- Department of Neurosurgery, Azienda Ospedaliero Universitaria Renato Dulbecco di Catanzaro, Catanzaro, Italy
- Unit of Infectious and Tropical Diseases, Azienda Ospedaliero Universitaria “Renato Dulbecco” di Catanzaro, Catanzaro, Italy
- Unit of Biomedical Engineering, Azienda Ospedaliero Universitaria “Renato Dulbecco” di Catanzaro, Catanzaro, Italy
- Department of Radiology, Azienda Ospedaliero Universitaria “Renato Dulbecco” di Catanzaro, Catanzaro, Italy
- Department of Neurosurgery, Azienda Ospedaliero Universitaria di Sassari, Sassari, Italy.
Correspondence Address:
Domenico Policicchio, Department of Neurosurgery, Azienda Ospedaliero Universitaria “Renato Dulbecco” di Catanzaro, Catanzaro, Italy.
DOI:10.25259/SNI_977_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Domenico Policicchio1, Lucio Cosco2, Giuseppe Mauro1, Alfonso Nicola Iannello1, Luigi Santaguida3, Virginia Vescio4, Giosué Dipellegrini5. Stereotactic placement of dual lumen catheter system for continuous drainage, irrigation, and intraventricular antibiotic therapy for treatment of brain abscess with ventriculitis – A case report and literature review. 23-Feb-2024;15:57
How to cite this URL: Domenico Policicchio1, Lucio Cosco2, Giuseppe Mauro1, Alfonso Nicola Iannello1, Luigi Santaguida3, Virginia Vescio4, Giosué Dipellegrini5. Stereotactic placement of dual lumen catheter system for continuous drainage, irrigation, and intraventricular antibiotic therapy for treatment of brain abscess with ventriculitis – A case report and literature review. 23-Feb-2024;15:57. Available from: https://surgicalneurologyint.com/surgicalint-articles/12763/
Abstract
Background: Cerebral abscesses complicated by ventriculitis present significant treatment challenges, often associated with high morbidity and mortality. Traditional management approaches, including systemic antibiotic therapy and external ventricular drainage (EVD), face limitations due to the blood-brain barrier and risks of catheter-related complications. This report discusses a case where the dual-lumen catheter system, an innovative neurosurgical tool integrating continuous irrigation with drainage, was employed.
Case Description: A patient presented with a cerebral abscess ruptured into the ventricle, leading to ventriculitis. Conventional treatment options were limited due to the abscess’s deep and eloquent location and the associated risk of complications from standard EVD. The dual lumen system was chosen for its ability to provide continuous irrigation and drainage, effectively addressing issues of catheter blockage and enhancing localized antibiotic delivery. The system was used to create a single stereotactic tract for simultaneous treatment of the abscess and ventriculitis. This approach allowed for a more controlled and effective treatment process, resulting in rapid resolution of the conditions without chronic hydrocephalus development or further complications.
Conclusion: The use of the dual lumen system represented a significant advancement in this case, addressing the limitations of conventional treatments. Its ability to maintain intracranial pressure within optimal limits while providing localized, continuous treatment was pivotal. This case highlights the potential of the dual lumen catheter in managing complex neurosurgical infections and underscores the need for further research to establish its efficacy in broader clinical applications.
Keywords: Brain abscess, Frameless stereotaxy, Intrathecal therapy, IrraFlow, Ventriculitis
INTRODUCTION
This scientific report delves into the exploration of the dual lumen as a potential breakthrough in the targeted treatment of brain abscess with ventriculitis, a complex and life-threatening pathology that precipitates an infectious condition within the ventricular system paired with hydrocephalus due to altered cerebrospinal fluid (CSF) circulation and intracranial hypertension.[
Addressing both these facets is pivotal in management. While systemic antibiotic therapy often results in suboptimal efficacy due to limited penetration, and traditional external ventricular drainage (EVD) systems are fraught with high failure rates due to clogging from purulent material, the dual lumen system presents a novel approach.
In an effort to improve outcomes, intrathecal (IT) antibiotic therapy has been proposed as a supplemental treatment.[
Recently, the use of the Dual lumen catheter for continuous ventricular drainage and irrigation has been advanced for the management of ventricular hemorrhages[
In this case report, we present an unusual scenario involving a thalamic abscess that had ruptured into the ventricular system, leading to ventriculitis and hydrocephalus. We performed a frameless stereotactic drainage of the abscess and, through the same stereotactic approach, placed the dual lumen catheter to irrigate both the ventricle and the abscess cavity continuously. We discuss this case in detail, highlighting the potential advantages and disadvantages of this novel technique, also in light of a literature review.
