- Department of Neurology, The Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University, Luzhou City, Sichuan, China.
- Department of Blood Transfusion, The Affiliated Hospital of Southwest Medical University, Luzhou City, Sichuan, China.
Correspondence Address:
Jin Si Yang, Department of Neurology, The Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University, Luzhou City, Sichuan, China.
Zu Tian Liu Department of Neurology, The Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University, Luzhou City, Sichuan, China.
DOI:10.25259/SNI_997_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Li Chen1, Yu Shi Deng1, Lan Yu Wang2, Xi Quan Mao1, De Chou Zhang1, Zu Tian Liu1, Jin Si Yang1. Successful endovascular thrombectomy using solitaire FR stent with intermediate catheter assisting technique for acute persistent primitive trigeminal artery and basilar artery occlusion: A case report and literature review. 15-Mar-2024;15:93
How to cite this URL: Li Chen1, Yu Shi Deng1, Lan Yu Wang2, Xi Quan Mao1, De Chou Zhang1, Zu Tian Liu1, Jin Si Yang1. Successful endovascular thrombectomy using solitaire FR stent with intermediate catheter assisting technique for acute persistent primitive trigeminal artery and basilar artery occlusion: A case report and literature review. 15-Mar-2024;15:93. Available from: https://surgicalneurologyint.com/surgicalint-articles/12796/
Abstract
Background: The persistent primitive trigeminal artery (PPTA) is a persistent embryological carotid-basilar connection. Endovascular thrombectomy (EVT) for hypoplastic PPTA occlusion is a challenge. This case report aims to describe the successful recanalization of simultaneous occlusions in both the PPTA and basilar artery (BA) using the Solitaire FR (RECO SR)/Stent and Intermediate Catheter Assisting (SWIM) technique in a patient with acute cardiogenic cerebral embolism. To the best of our knowledge, this is the first report of such a case.
Case Description: We present a case of a 70-year-old female patient who presented with acute right-sided hemiparesis and altered consciousness. Digital subtraction angiography confirmed the occlusion of both the distal portion of the PPTA and the BA. The patient underwent EVT using the SWIM technique, resulting in successful recanalization and significant improvement in the patient’s condition.
Conclusion: This case report demonstrates the successful application of the SWIM technique in achieving recanalization and improving outcomes in a patient with simultaneous occlusion of the acute PPTA and BA. These findings support the potential use of EVT in similar cases.
Keywords: Acute cardiogenic cerebral embolism, Basilar artery, Endovascular thrombectomy, Occlusion, Persistent primitive trigeminal artery, Solitaire FR stent with intermediate catheter assisting technique
INTRODUCTION
The persistent primitive trigeminal artery (PPTA) is a rare embryological vascular anomaly that persists into adulthood.[
Addressing ischemic strokes related to the PPTA presents distinct complexities for clinical neurologists.[
The Solitaire FR (RECO SR)/Stent with Intermediate Catheter Assisting (SWIM) technique has emerged as a promising solution for these challenges. The SWIM technique is defined by its ability to navigate through tortuous and fragile blood vessels, minimizing the risk of proximal and distal embolisms, as well as reducing the potential for mechanical damage to the vessel wall.[
In this report, we present a compelling case of cerebral vascular occlusion successfully treated using the SWIM technique. Our patient presented with acute right-sided hemiparesis and altered consciousness. Diagnostic imaging confirmed the occlusion of the distal portion of PPTA and BA. Following the application of the SWIM technique, our patient experienced successful recanalization and significant improvement in her condition. This case highlights the SWIM technique’s effectiveness in addressing cerebral vascular occlusions, underscoring its potential as a valuable treatment modality for such challenging cases.
