- Department of Neurosurgery, Kawano Neurosurgery Hospital, Morimachinishi, Oita, Japan.
- Department of Neurosurgery, Fukuoka University Hospital and School of Medicine, Nanakuma Jonan-Ku, Fukuoka, Japan.
Correspondence Address:
Yoshinobu Horio
Department of Neurosurgery, Fukuoka University Hospital and School of Medicine, Nanakuma Jonan-Ku, Fukuoka, Japan.
DOI:10.25259/SNI_657_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshinobu Horio1, Kenji Fukuda2, Takaya Yoshinaga1, Ryuhei Takeyama1, Hironori Fukumoto1, Kiminori Sato1, Yoshihisa Kawano1, Tooru Inoue2. Successful mechanical thrombectomy using a combined technique for internal carotid artery occlusion with persistent primitive trigeminal artery. 15-Oct-2020;11:345
How to cite this URL: Yoshinobu Horio1, Kenji Fukuda2, Takaya Yoshinaga1, Ryuhei Takeyama1, Hironori Fukumoto1, Kiminori Sato1, Yoshihisa Kawano1, Tooru Inoue2. Successful mechanical thrombectomy using a combined technique for internal carotid artery occlusion with persistent primitive trigeminal artery. 15-Oct-2020;11:345. Available from: https://surgicalneurologyint.com/surgicalint-articles/10332/
Abstract
Background: The prevalence of persistent primitive trigeminal artery (PPTA) has been reported to be 0.1–0.6%. We report the successful recanalization of internal carotid artery (ICA) without embolization to new vascular territory (ENT) using a combined technique in a case of ICA occlusion with PPTA.
Case Description: A 65-year-old female presented with sudden consciousness disorder. The Glasgow Coma Scale score was 7 (E1, V1, M5) and National Institutes of Health Stroke Scale score was 28. Magnetic resonance diffusion-weighted imaging showed areas of high signal intensity in the left frontal lobe, parietal lobe, insular cortex, and corona radiata. Magnetic resonance angiography showed occlusion of the left ICA distal to a PPTA. We performed mechanical thrombectomy (MT) using a combined technique with a balloon guide catheter (BGC), aspiration catheter, and stent retriever and achieved complete recanalization without ENT. The patient experienced a good postoperative recovery course. At 6 months, her Modified Rankin Scale score was 2.
Conclusion: MT using a combined technique with BGC would be useful to prevent embolization to the posterior circulation through the PPTA in cases of ICA occlusion with PPTA.
Keywords: Acute ischemic stroke, Mechanical thrombectomy, Persistent primitive trigeminal artery
INTRODUCTION
The reported prevalence of persistent primitive trigeminal artery (PPTA) ranges between 0.1% and 0.6%.[
If ENT occurs in a patient with a PPTA, the patient may suffer from basilar artery (BA) occlusion with poor outcome.[
Various combined techniques using an aspiration catheter and stent retriever have been reported to show good results.[
CASE DESCRIPTION
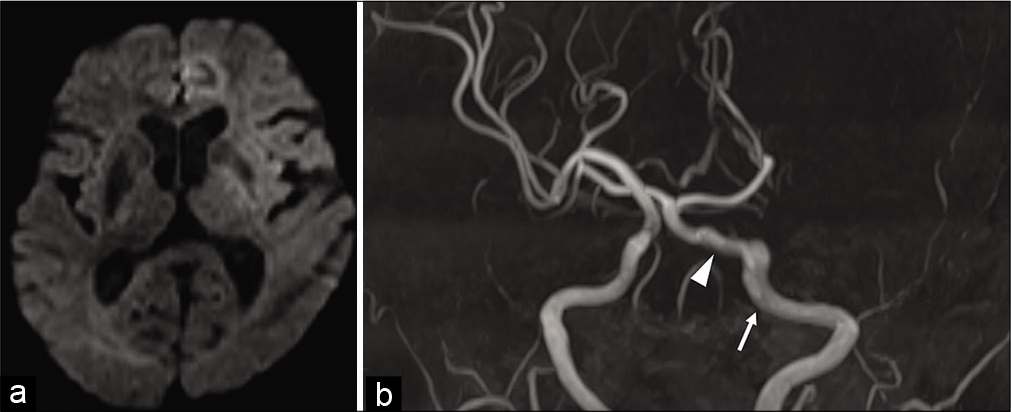
A 65-year-old female presented with sudden consciousness disorder. She had a history of surgery for arterial septal defect closure, mitral valve angioplasty for mitral regurgitation, and coronary artery bypass graft surgery for coronary artery stenosis. Medications at the time of admission included clopidogrel 75 mg daily for coronary artery stenosis. Her Glasgow Coma Scale score was 7 (E1, V1, M5) and National Institutes of Health Stroke Scale score was 28. Electrocardiography revealed atrial fibrillation. Computed tomography of the head showed no evidence of early ischemic change. Magnetic resonance diffusion-weighted imaging (DWI) showed regions of high signal intensity in the left frontal lobe, parietal lobe, insular cortex, and corona radiata. The DWI Alberta Stroke Program Early Computed Tomographic Score was 5 [
Figure 1:
(a) Magnetic resonance diffusion-weighted imaging at admission showed regions of high signal intensity in the left frontal lobe, parietal lobe, insular cortex, and corona radiata. (b) Magnetic resonance angiography showed occlusion of the left internal carotid artery (ICA) (white arrow) distal to a persistent primitive trigeminal artery (PPTA) (white arrow head). The vertebral arteries and posterior communicating arteries were hypoplastic bilaterally. The bilateral superior cerebellar and posterior cerebral arteries were fed by the left ICA through the PPTA.