CASE DESCRIPTION
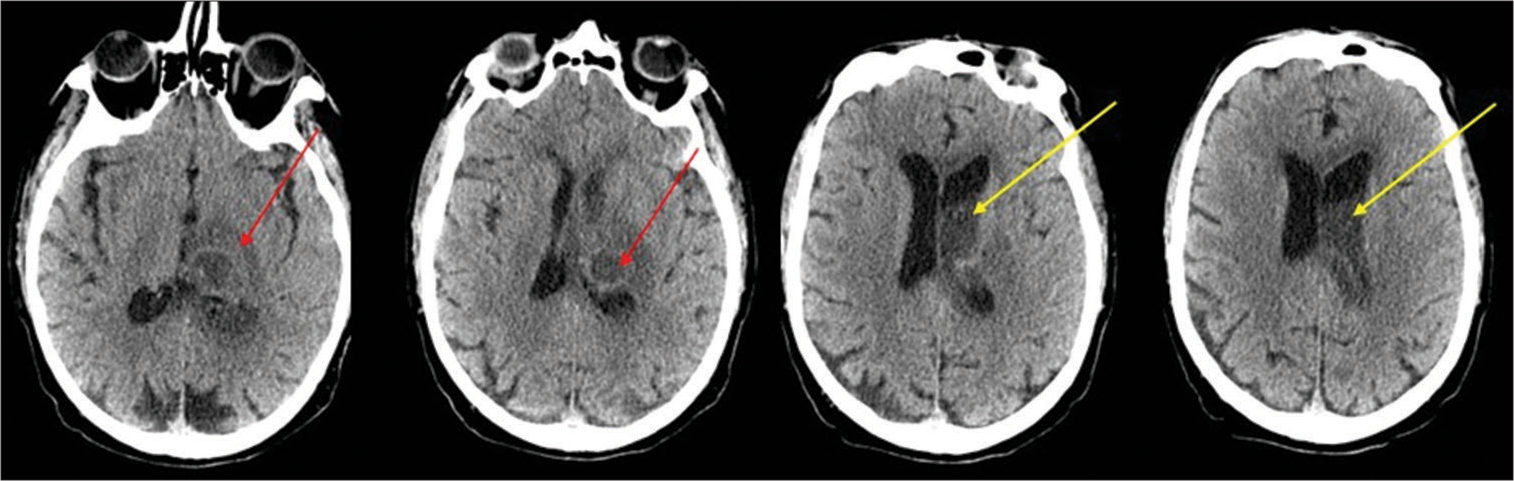
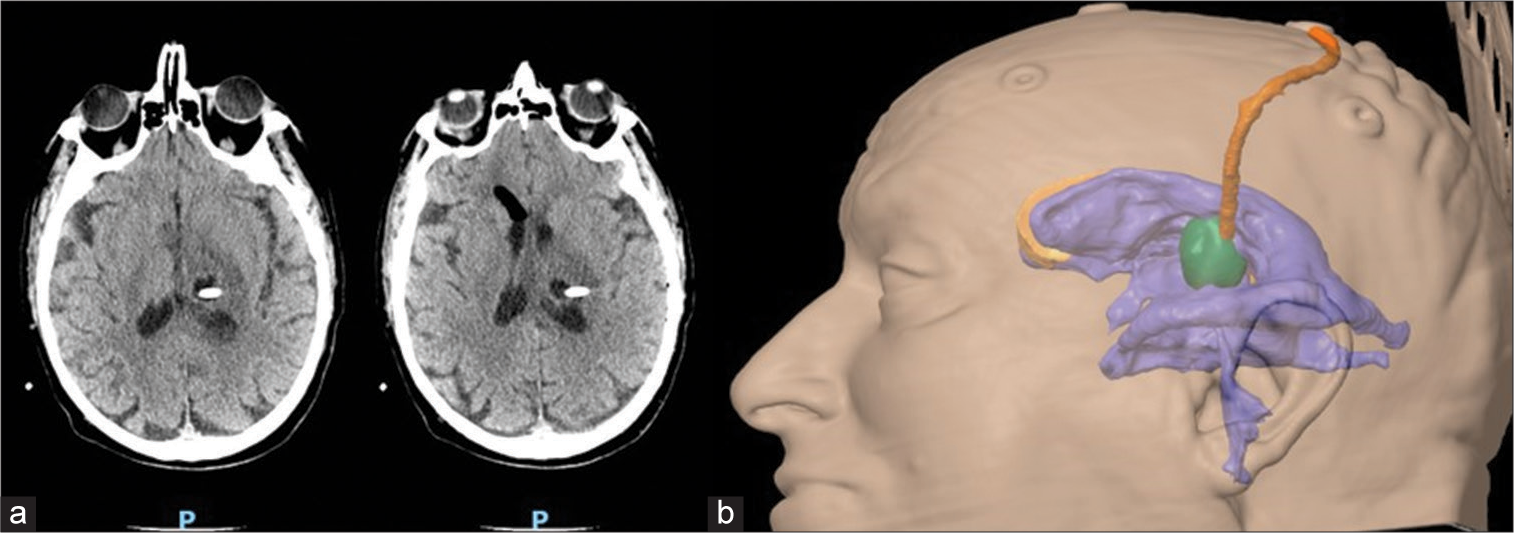
A 73-year-old male with histories of hypertension and diabetes mellitus and no other significant medical history presented in good health to our emergency department with a 3-day history of confusion and fever (37.8°C). Upon examination, the patient was alert but exhibited signs of mild ideomotor slowing, disorientation in time and space, recent memory impairment, and mild right-sided hemiparesis, accompanied by a slight headache (Glasgow coma score [GCS] 14). Though the fever had resolved by the time of examination, no