- Department of Neurosurgery, University of Arizona, Phoenix/Banner University Medical Center, Arizona, United States
- Department of Neurosurgery, University of Arizona, Phoenix, Arizona, United States.
- Department of Spine Surgery, University of Arizona, Phoenix, Arizona, United States.
Correspondence Address:
Julie Mayeku, Department of Neurosurgery, University of Arizona, Phoenix/ Banner University Medical Center, Phoenix, Arizona, United States.
DOI:10.25259/SNI_934_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Julie Mayeku1, Esteban Quiceno1, Christina Cannata1, Giovanni Barbagli1, Amna Hussein1, Nikhil Dholaria1, Michael Prim2, Ali A. Baaj3. Subfascial drains are safe and effective in preventing postoperative cerebrospinal fluid leaks after intradural spine tumor surgery. 12-Jan-2024;15:8
How to cite this URL: Julie Mayeku1, Esteban Quiceno1, Christina Cannata1, Giovanni Barbagli1, Amna Hussein1, Nikhil Dholaria1, Michael Prim2, Ali A. Baaj3. Subfascial drains are safe and effective in preventing postoperative cerebrospinal fluid leaks after intradural spine tumor surgery. 12-Jan-2024;15:8. Available from: https://surgicalneurologyint.com/surgicalint-articles/12705/
Abstract
Background: Delayed cerebrospinal fluid (CSF) leaks are a known complication following intradural spinal tumor surgery. The placement of subfascial drains in these patients undergoing requisite intradural surgery is controversial. Here, we demonstrated that placing a subfascial drain on partial suction for 48 h, with early ambulation, proved to be safe and effective in preventing early/delayed recurrent CSF fistulas.
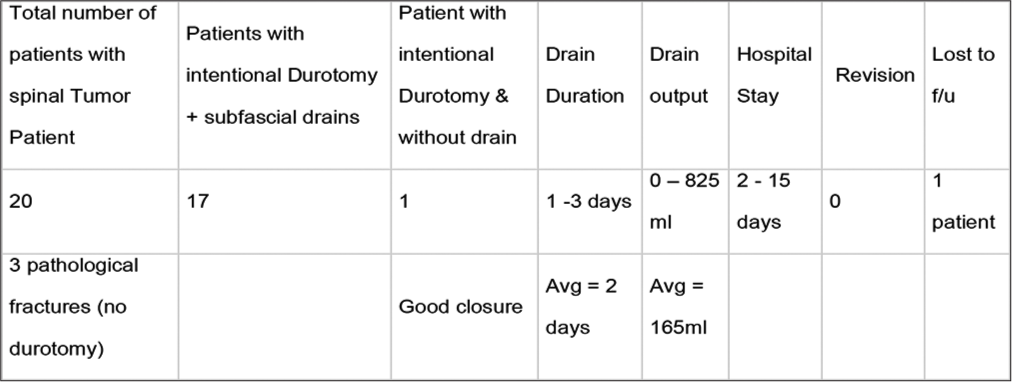
Methods: Medical records of 17 patients undergoing surgery for intradural spinal tumors over a 30-month were reviewed. All patients underwent intradural tumor resection followed by primary dural closure, placement of Gelfoam in a non-compressive fashion, application of fibrin sealant, and utilization of a subfascial drain placed on partial suction for 48 h postoperatively. Patients are mobilized the morning following surgery. We tracked the incidence of postoperative recurrent CSF leaks, over drainage, infection, wound dehiscence, pseudo meningocele formation, and the reoperation rate.
Results: For the 17 patients, our programmed average utilization of subfascial drains was 48 h. Moreover, the average drain output was 165 mL. Over the 1-year follow-up period, no patient developed a recurrent early/ delayed CSF leak, there were no wound complications, nor need for revision surgery.
Conclusion: Utilizing subfascial drains on partial suction following the resection of intradural spinal tumors with primary dural closure proved to be safe and effective.