CASE PRESENTATION
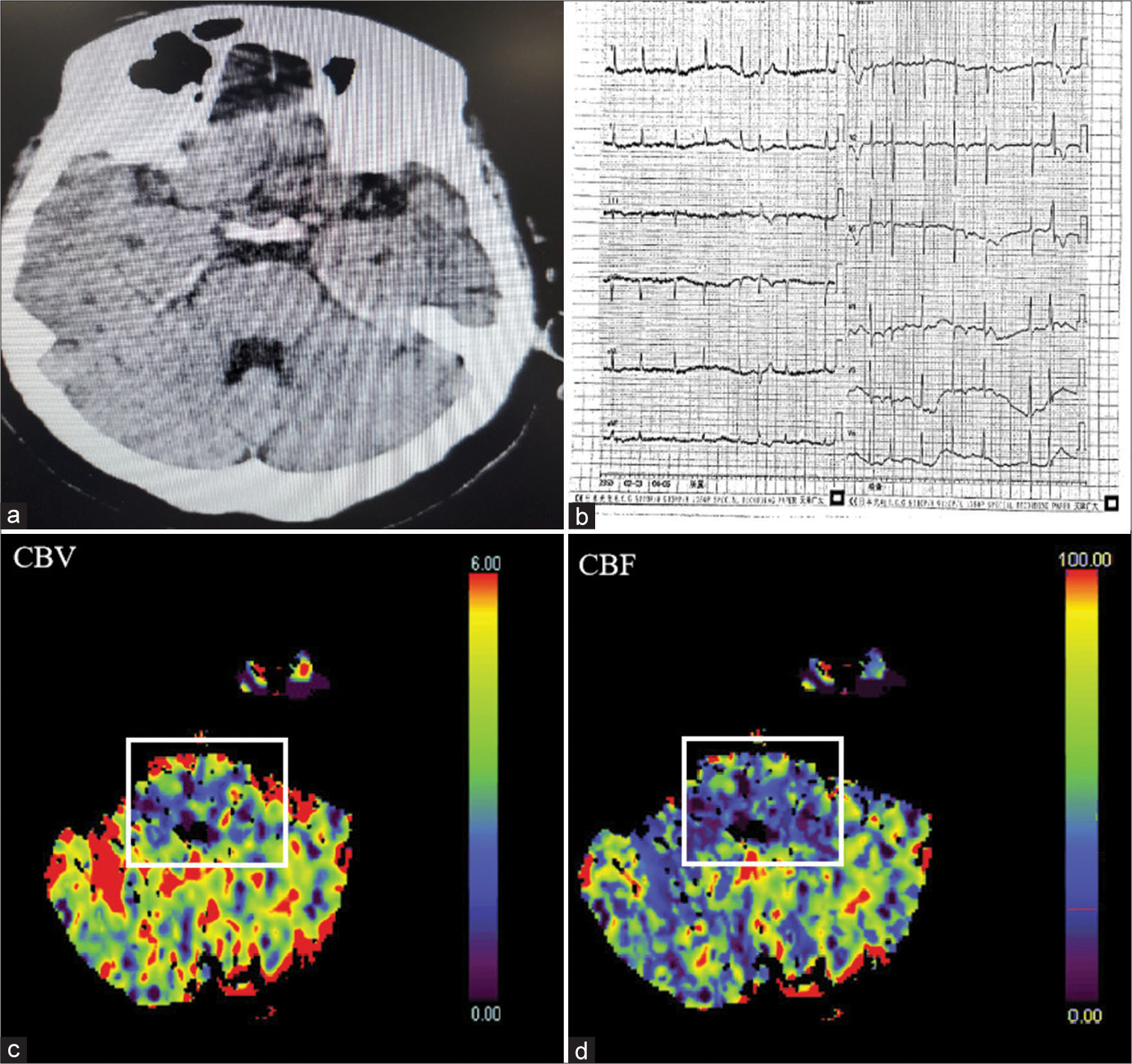
The patient, a 70-year-old female, presented with acute right-sided hemiparesis and altered consciousness, with a duration of 4 h and 46 min. On admission, her Glasgow Coma Scale (GCS) score was 11, and she scored four on the water swallow test. The National Institutes of Health Stroke Scale score was 14, reflecting the severity of her symptoms. She had a history of hypertension but denied diabetes mellitus, heart disease, and significant trauma or surgery. Noncontrast computed tomography (CT) on admission showed no evidence of hemorrhage or early ischemia [
Figure 1:
(a) Computed tomography (CT) showed no signs of hemorrhage or early ischemia; (b) electrocardiogram showed the cardiogram feature of atrial fibrillation; (c) preoperative CT perfusion (CTP)-cerebral blood volume (CBV) image demonstrated acute cerebral infarction involving the brainstem; solid lines of squares represented the ischemic core area with CBV <1.2 mL/100 mL; (d) preoperative CTP-cerebral blood flow (CBF) image displayed an area of penumbra in the brainstem; solid lines of squares represented the penumbra area with CBF <27 mL/100 g/min.