signs of meningeal irritation were observed. Initial cranial computed tomography (CT) imaging identified a hypodense nodular lesion in the left thalamus suggestive of a neoplastic process or an abscess [
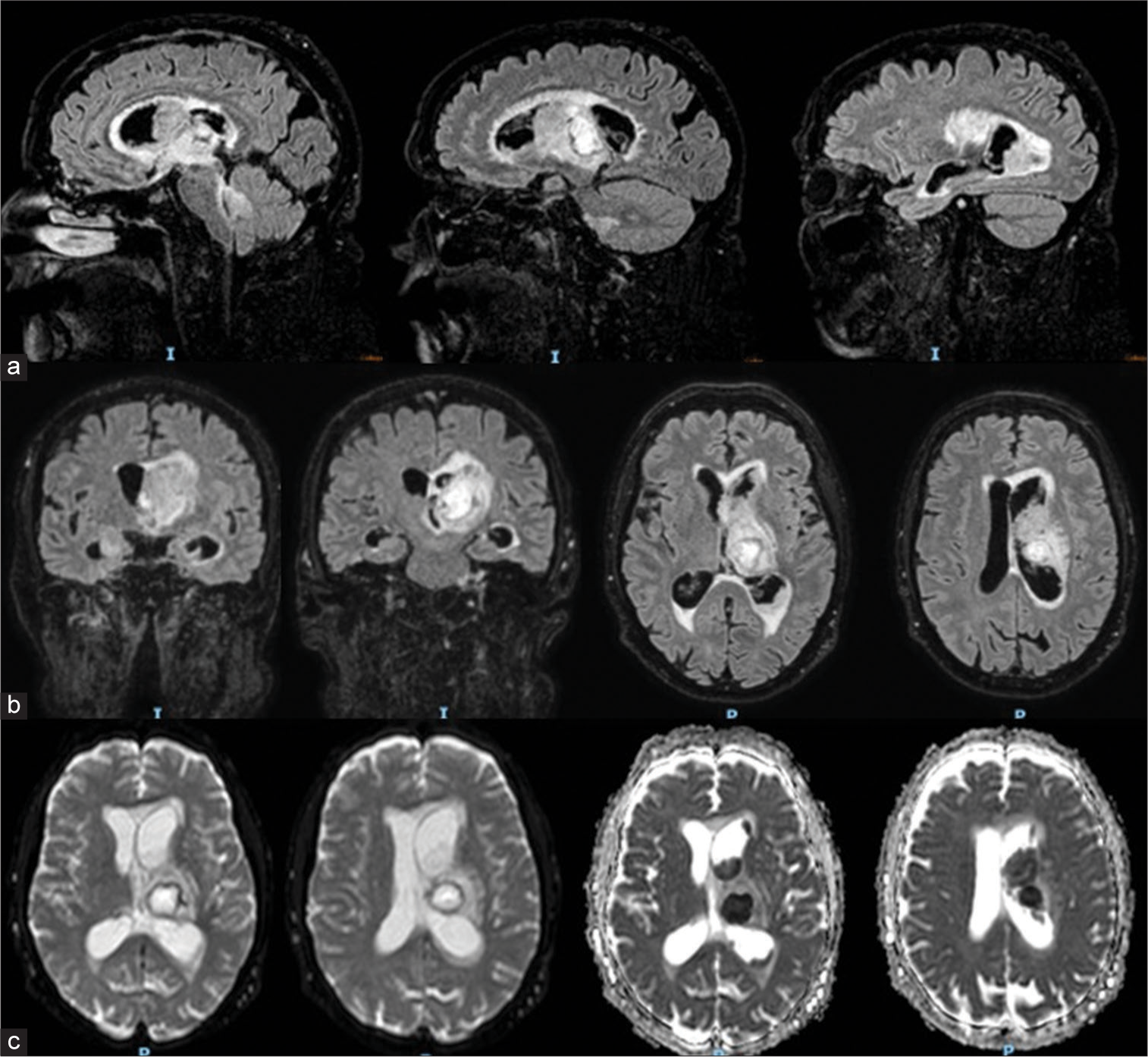
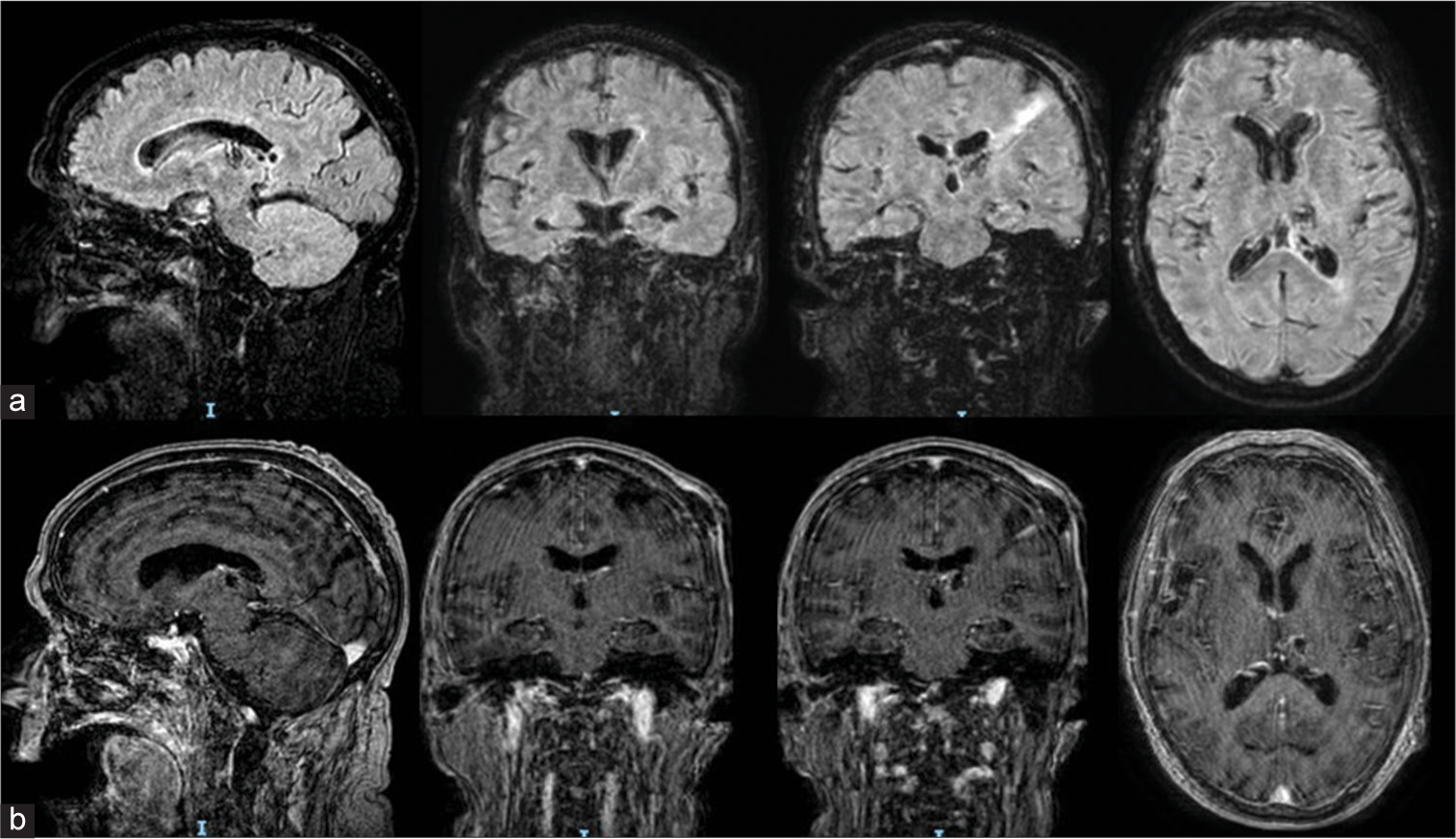
The MRI confirmed a left thalamic abscess with a direct rupture into the ventricular system, causing ventriculitis characterized by diffuse ependymal enhancement and dense intraventricular material [
Figure 2:
Brain MRI: A left thalamic abscess measuring approximately 2cm in maximum diameter, with characteristics consistent with an infectious process – hyperintensity on DWI, hypointensity on ADC, central necrosis, surrounding edema affecting the thalamus and midbrain tectum. Dense material within the left lateral ventricle (body, atrium, and occipital horn) and partially in the right lateral ventricle, the aqueduct of Sylvius, and the fourth ventricle. The upper (a) and middle (b) rows display MRI FLAIR sequences in sagittal, coronal, and axial slices. The lower row (c) presents images in DWI and ADC map axial slices. FLAIR: Fluid Attenuation Inversion Recovery, DWI: Diffusion Weighted Images, ADC: Apparent Diffusion Coefficent.