Keywords: Intentional durotomy, Intradural spinal tumors, Postoperative cerebrospinal fluid leak, Subfascial drains
INTRODUCTION
Delayed cerebrospinal fluid (CSF) leak following the resection of intradural spinal tumors may lead to early/delayed recurrent fistulas, over drainage, infection, wound dehiscence, pseudo meningocele, intracranial hemorrhage, and reoperations. Recurrent CSF leaks contribute to the intraoperative times, postoperative length of hospital stay, and perioperative costs.[
MATERIALS AND METHODS
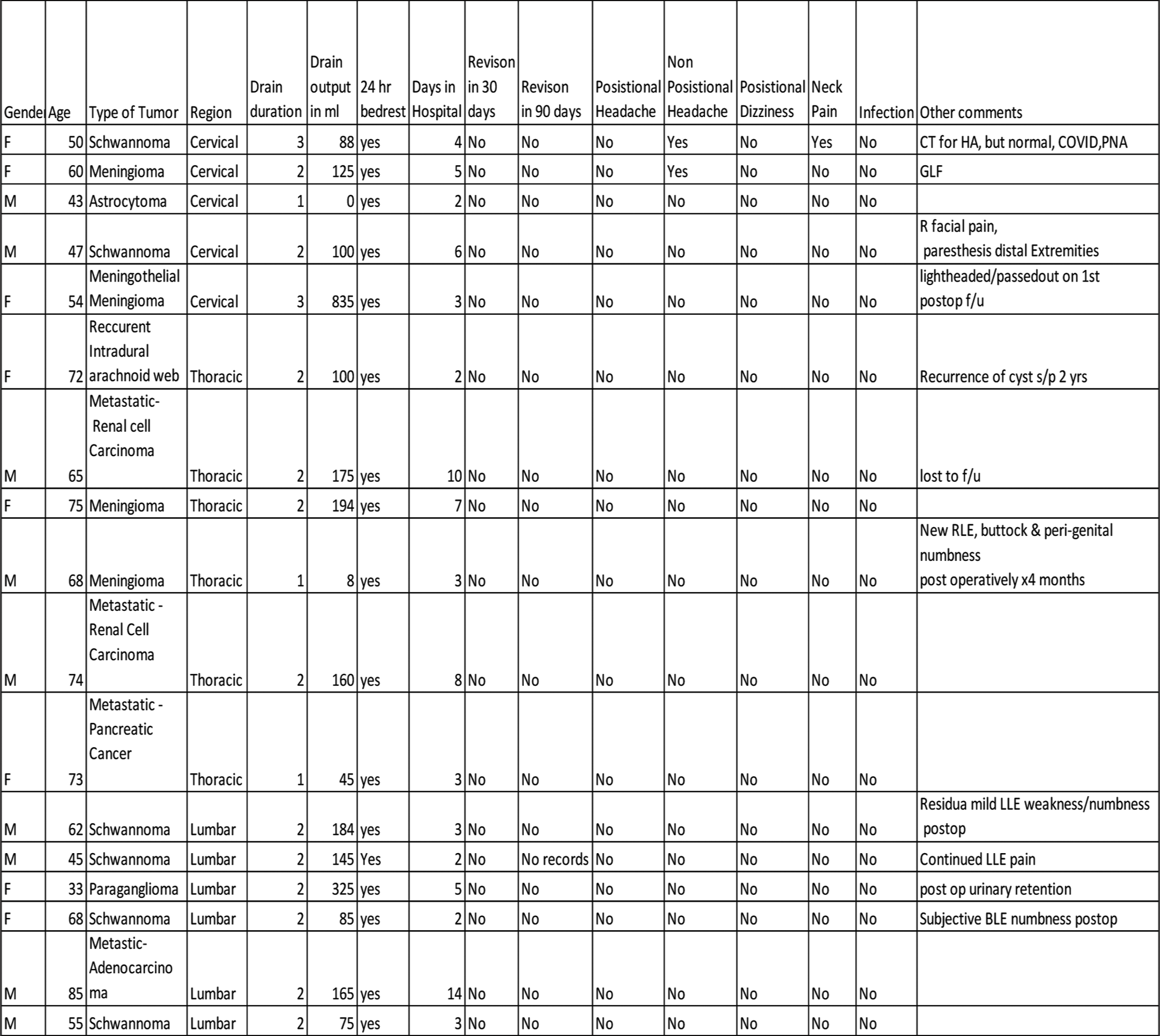
Seventeen patients who met multiple inclusion criteria underwent the resection of intradural tumors; they were followed over an average 30-month postoperative period [
Surgical technique and protocol
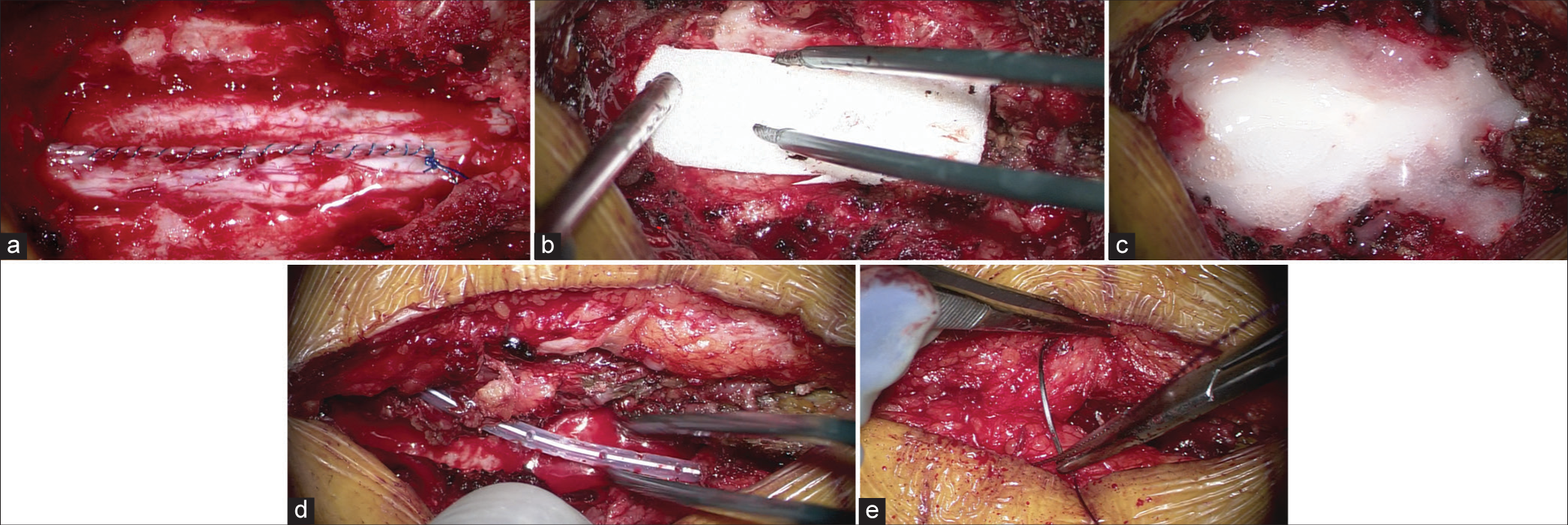
After tumor resection, primary dural closure was performed under the operating microscope using a running simple 5-0 Prolene suture. Next, Gelfoam and fibrin sealant were applied over the dura in a non-compressive fashion, followed by the application of an intraoperative subfascial drain placed on “partial suction” for 48 postoperative hours; routine closure followed using Polydioxanone Stratafix 2-0, and VICRYL 3-0. Patients were mobilized the morning after surgery [
It should be noted that placement of Gelfoam, particularly under a lamina, is not advisable and can be contra-indicated. In our technique, Gelfoam is placed in a non-compressive fashion and not under the lamina. We believe that this is more cost-effective and may have better absorptive/sealant properties than standard dural substitutes.
RESULTS
Subfascial drains were put in place for between 1 and 3 days, 82% of them for only two days; drain output averaged 165 mL. The average length of stay was five days (range: 2 days–15 days). The majority of patients stay for rehab placement, not CSF leak-related complications. One patient was lost to follow-up, and the average length of follow-up was 11.7 months (range 8–12 months). Sixteen patients had ≥12 months of follow-up [
Adverse events/complications
Postoperatively, one patient had nonpositional headaches, one had nonpositional head and neck pain, and one had neck pain. Note the patient with a headache and neck pain was later diagnosed with COVID pneumonia. No surgical revisions were required for delayed CSF leaks occurring between 30 and 90 days following surgery.
DISCUSSION
Primary dural closure
