- Department of Neurosurgery, Fukuoka Neurosurgical Hospital, Fukuoka, Japan.
- Department of Cerebrovascular Medicine, Fukuoka Neurosurgical Hospital, Fukuoka, Japan.
Correspondence Address:
Shinichiro Yoshida, Department of Neurosurgery, Fukuoka Neurosurgical Hospital, Fukuoka, Japan.
DOI:10.25259/SNI_567_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shinichiro Yoshida1, Kaisei Kamatani1, Kousuke Takigawa1, Noriaki Tashiro2, Yoshiya Hashiguchi2, Masahiro Yasaka2, Hiroshi Aikawa1, Yoshinori Go1, Kiyoshi Kazekawa1. Strategy of cerebral endovascular treatment for cervical internal carotid artery stenosis with a persistent primitive hypoglossal artery. 01-Sep-2023;14:308
How to cite this URL: Shinichiro Yoshida1, Kaisei Kamatani1, Kousuke Takigawa1, Noriaki Tashiro2, Yoshiya Hashiguchi2, Masahiro Yasaka2, Hiroshi Aikawa1, Yoshinori Go1, Kiyoshi Kazekawa1. Strategy of cerebral endovascular treatment for cervical internal carotid artery stenosis with a persistent primitive hypoglossal artery. 01-Sep-2023;14:308. Available from: https://surgicalneurologyint.com/surgicalint-articles/12523/
Abstract
Background: Persistent primitive hypoglossal artery (PPHA) is a rare residual arterial anastomosis. We placed a CASPER stent using Spider FX as an embolic protection device (EPD) in a patient with internal carotid artery (ICA) stenosis and PPHA. There are no reports of carotid artery stenting (CAS) using a CASPER stent for ICA stenosis with PPHA. We report the EPD strategy used in this case and the usefulness and precautions of CASPER stent insertion for cervical ICA stenosis in association with PPHA.
Methods: A 9Fr sheath was placed in the right femoral artery and a 9Fr Branchor balloon guide catheter was guided to the common carotid artery. A Spider FX was placed proximal to the bifurcation of the ICA and the PPHA. A 10 mm × 20 mm CASPER stent was deployed at the site of the stricture with no postoperative ischemic complications.