However, approximately 30 min after the completion of UK treatment, her condition abruptly worsened, possibly due to a recurrent cerebral embolism caused by the dislodgment of a cardiac thrombus. At this stage, CT perfusion analysis was conducted using syngo.via software (Siemens, Erlangen, Germany). The analysis revealed a significant volume of penumbra (70 mL), the region of potentially salvageable brain tissue, and ischemic core (10 mL), the irreversibly damaged brain tissue, in the brain stem and cerebellar hemispheres [
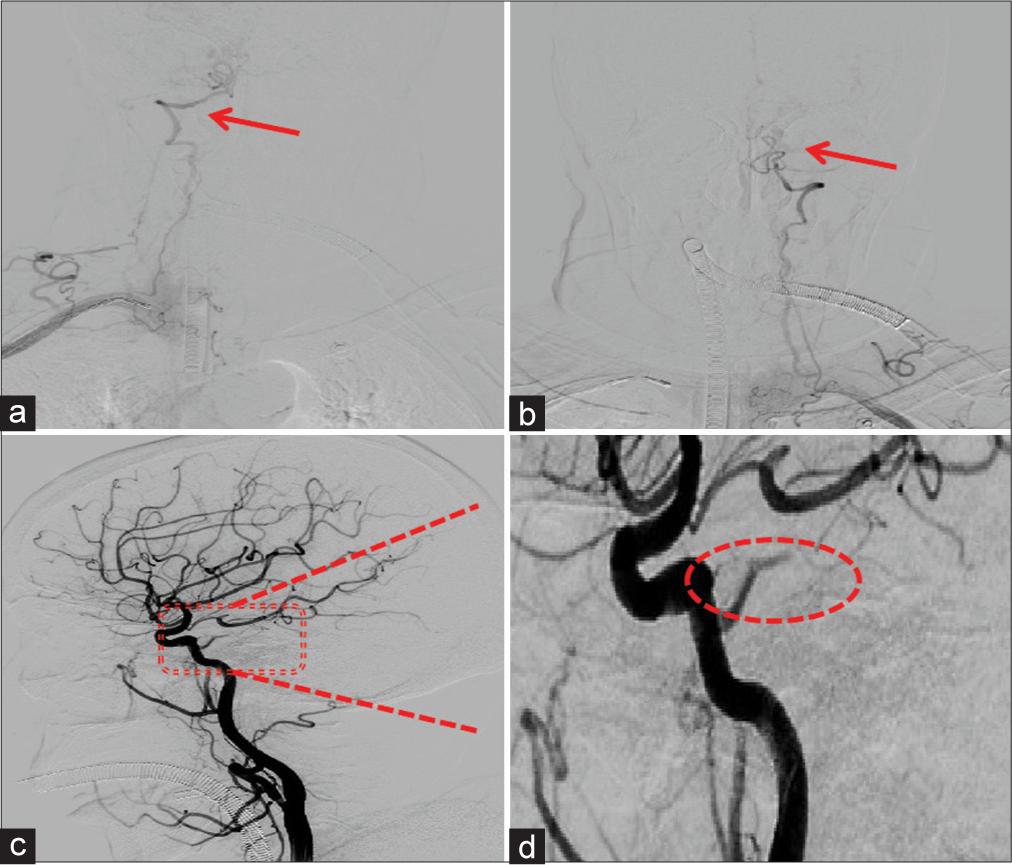
Emergent digital subtraction angiography (DSA) revealed the following results: the termination of both the left vertebral artery (VA) and the right VA was observed in the posterior inferior cerebellar artery [
Figure 2:
(a) Digital subtraction angiography (DSA) image indicating the left posterior inferior cerebellar artery (PICA) with a red arrow; (b) DSA image illustrating the hypoplastic right PICA (red arrow); (c) DSA image displaying the right posterior cerebral artery(PCA) and middle cerebral artery(MCA); the red dotted square highlights the presence of the persistent primitive trigeminal artery (PPTA) arising from the cavernous Internal carotid artery( ICA). In (d), the red dotted square is enlarged to reveal the absence of the terminal portions of the PPTA, as indicated by the red dotted oval curve.
