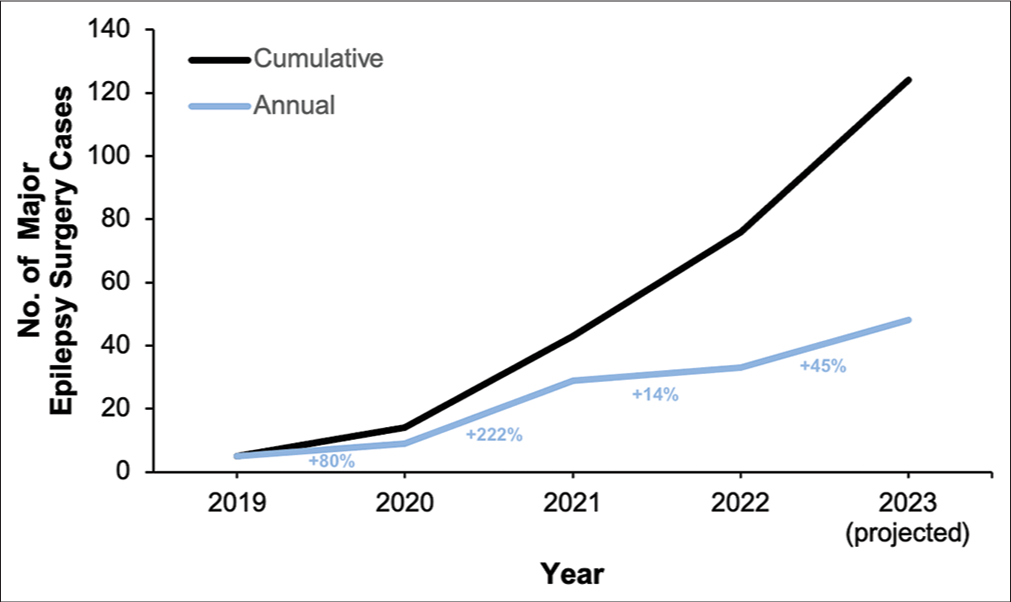
Figure 1:
Major cases in epilepsy surgery (i.e., depth electrode insertion for stereoelectroencephalography (sEEG), craniotomy for grids, craniotomy for resection or disconnection, and laser ablation) performed by L.D.T. in private practice from 2019 to 2023. Numbers correspond to major cases performed on an annual basis and cumulative basis (i.e., total number of cases performed to date). Projections for 2023 are based on cases performed in the first half of the year. These cases exclude vagus nerve stimulator implantation, vagus nerve stimulator revision, skull fiducial placement for stereotactic planning, and removal of sEEG electrodes.
The large volume of complex and advanced presurgical and surgical procedures can be attributed to high-quality resources and trained personnel in our vicinity. Nearly all of the epilepsy surgery at the Epilepsy Institute of New Jersey is conducted at a teaching hospital with resident staff and a pediatric intensive care unit as well as operating rooms equipped with neuronavigation technology, operating microscopes, sophisticated neuromonitoring including the ability to conduct phase reversal and direct cortical and subcortical stimulation, robotic technology for depth electrode implantation for stereoelectroencephalography, laser ablation technology, and intraoperative magnetic resonance imaging (MRI). The full gamut of non-invasive presurgical testing is available in New Jersey, including high-quality video electroencephalogram, 3 Tesla MRI, fluorodeoxyglucose-positron emission tomography, ictal single-photon emission computed tomography, and magnetoencephalography. Functional MRI, neuropsychological testing, and intracarotid amobarbital testing are commonly employed. While all of these studies are not typically offered at a single center, a thorough presurgical evaluation can be obtained, although in a somewhat piecemeal fashion. Furthermore, all surgical patients are reviewed in a multidisciplinary conference typically attended by epileptologists, surgeons, neuropsychologists, and radiologists, among other specialists. Access to these resources and the curation of a highly experienced network of healthcare professionals ensure that patients receive complete and the most up-to-date care.