Results: There was no intra-stent occlusion, stenosis, or plaque protrusion immediately after surgery, and no postoperative ischemic complications were observed.
Conclusion: CASPER stent deployment with the Spider FX in the ICA and PPHA bifurcation can be considered to be an effective treatment method for ICA stenosis associated with PPHA. However, care should be taken in selecting the appropriate EPDs and stents depending on the location of the stenosis and bifurcation of the PPHA.
Keywords: carotid artery stenting, carotid stenting, CASPER, persistent primitive hypoglossal artery
INTRODUCTION
Persistent primitive hypoglossal artery (PPHA) is a rare residual artery anastomosis.[
MATERIALS AND METHODS
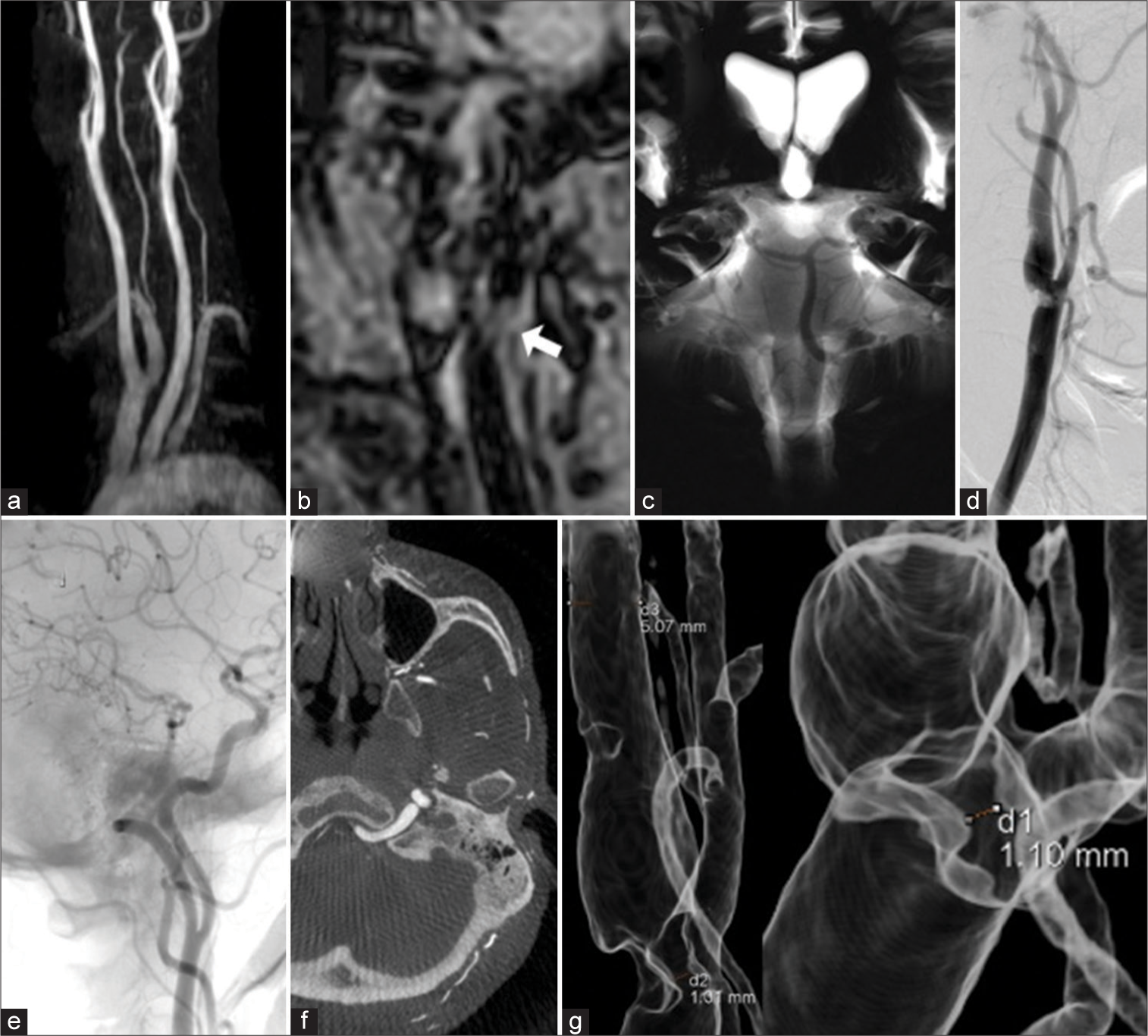
A 76-year-old male patient with repeated episodes of fainting, apraxia, and right-sided weakness was diagnosed by magnetic resonance imaging and digital subtraction angiography with ICA stenosis and PPHA [
Figure 1:
A 76-year-old male patient was brought to the emergency department due to repeated episodes of fainting, apraxia, and right-sided weakness. (a) Magnetic resonance angiography showed stenosis of the left internal carotid artery (ICA). (b) T1-weighted image black-blood magnetic resonance imaging (MRI) showed that the stenotic part had normal signal intensity (white arrow). (c) Basi-parallel anatomical scanning MRI revealed right vertebral artery hypoplasia. (d) Pre-procedure digital subtraction angiography (DSA) demonstrated two areas of stenosis, one immediately after the bifurcation and one distal to it. (e) Pre-procedure DSA of left common carotid angiography demonstrated the primitive hypoglossal artery distal to the stenosis of the ICA. (f) Pre-procedure three-dimensional rotational angiography (3D-RA) demonstrated the primitive hypoglossal artery penetrating the hypoglossal canal. (g) Pre-procedure 3D-RA showed that the stenotic part was about 1 mm in diameter.