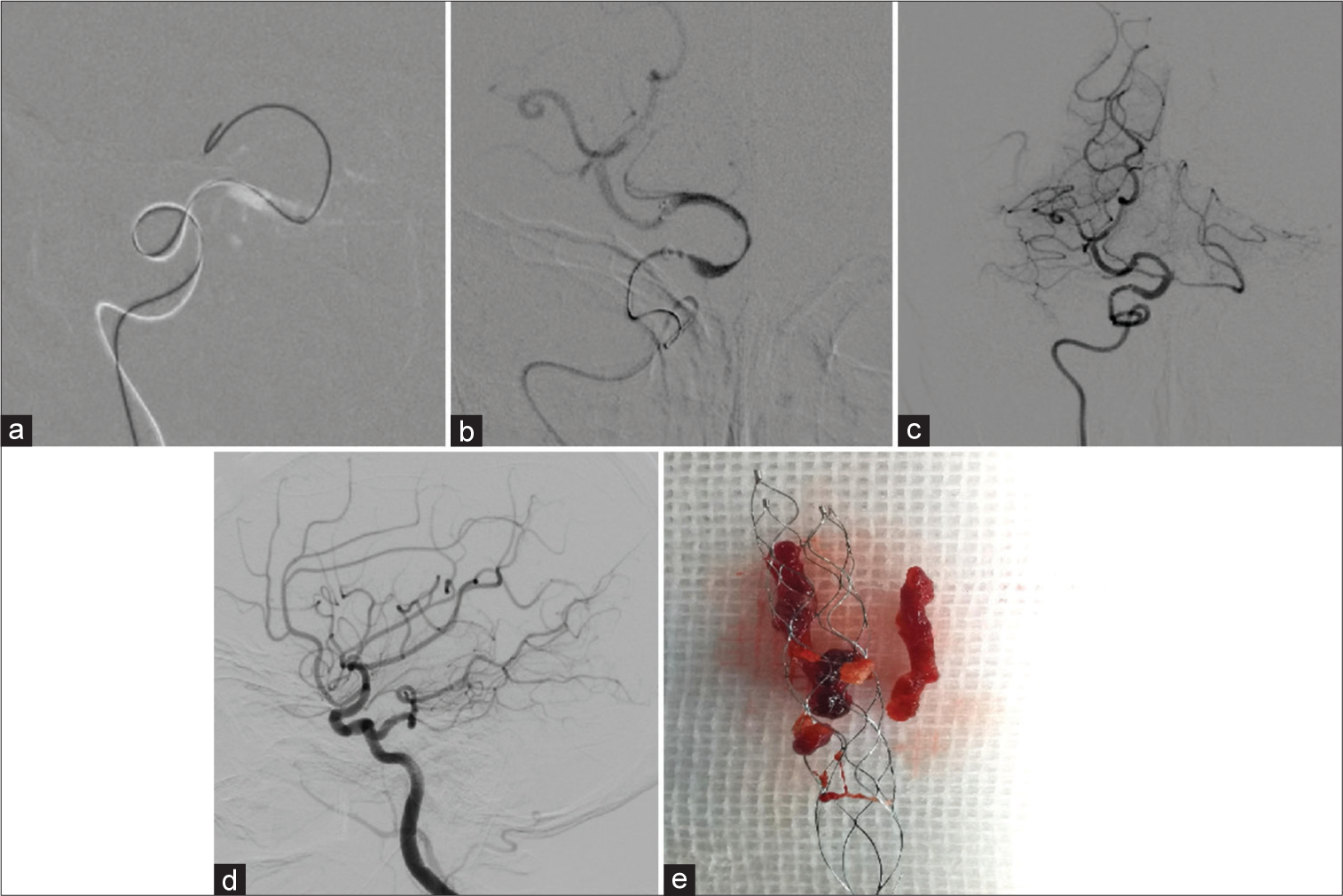
To initiate the procedure, we carefully positioned an 8F guide catheter (Boston Scientific, USA) at the origin of the right ICA, serving as the entry point for the intervention. Subsequently, we advanced an AXS Catalyst 6 distal access catheter (Stryker, USA) in conjunction with an XT-27 microcatheter (Stryker, USA), using a 0.014-inch synchro microwire (Stryker, USA). This intricate setup allowed for precise access to the occluded area associated with the PPTA, as depicted in
Figure 3:
(a) Successful passage of a micro guidewire through the occlusion site, reaching the posterior cerebral artery (PCA); (b) images illustrating the basilar artery (BA) and PCA after deploying a revascularization with the embolization of a carotid occlusion (RECO) 4 ×20 mm stent, leading to vessel reperfusion; (c) visualization of the recanalized BA after stent retrieval; (d) digital subtraction angiography image depicting the presence of the PPTA, BA, PCA, middle cerebral artery, and PCA following the successful recanalization of the persistent primitive trigeminal artery (PPTA) and BA; (e) extraction of a firm thrombus from the occluded PPTA.
The XT-27 microcatheter was then expertly navigated to the distal end of the thrombus, facilitated by the synchro 14. Following this, we introduced a RECO 4 × 20 mm stent retriever (Medtronic, USA) into the XT-27 microcatheter, positioning it strategically across the thrombus [
To optimize the effectiveness of thrombus removal, we performed manual aspiration concurrently with the inflation of the Optimo balloon, creating a reverse flow. Finally, both the RECO stent retriever and AXS Catalyst 6 were meticulously withdrawn from the procedure. DSA was then employed to assess the results.