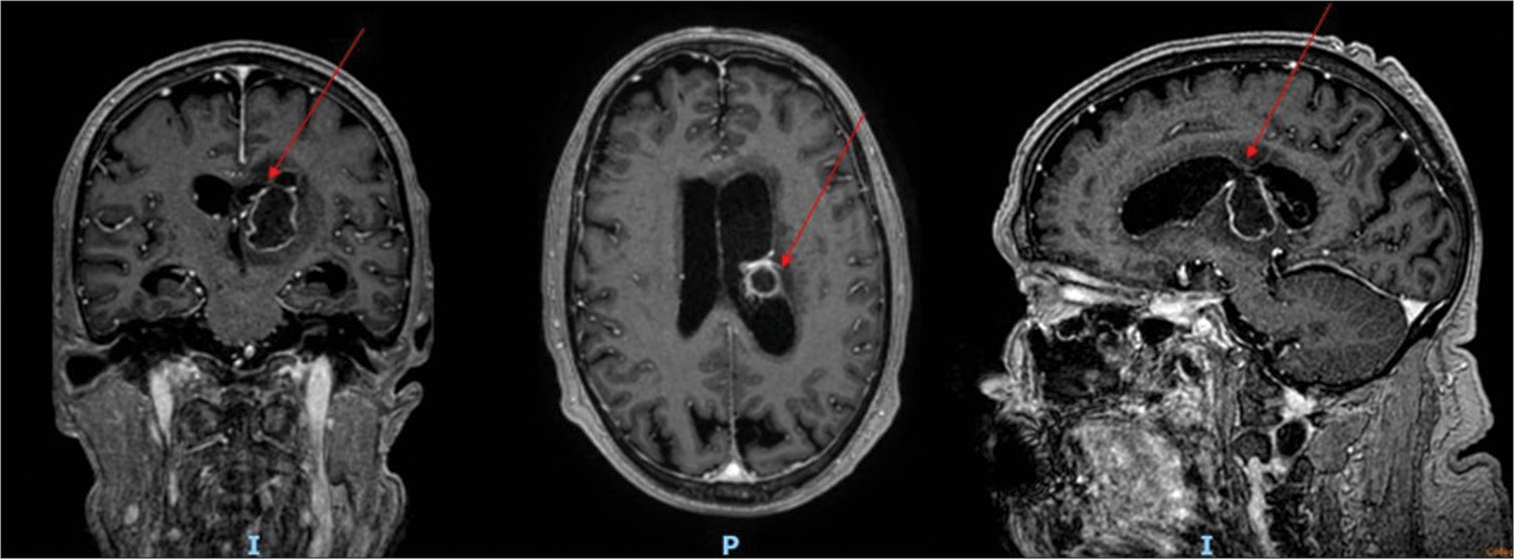
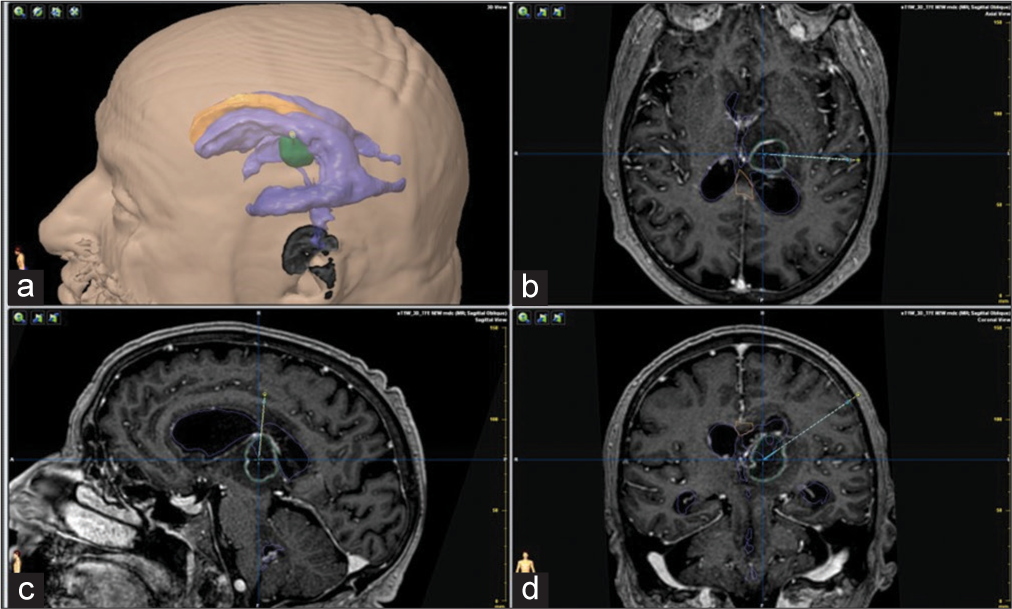
A decision for surgical intervention was made given the triad of abscess, ventriculitis, and hydrocephalus. Preoperative planning involved a 3D virtual model to strategize the stereotactic approach to the abscess and possible EVD placement[
Figure 4:
Stereotactic planning using a pc-generated 3D virtual model representing ventricles and abscess and showing the planned trajectory. Panel a: 3D virtual model; Panels b, c, d: pos-contrast T1 weighted MRI, axial, coronal and sagittal slices with superimposed reconstruction of abscess and ventricles and planned stereotactic trajectory.