RESULTS
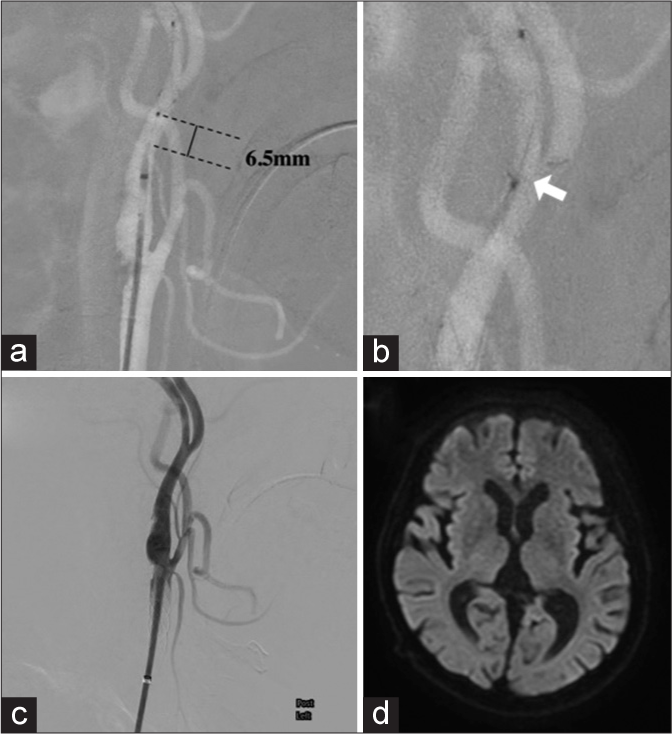
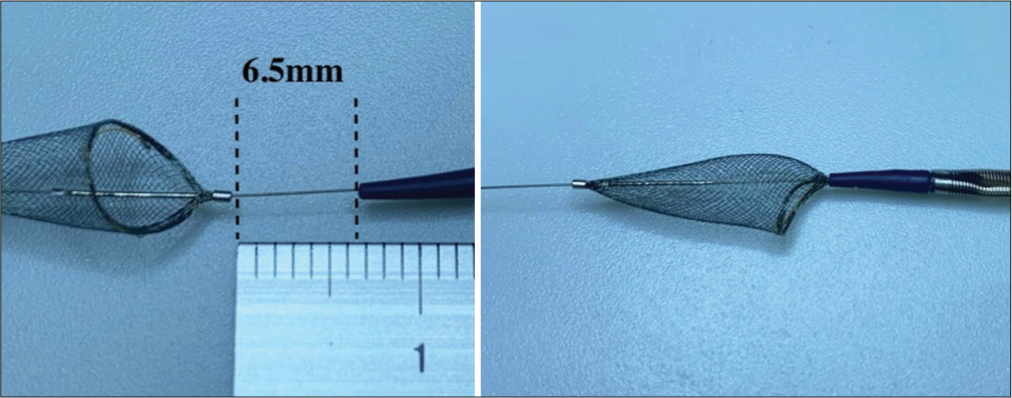
The results of preoperative VerifyNow System testing were 415 ARU and 159 PRU. The distance between the catheter tip of the Spider FX and the stent delivery system before stent placement was 6.5 mm [
Figure 2:
(a-c) Intraprocedure digital subtraction angiography. (a) The distance between the catheter tip of the Spider FX and the stent delivery system before stent placement was 6.5 mm. (b) The catheter tip of the CASPER stent delivery system got stuck in the Spider FX (white arrow), making its retrieval difficult. (c) No intrastent occlusion, stenosis, or plaque protrusion was observed. (d) Postprocedure magnetic resonance imaging–diffusion-weighted imaging showed no ischemic complications.
DISCUSSION
In addition to, persistent primitive trigeminal artery and persistent proatlantal artery, PPHA exists as a residual vascular anastomosis that connects the carotid and vertebral arteries.[
Our patient had both ICA stenosis and PPHA and since the number of such case reports is small, there is no consensus regarding the appropriate treatment method. Treatment methods for ICA stenosis include carotid endarterectomy (CEA) and CAS.