DSA confirmed the complete recanalization of the PPTA and the BA, achieving modified thrombolysis in cerebral infarction Grade 3 blood flow, as illustrated in
DISCUSSION
PPTA is a rare vascular anomaly resulting from a persistent carotid-to-BA connection, typically regressing during embryonic development by day 14. However, in some cases, PPTA persists beyond this stage.[
Diagnosing PPTA and associated occlusions poses unique clinical challenges. Various imaging modalities, including DSA, computed tomography angiography (CTA), and magnetic resonance angiography (MRA), have been employed for diagnosis. However, thrombosis of the PPTA remains rare due to its distinctive anatomical characteristics.[
Our case presents a rare scenario where cardiac thrombi migrated to the brain, causing the simultaneous occlusion of both the PPTA and the BA, a previously undocumented occurrence. Clinical guidelines recommend prompt implementation of complementary treatments, including thrombolysis and interventional therapy, on the diagnosis of acute cerebral infarction.[
A detailed analysis of the angiography results revealed a PPTA originating from the right ICA and an occlusion in close proximity. Surprisingly, the PPTA was supplying the BA instead of the VA, necessitating a different approach. By selecting the ICA as the access route for EVT, we achieved successful recanalization of the occluded vessels. This case serves as an instructive example of the importance of tailored treatment strategies for unique vascular anatomies.