Using the BrainLab VarioGuide system, we performed frameless stereotactic surgery, aspirating the abscess and obtaining samples for histological examination. The confirmation of CSF flow through the stereotactic needle indicated a patent communication with the ventricular system. A dual-lumen catheter (IRRAFlow®, IRRAS, Stockholm, Sweden) was subsequently inserted via the same stereotactic route. Postoperative CT confirmed the reduction of the abscess and optimal placement of the catheter [
Postoperatively, the irrigation and drainage exchange system was initiated; treatment began with a single intraventricular gentamicin bolus of 9 mg, followed by an infusion of NaCl 0.9% at 180 mL/h with gentamicin three mg/L diluted in the saline solution. The intracranial pressure (ICP) alarm was set at 15 mmHg to prevent over-irrigation. The patient was rotated every six hours to facilitate antibiotic penetration throughout the ventricular system and to aid in the drainage of pus. Systemic antibiotic and corticosteroid therapy continued.
The patient’s clinical conditions gradually improved, and laboratory tests were monitored, showing a progressive normalization of inflammation markers. Follow-up cranial CT scans revealed progressive clearance of the ventricular system. After eight days, the catheter ceased functioning. A subsequent CT indicated a slight dislocation; an MRI of the brain confirmed the well-drained abscess and reduction in ventricular size with a marked decrease in ventriculitis, diminished intraventricular purulent material, and disappearance of transependymal resorption [
Figure 6:
Post-operative MRI performed 9 days following surgery, depicting a reduction in the size of the brain abscess and ventricular dimensions, a decrease in edema, and an almost complete regression of ventriculitis. Upper row (a): Fluid Attenuation Inversion Recovery (FLAIR) sequences in sagittal, coronal and axial slices; lower row (b): post-contrast T1 weighted MRI in sagittal, coronal and axial slices. FLAIR: Fluid Attenuation Inversion Recovery.
The patient’s recovery was remarkable; 4 weeks after surgery, the patient appeared alert and, responsive, cooperative, with mild memory deficits and slight confusion, complete regression of hemiparesis (GCS 14), and in good general condition, and was then transferred to a rehabilitation facility to begin the recovery process.
DISCUSSION
This case report illustrates a complex scenario involving the management of a cerebral abscess ruptured into the ventricle with subsequent ventriculitis, a condition that poses significant treatment challenges and is associated with high morbidity and mortality rates from 26% to 72.7% reported in various case series depending on the route of infection and the organism responsible.[
The patient’s clinical journey underscores the nuanced decision-making process in neurosurgical interventions and the critical role of innovative techniques such as the dual lumen catheter system.[
The standard management of cerebral abscesses through systemic antibiotic therapy is hindered by the blood-brain barrier, which limits the efficacy of therapeutic agents within the CSF and abscess cavities. Conventional EVD, although a critical component in treating ventriculitis, is prone to complications. The frequent occurrence of catheter occlusion by purulent material necessitates repeated repositioning, increasing the risk of hemorrhagic events. The inflammation of the ventricular walls, a consequence of the ongoing infection, exacerbates this risk, as the fragile tissue is more susceptible to bleeding during such interventions.
To overcome these challenges, the dual-lumen catheter system has emerged as an innovative solution, transforming the approach to managing such neurosurgical conditions.[
In our case, we were faced with the dual surgical challenges of draining the abscess and treating hydrocephalus secondary to ventriculitis. Brain abscesses could be managed via stereotactic aspiration through a burr hole or open craniotomy. Considering the deep and eloquent location of the abscess, we favored a stereotactic aspiration over craniotomy, in line with contemporary literature advocating for a minimally invasive technique for supratentorial brain abscesses.[
Regarding ventricular drainage, drawing on prior literature that suggests the high efficacy and safety of this dual-lumen catheter system in ventriculitis cases, we decided to implement this novel system.[
The Dual-lumen system differs from traditional EVD due to its capability to drain and instill fluid simultaneously through a dual-lumen catheter.[
It operates on a cycle, monitoring ICP for 9 s, infusing 1 mL in 1 s (in our case, a solution of 0.9% NaCl with Gentamicin 9 mg/L at an infusion rate of 180 mL/h), and then draining for 10 s. The system is programmed with maximum and minimum ICPs to regulate the infusion and ensure balanced fluid exchange within 24 hours. The patient’s positioning is altered to facilitate ventricular lavage and the drainage of the highly viscous pus. Our placement of the drain within the abscess cavity enabled simultaneous washing of the ventricular system and abscess cavity.