In the SAPPHIRE study, CEA was considered to carry a high risk in patients with heart disease, severe respiratory disease, contralateral carotid artery occlusion, contralateral laryngeal nerve palsy, previous direct neck surgery or neck radiotherapy, and CEA restenosis with CEA, and CAS is considered to be a treatment option in such cases.[
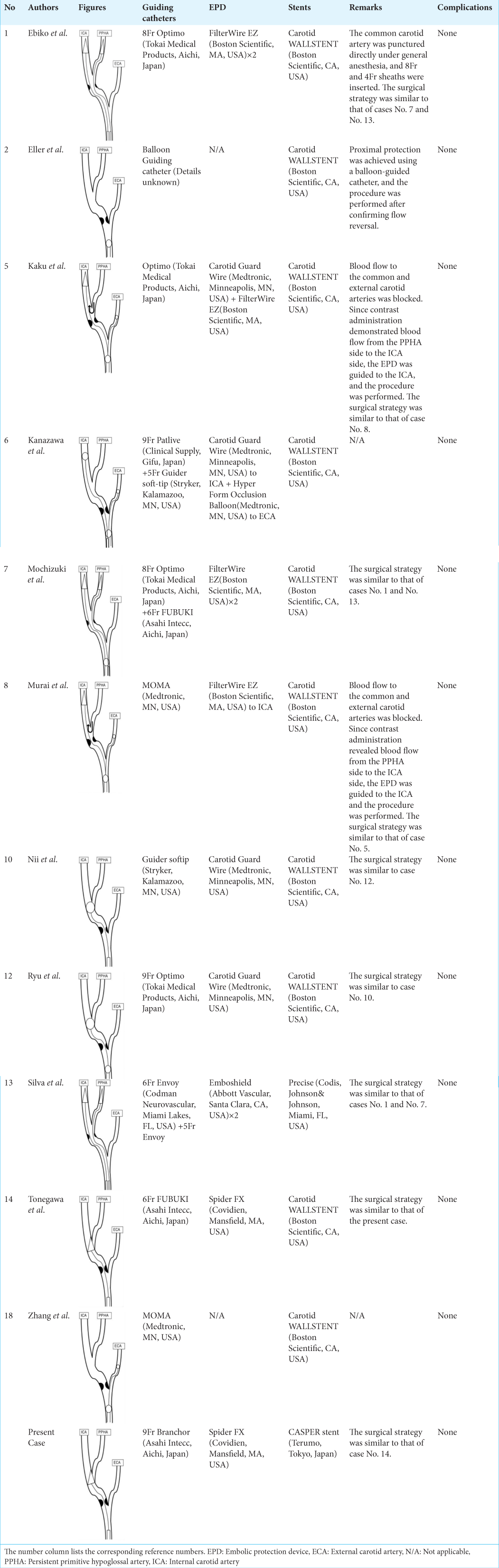
There are 12 reported cases of CAS for ICA stenosis accompanied by PPHA, including ours.[
Tonegawa et al.[
Conventional carotid artery stents used in CAS include the open-cell PROTÉGÉ (Covidien, Mansfield, MA, USA), Precise (Cordis, Johnson and Johnson, Miami, FL, USA), and the closed-cell Carotid Wallstent (Boston Scientific, Santa Clara, CA, USA). The CASPER stent has a small mesh structure and a double-layer micromesh structure and has been used in recent years since it has been shown to have fewer embolic complications than conventional stents.[
In the present case, a CASPER stent was used to prevent plaque protrusion and plaque scattering during the procedure, and a Spider FX was used as the DF-type EPD. Consequently, no postoperative ischemic complications were observed following the procedure [
CONCLUSION
CASPER stent deployment with Spider FX in the ICA and PPHA bifurcation is considered to be an effective method for treating ICA stenosis associated with PPHA. However, care should be taken to ensure the appropriate selection of EPDs and stents, depending on the location of the stenosis and bifurcation of the PPHA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that they have used Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript or image creations.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ebiko Y, Yoshino Y, Ikota M, Watabe T, Uchiyama T, Soma N, Kusaka G. Carotid artery stenting with persistent primitive hypoglossal artery performed by carotid direct puncture and double distal filter protection: A case report. Jpn J Stroke. 2021. 43: 540-5
2. Eller JL, Jahshan S, Dumont TM, Kan P, Siddiqui AH. Tandem symptomatic internal carotid artery and persistent hypoglossal artery stenosis treated by endovascular stenting and flow reversal. BMJ Case Rep. 2013. 2013: bcr2012010578
3. Fantini GA, Reilly LM, Stoney RJ. Persistent hypoglossal artery: Diagnostic and therapeutic considerations concerning carotid thromboendarterectomy. J Vasc Surg. 1994. 20: 995-9
4. Grego F, Stramanà R, Lepidi S, Antonello M, Bonvini S, Zaramella M. Primitive proatlantal intersegmental artery and carotid endoarterectomy. J Vasc Surg. 2004. 39: 691
5. Kaku S, Nishimura K, Fuga M, Watanabe M, Iwamoto I, Murayama Y. Carotid artery stenting for symptomatic stenosis of the cervical carotid artery associated with persistent primitive hypoglossal artery: A case report. J Neuroendovasc Ther. 2017. 11: 474-8