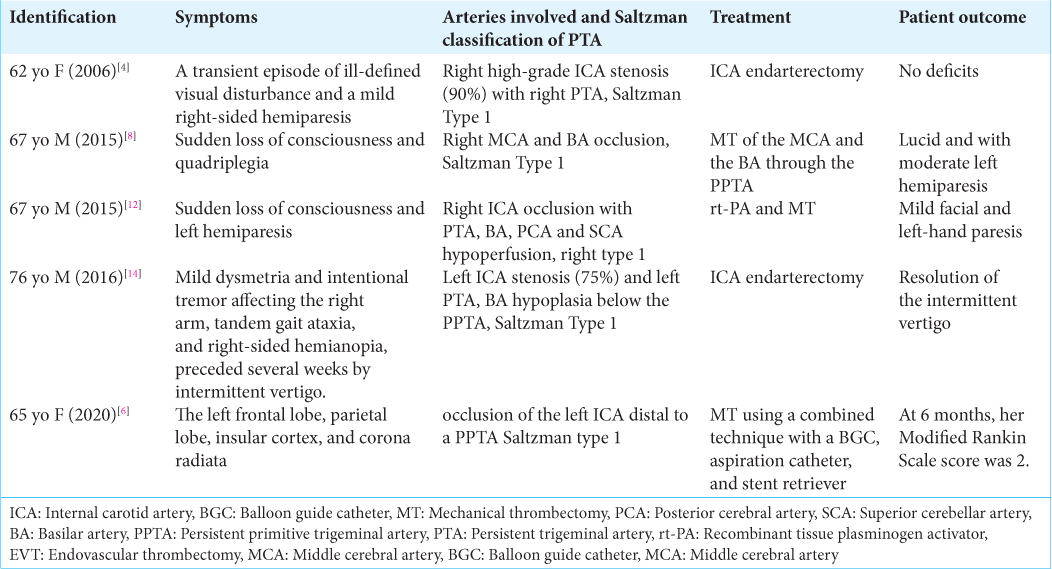
PPTA-related stroke poses a management challenge, marked by diverse outcomes documented in the existing literature. Our report delves into the contemporary treatment landscape for PPTA-related stroke, providing a comprehensive overview before introducing the innovative SWIM. Various treatment modalities have been explored for PPTA-related stroke, each yielding distinct outcomes. Medical management strategies vary, encompassing anticoagulation therapy and antiplatelet agents to prevent thromboembolic events associated with PPTA. In the acute phase, treatment may involve thrombolysis,[
Against this backdrop of existing treatments, our case study introduces SWIM as a novel approach to PPTA-related stroke. SWIM aims to mitigate the risk of lingering symptoms and complications observed in prior cases. Our literature review, which includes a thorough examination of various treatment approaches, underscores the scarcity of reports on the successful application of EVT for PPTA-related stroke. To date, only five relevant cases have been documented, as summarized in
Known for its high recanalization rate and rapid restoration of cerebral blood perfusion,[
CONCLUSION
This case illustrates the complexity and uniqueness of PPTA-related stroke, emphasizing the importance of tailored treatment approaches. It expands the limited body of evidence regarding the successful use of EVT, particularly the SWIM technique, in addressing PPTA occlusions. This case is the first reported instance demonstrating the successful application of the SWIM technique for PPTA-related stroke, further underscoring its potential as a valuable tool in the management of such cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
This work was supported by the 72nd Batch of General Funding, second class from the China Postdoctoral Science Foundation (Grant Number: 2022M722640), the Luzhou Science and Technology Program (Grant Number: 2021-JYJ-53), the Sichuan Administration of Traditional Chinese Medicine (Grant Number: 2021MS515), and the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine (Grant Number: ZYYCXTD-C-202207).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Azab W, Delashaw J, Mohammed M. Persistent primitive trigeminal artery: A review. Turk Neurosurg. 2012. 22: 399-406
2. Fields WS. The significance of persistent trigeminal artery. Carotid-Basilar anastomosis. Radiology. 1968. 91: 1095-101
3. Ferreira A, Coelho PS, Cruz VT. Persistent trigeminal artery in a patient with posterior circulation stroke treated with rt-PA: Case report. BMC Neurol. 2019. 19: 257
4. Foerch C, Berkefeld J, Halbsguth A, Ziemann U, Neumann-Haefelin T. Brain stem infarction caused by proximal internal carotid artery stenosis in a patient with a persisting primitive trigeminal artery. Cerebrovasc Dis. 2006. 22: 200-2
5. Hankey GJ. Endovascular therapy for acute basilar artery occlusion. Circulation. 2022. 146: 18-20
6. Horio Y, Fukuda K, Yoshinaga T, Takeyama R, Fukumoto H, Sato K. Successful mechanical thrombectomy using a combined technique for internal carotid artery occlusion with persistent primitive trigeminal artery. Surg Neurol Int. 2020. 11: 345