The dual lumen catheter system boasts an advantage over standard catheters by flushing out inflammatory mediators and debris from the ventricular system, which aids in reducing inflammation; however, it particularly stands out for its ability to deliver antibiotics directly into the ventricular system, allowing for high local concentrations of antibiotics that could be pivotal in eradicating the infection.
IT antibiotic therapy is still an emerging, non-standardized technique, but recent literature points to its potential advantages in managing ventricular infections. Traditional delivery through EVDs faces several challenges, including the risks associated with opening a sterile system, bolus drug administration, and the necessity to clamp the EVD post-medication, which can complicate treatment. In contrast, the continuous and controlled medication delivery offered by the dual-lumen active fluid exchange system has been shown to diminish these issues, signifying a potential leap forward in IT pharmacotherapy.
The case we reported showed excellent results with a short treatment duration (7 days) and complete resolution of ventriculitis and abscess without complications or chronic hydrocephalus. Despite this positive outcome, caution is necessary when considering the results; varying successes with this device in ventriculitis have been documented in the literature.[
Rezai et al. reported on two patients who were treated with the IRRAflow system for ventriculitis. The treatment lasted for 11 and 19 days, respectively. Both patients developed post-infectious hydrocephalus, which was managed with an endoscopic third ventriculostomy in one case and a ventriculoperitoneal (VP) shunt in the other.[
In our patient, we achieved rapid resolution of ventriculitis without chronic hydrocephalus development. We speculate that ventricular lavage (combined with systemic antibiotic and cortisone therapy) may prevent post-infective hydrocephalus, which is common after ventriculitis and often necessitates VP shunt placement. Although we cannot assert with certainty that the dual lumen catheter system prevented hydrocephalus, as other cases have required shunt implantation despite successful resolution with dual lumen catheter, we hypothesize that it may expedite healing and reduce the likelihood of developing chronic hydrocephalus. This hypothesis, however, requires confirmation through larger case series and controlled clinical trials. The use of dual lumen catheters for ventriculitis treatment is an evolving field, and ongoing research and clinical experience are necessary to better define its role, optimal protocols, and long-term outcomes.
Potential drawbacks
While this device shows promise, there are challenges to consider. These include the potential for complications related to the irrigation procedure, the selection of appropriate antibiotics, and the need for a dedicated team with experience in the technique.
Another potential drawback of this device is its significantly higher cost compared to standard EVDs, placing a heavier financial burden on healthcare providers. However, should clinical trials and evidence-based data demonstrate a clear superiority in managing complex patient conditions, the increased expense could be justified as a cost-effective investment in improved patient outcomes.
CONCLUSION
The introduction of the dual-lumen catheter system was pivotal in our patient’s recovery. Its mechanism of continuous irrigation and drainage represents a significant advancement in treating such infections. By ensuring the unobstructed flow of CSF and the delivery of antibiotics directly to the infection site, the dual-lumen catheter addresses the fundamental limitations of conventional EVD. Moreover, the system’s ability to maintain ICP within optimal limits while administering localized treatment exemplifies the potential for tailored therapeutic interventions in neurosurgery.
However, larger clinical trials and further research are necessary to fully understand and establish the long-term benefits and potential drawbacks of this innovative treatment modality.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors thank Engineer Raffaele Tiriolo and ForMedical Srl for their invaluable technical and scientific support.
References
1. Carpenter AB, Lara-Reyna J, Hardigan T, Ladner T, Kellner C, Yaeger K. Use of emerging technologies to enhance the treatment paradigm for spontaneous intraventricular hemorrhage. Neurosurg Rev. 2022. 45: 317-28
2. DiPellegrini G, Boccaletti R, Mingozzi A, Fara A, Policicchio D. Single thalamic localization of brain toxoplasmosis mimicking brain tumors: Radiological and clinical findings. Surg Neurol Int. 2023. 14: 82
3. Feinberg N, Campbell B, Bazylewicz M, Brown WD, Singh D, Whitman T. Brain abscess with pyogenic ventriculitis. IDCases. 2022. 28: e01503
4. Field NC, Custozzo AJ, Harland TA, Sweeney JF, Adamo MA, Dalfino JC. Drainage, irrigation, and fibrinolytic therapy (DRIFT) for adult intraventricular hemorrhage associated with primary hypertensive hemorrhages using IRRAflow self-irrigating catheter: A report of three cases and prior historical controls. World Neurosurg. 2023. 177: 137-42
5. Garavaglia J, Hardigan T, Turner R, Monachello G, Khan MB, Hodge JO. Continuous intrathecal medication delivery with the IRRAflow catheter: Pearls and early experience. Oper Neurosurg (Hagerstown). 2023. p.