6. Kanazawa R, Ishihara S, Okawara M, Ishihara H, Kohyama S, Yamane F. A successful treatment with carotid arterial stenting for symptomatic internal carotid artery severe stenosis with ipsilateral persistent primitive hypoglossal artery: Case report and review of the literature. Minim Invasive Neurosurg. 2008. 51: 298-302
7. Mochizuki Y, Higa T, Iwata Y, Kawamata T. A case of carotid artery stenosis associated with persistent primitive hypoglossal artery treated by carotid artery stenting with double distal protection using the jail technique. J Neuroendovasc Ther. 2017. 11: 588-91
8. Murai S, Kusaka N, Umakoshi M, Itami H, Otsuka S, Nishiura T. Stenting for internal carotid artery stenosis associated with persistent primitive hypoglossal artery using proximal flow blockade and distal protection system: A technical case report and literature review. J Stroke Cerebrovasc Dis. 2016. 25: e98-102
9. Nagata T, Mitsuhashi Y, Kawakami T, Tsuruta S, Inoue T, Ohata K. Selection of surgical procedures to treat carotid artery stenosis. Surg Cerebral Stroke. 2019. 47: 266-71
10. Nii K, Aikawa H, Tsutsumi M, Onizuka M, Nakau H, Inoue R. Carotid artery stenting in a patient with internal carotid artery stenosis and ipsilateral persistent primitive hypoglossal artery presenting with transient ischemia of the vertebrobasilar system: Case report. Neurol Med Chir (Tokyo). 2010. 50: 921-4
11. Ouriel K, Green RM, DeWeese JA. Anomalous carotid-basilar anastomoses in cerebrovascular surgery. J Vasc Surg. 1988. 7: 774-7
12. Ryu B, Ishikawa T, Hashimoto K, Shimizu M, Yagi S, Shimizu T. Internal carotid artery stenosis with persistent primitive hypoglossal artery treated with carotid artery stenting: A case report and literature review. Neuroradiol J. 2016. 29: 115-21
13. Silva CF, Hou SY, Kühn AL, Whitten RH, Wakhloo AK. Double embolic protection during carotid artery stenting with persistent hypoglossal artery. BMJ Case Rep. 2013. 2013: bcr2013010709
14. Tonegawa T, Ohmori Y, Hitoshi Y, Yoshida K. Carotid artery stenting to treat internal carotid artery stenosis with persistent primitive hypoglossal artery: A case report. Jpn J Stroke. 2020. 42: 275-9
15. Vlychou M, Georganas M, Spanomichos G, Kanavaros P, Artinopoulos C, Zavras GM. Angiographic findings and clinical implications of persistent primitive hypoglossal artery. BMC Med Imaging. 2003. 3: 2
16. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ. Protected carotidartery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004. 351: 1493-501
17. Yamada K, Yoshimura S, Miura M, Kanamaru T, Shindo S, Uchida K. Potential of new-generation double-layer micromesh stent for carotid artery stenting in patients with unstable plaque: A preliminary result using OFDI analysis. World Neurosurg. 2017. 105: 321-6
18. Zhang L, Song G, Chen L, Jiao L, Chen Y, Wang Y. Concomitant asymptomatic internal carotid artery and persistent primitive hypoglossal artery stenosis treated by endovascular stenting with proximal embolic protection. J Vasc Surg. 2016. 63: 237-40