Few studies investigate the outcomes following resection of intradural spinal tumors, particularly regarding CSF early/ delayed recurrent leaks and other adverse events. Primary dural closure, various dural closing techniques with/without synthetic patches, grafts, and layered watertight closure with supplemental sealants help reduce the risk of postoperative CSF leaks.
Subfascial drain placement
We believe that placement of subfascial dural closure, even after primary dural closure, helps divert CSF, blood, and serum from the subfascial space. Diverting the right amount of fluid away from the surgical bed by an Subfascial Drain drain on partial rather than full suction facilitates fascial healing;[
CONCLUSION
The use of subfascial drains after intradural spinal tumor surgery proved to be safe and effective.
Ethical approval
Institutional Review Board approval is taken, Number: UA IRBI: STUDY0001817.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Fang Z, Jia YT, Tian R, Liu Y. Subfascial drainage for management of cerebrospinal fluid leakage after posterior spine surgery-a prospective study based on Poiseuille’s law. Chin J Traumatol. 2016. 19: 35-8
2. Lenschow M, Perrech M, Telentschak S, von Spreckelsen N, Pieczewski J, Goldbrunner R. Cerebrospinal fluid leaks following intradural spinal surgery-risk factors and clinical management. Front Surg. 2022. 9: 959533
3. Niu T, Lu DS, Yew A, Lau D, Hoffman H, McArthur D. Postoperative cerebrospinal fluid leak rates with subfascial epidural drain placement after intentional durotomy in spine surgery. Glob Spine J. 2016. 6: 780-5
4. Ropper AE, Huang KT, Ho AL, Wong JM, Nalbach SV, Chi JH. Intraoperative cerebrospinal fluid leak in extradural spinal tumor surgery. Neurospine. 2018. 15: 338-47
5. Shapiro SA, Scully T. Closed continuous drainage of cerebrospinal fluid via a lumbar subarachnoid catheter for treatment or prevention of cranial/spinal cerebrospinal fluid fistula. Neurosurgery. 1992. 30: 241-5
6. Tan LA, Takagi I, Straus D, O’Toole JE. Management of intended durotomy in minimally invasive intradural spine surgery: Clinical article. J Neurosurg Spine. 2014. 21: 279-85
7. Walid MS, Abbara M, Tolaymat A, Davis JR, Waits KD, Robinson JS. The role of drains in lumbar spine fusion. World Neurosurg. 2012. 77: 564-8
8. Woodroffe RW, Nourski KV, Helland LC, Walsh B, Noeller J, Kerezoudis P. Management of iatrogenic spinal cerebrospinal fluid leaks: A cohort of 124 patients. Clin Neurol Neurosurg. 2018. 170: 61-6