6. Haldrup M, Mohamad N, Rasmussen M, Thorup L, Dyrskog S, Simonsen CZ. Study protocol for ACTIVE study: Safety and feasibility evaluation of external ventricular drainage with ACTIVE fluid exchange in intraventricular hemorrhage-a phase 2, multi-center, randomized controlled trial. Trials. 2022. 23: 1062
7. Hess RM, Khan A, Edwards M, Siddiqui AH, Levy EI. Continuous intraventricular vancomycin for treatment of ventriculitis using IRRAflow® A case report. Surg Neurol Int. 2021. 12: 583
8. Hess RM, Lazar A, Smolar D, OConnor TE, Khan A, Siddiqui AH. Continuous antibiotic administration using IRRAflow® catheter for treatment of intracranial abscess. Cureus. 2021. 13: e19061
9. Hess RM, OConnor TE, Khan A, Siddiqui AH, Davies J. Minimally invasive approach to subdural hematoma treatment using IRRAflow catheter and middle meningeal artery embolization. Cureus. 2021. 13: e13979
10. Lewin JJ, Cook AM, Gonzales C, Merola D, Neyens R, Peppard WJ. Current practices of intraventricular antibiotic therapy in the treatment of meningitis and ventriculitis: Results from a multicenter retrospective cohort study. Neurocrit Care. 2019. 30: 609-16
11. Mazzucchi E, La Rocca G, Hiepe P, Pignotti F, Galieri G, Policicchio D. Intraoperative integration of multimodal imaging to improve neuronavigation: A technical note. World Neurosurg. 2022. 164: 330-40
12. Policicchio D, Boccaletti R, Casu G, Dipellegrini G, Doda A, Muggianu G. Utility and feasibility of a low-cost system to simulate clipping strategy for cerebral aneurysms using 3D CTA with virtual craniotomy. World Neurosurg. 2022. 168: 155-64
13. Policicchio D, Boccaletti R, Mingozzi A, Veiceschi P, Dipellegrini G. Minimally invasive ultrasound-assisted evacuation of Spontaneous Supratentorial Intracerebral hemorrhages: Retrospective observational single-cohort study. J Stroke Cerebrovasc Dis. 2023. 32: 107445
14. Policicchio D, Boccaletti R, Dipellegrini G, Doda A, Stangoni A, Veneziani SF. Pedicled multifidus muscle flap to treat inaccessible dural tear in spine surgery: Technical note and preliminary experience. World Neurosurg. 2021. 145: 267-77
15. Policicchio D, Dipellegrini G, Muggianu G, Pintus A, Sgaramella E, Veneziani Santonio F. Flexible fiber CO(2) laser in microsurgical treatment of intraventricular tumors: Usefulness and limitations. World Neurosurg. 2019. 122: e427-35
16. Rajjoub K, Hess RM, O’Connor TE, Khan A, Siddiqui AH, Levy EI. Drainage, irrigation, and fibrinolytic therapy (DRIFT) for adult intraventricular hemorrhage using IRRAflow® Self-irrigating catheter. Cureus. 2021. 13: e15167
17. Ratnaike TE, Das S, Gregson BA, Mendelow AD. A review of brain abscess surgical treatment--78 years: Aspiration versus excision. World Neurosurg. 2011. 76: 431-6
18. Rezai Jahromi B, Tanskanen P, Koski-Pàlken A, Schwartz C, Koroknay-Pal P, Romo I. Active cerebrospinal fluid exchange system for treatment of pyogenic ventriculitis. Neurosurg Open. 2021. 2: 1-6
19. Shofty B, Neuberger A, Naffaa ME, Binawi T, Babitch T, Rappaport ZH. Intrathecal or intraventricular therapy for post-neurosurgical Gram-negative meningitis: Matched cohort study. Clin Microbiol Infect. 2016. 22: 66-70
20. Spanu T, Rigante D, Tamburrini G, Fiori B, D’Inzeo T, Posteraro B. Ventriculitis due to Staphylococcus lugdunensis Two case reports. J Med Case Rep. 2008. 2: 267
21. Stati G, Migliorino E, Moneti M, Castioni CA, Scibilia A, Palandri G. Treatment of cerebral ventriculitis with a new self-irrigating catheter system: Narrative review and case series. J Anesth Analg Crit Care. 2023. 3: 46