7. Ito Y, Watanabe H, Niwa H, Hakusui S, Ando T, Yasuda T. The protective effect of a persistent trigeminal artery on brain stem infarctions: A follow-up case report. Intern Med. 1998. 37: 334-7
8. Imahori T, Fujita A, Hosoda K, Kohmura E. Acute ischemic stroke involving both anterior and posterior circulation treated by endovascular revascularization for acute basilar artery occlusion via persistent primitive trigeminal artery. J Korean Neurosurg Soc. 2016. 59: 400-4
9. Liu T, Ren S, Chen L, Deng S, Xu H, Wu Y. Successful endovascular thrombectomy 8 days after onset of acute ischemic stroke: A case report. Heliyon. 2023. 9: e13259
10. Li D, Chen Z, Fan T, Zhao X, Qi H, Liang X. Cross-circulation thrombectomy through posterior communicating artery for acute middle cerebral artery occlusion using Solitaire FR stent with intermediate catheter assisting technique. Neurol Neurochir Pol. 2021. 55: 403-6
11. Meckel S, Spittau B, McAuliffe W. The persistent trigeminal artery: Development, imaging anatomy, variants, and associated vascular pathologies. Neuroradiology. 2013. 55: 5-16
12. Mulder M, Lycklama À Nijeholt GJ, Dinkelaar W, de Rooij T, van Es A. Thrombectomy in posterior circulation stroke through persistent primitive trigeminal artery: A case report. Interv Neuroradiol. 2015. 21: 715-8
13. Neurology Branch, Chinese Medical Association; Cerebrovascular Diseases Group, Neurology Branch of Chinese Medical Associati. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol. 2018. 51: 666-82
14. Parthasarathy R, Derksen C, Saqqur M, Khan K. Isolated intermittent vertigo: A presenting feature of persistent trigeminal artery. J Neurosci Rural Pract. 2016. 7: 161-3
15. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke. 2018. 49: e46-110
16. Sadashiva N. Microvascular decompression for trigeminal neuralgia with concomitant persistent primitive trigeminal artery. Neurol India. 2021. 69: 826-8
17. Saltzman GF. Patent primitive trigeminal artery studied by cerebral angiography. Acta Radiol. 1959. 51: 329-36
18. Singh J, Wolfe SQ, Janjua RM, Hedayat H, Burnette C. Anchor technique: Use of stent retrievers as an anchor to advance thrombectomy catheters in internal carotid artery occlusions. Interv Neuroradiol. 2015. 21: 707-9
19. Sreenivasan S, Agarwal N, Roychowdhury S, Khandelwal P, Sun H, Singla A. Management paradigms of persistent primitive trigeminal artery aneurysms: A systematic review and analysis of techniques and complications from 1960s to 2022: From conservative to surgical to endovascular, how far along the right path are we?. Interv Neuroradiol. 2023. p. 15910199221150471
20. Tasdemir R, Yasin S, Cihan OF. Basilar artery formed by persistent primitive trigeminal artery: A case report. Surg Radiol Anat. 2023. 45: 333-5
21. Tyagi G, Sadashiva N, Konar S, Aravinda HR, Saini J, Shukla D. Persistent trigeminal artery: Neuroanatomic and clinical relevance. World Neurosurg. 2020. 134: e214-23
22. Wang Y, Yu J. Clinical importance of the persistent primitive trigeminal artery in vascular lesions and its role in endovascular treatment. Front Neurol. 2022. 13: 928608