The identification of patients with DRE who may benefit from surgery encompasses several approaches. Selection of surgical candidates should ideally be spearheaded by a fellowship-trained epileptologist in close collaboration with a neurosurgeon who possesses a deep understanding of epilepsy syndromes, surgical treatments, and requirements for surgical candidacy. First, our team continues to be actively involved in training courses as well as national and international epilepsy conferences, in addition to actively contributing to the clinical research literature. Second, multidisciplinary clinics have served as a mechanism for introducing patients to the surgeon as an integral team member early in the disease process, presenting the family with the full range of treatment options should seizures prove intractable. Third, hospital-employed surgical epilepsy nurse coordinators streamline the often-arduous presurgical testing regimen and coordinate timely conference discussions for patients who are under consideration for surgery. Fourth, quality improvement programs have been initiated at various hospitals to use electronic medical record systems to aid in the identification of patients who have failed three or more anti-seizure medications and might be surgical candidates. Fifth, in addition to delivering didactic lectures to neurologists, we have focused on speaking to intensivists, pediatricians, neonatologists, and emergency physicians, encompassing all specialties that are likely to encounter patients with epilepsy. Encouraging emergency physicians to call neurosurgery in addition to neurology for every patient who presents with seizures has helped identify surgical candidates, given that seizures account for about 1 million emergency department visits annually in the United States.[
Altogether, our implemented strategies in private practice have allowed epilepsy surgery to reach more patients with DRE in northern New Jersey. Alongside academic medical centers, private practice can play a pivotal role in tackling the underutilization of epilepsy surgery throughout the United States in an effort to help more patients attain seizure freedom. While complex spine surgery and brain tumor surgery were once exclusively within the purview of the academic neurosurgeon, these operations are now routinely being performed in private practice. We envision a similar trajectory for epilepsy surgery. Despite the challenges inherent in providing care for patients with DRE, neurosurgeons must evolve to address the formidable and devastating surgical treatment gap.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
L.D.T. is the founder and sole partner of the Epilepsy Institute of New Jersey, Inc. No other disclosures were reported.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Berg AT, Langfitt J, Shinnar S, Vickrey BG, Sperling MR, Walczak T. How long does it take for partial epilepsy to become intractable?. Neurology. 2003. 60: 186-90
2. Burrows L, Lennard S, Hudson S, McLean B, Jadav M, Henley W. Exploring epilepsy attendance at the emergency department and interventions which may reduce unnecessary attendances: A scoping review. Seizure. 2020. 76: 39-46
3. Centers for Disease Control and Prevention. Epilepsy fast facts. Available from: https://www.cdc.gov/epilepsy/about/fast-facts.htm [Last accessed on 2023 Dec 07].
4. DeGiorgio CM, Curtis A, Carapetian A, Hovsepian D, Krishnadasan A, Markovic D. Why are epilepsy mortality rates rising in the United States? A population-based multiple cause-of-death study. BMJ Open. 2020. 10: e035767
5. Engel J. What can we do for people with drug-resistant epilepsy? The 2016 Wartenberg lecture. Neurology. 2016. 87: 2483-9
6. Engel J. Why is there still doubt to cut it out?. Epilepsy Curr. 2013. 13: 198-204
7. Hader WJ, Tellez-Zenteno J, Metcalfe A, Hernandez-Ronquillo L, Wiebe S, Kwon CS. Complications of epilepsy surgery-a systematic review of focal surgical resections and invasive EEG monitoring. Epilepsia. 2013. 54: 840-7
8. Pallin DJ, Goldstein JN, Moussally JS, Pelletier AJ, Green AR, Camargo CA. Seizure visits in US emergency departments: Epidemiology and potential disparities in care. Int J Emerg Med. 2008. 1: 97-105
9. Perucca E, Perucca P, White HS, Wirrell EC. Drug resistance in epilepsy. Lancet Neurol. 2023. 22: 723-34
10. Solli E, Colwell NA, Say I, Houston R, Johal AS, Pak J. Deciphering the surgical treatment gap for drug-resistant epilepsy (DRE): A literature review. Epilepsia. 2020. 61: 1352-64
11. Téllez-Zenteno JF, Dhar R, Wiebe S. Long-term seizure outcomes following epilepsy surgery: A systematic review and meta-analysis. Brain. 2005. 128: 1188-98