MT procedure
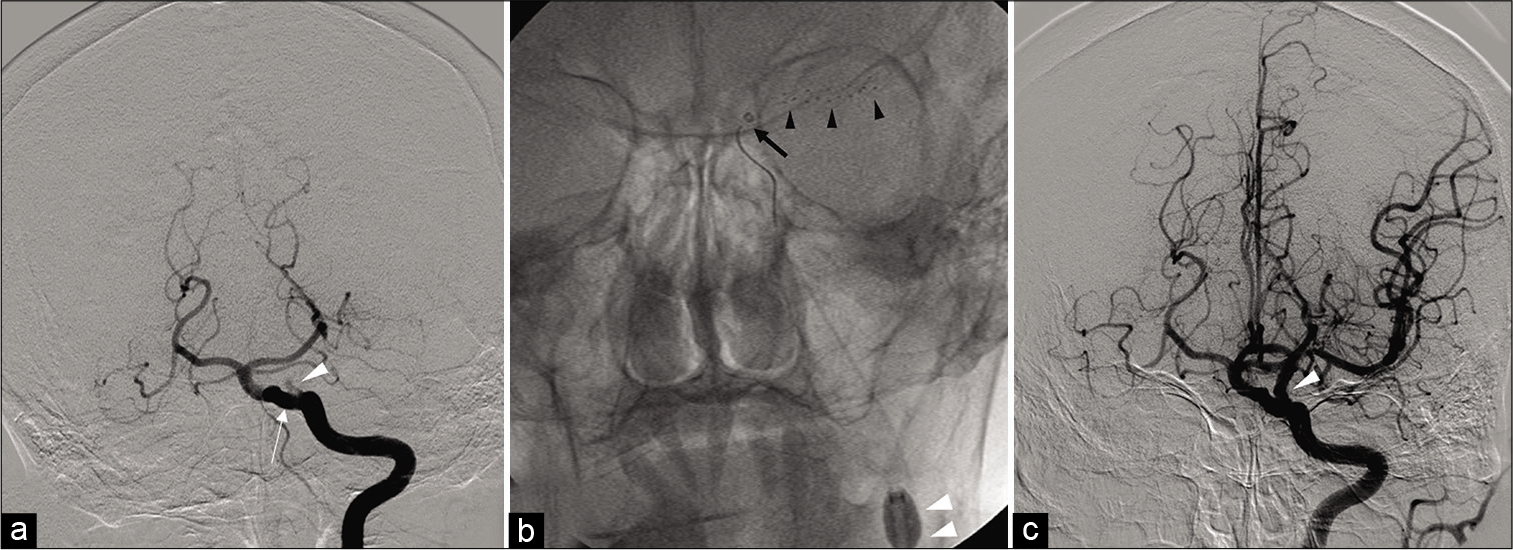
A 9 Fr sheath was inserted into the left femoral artery and a 9 Fr Optimo 90 (Tokai Medical Products, Kasugai, Aichi, Japan) was introduced into the cervical segment of the left ICA. Digital subtraction angiography showed occlusion of the left ICA distal to the ophthalmic artery and a PPTA arising from the cavernous ICA that anastomosed with the BA below the origin of both superior cerebellar arteries (SCAs). The PPTA was feeding the BA and bilateral SCAs and posterior cerebral arteries (PCAs) [
Figure 2:
(a) Digital subtraction angiography (DSA) showed occlusion of the left ICA (white arrow head) distal to a persistent primitive trigeminal artery (white arrow). (b) The Solitaire 4 × 20 mm stent retriever (Medtronic, Minneapolis, Minnesota, USA) (black arrow heads) was deployed. The Marksman microcatheter (Medtronic) was removed and the AXS Catalyst 6 (Stryker, Freemont, California, USA) (black arrow) was introduced proximal to the thrombus. The 9 Fr Optimo (Tokai Medical Products, Kasugai, Aichi, Japan) was inflated (white arrow heads) and the Solitaire and AXS Catalyst 6 were removed together. (c) Postoperative DSA showed complete recanalization of the left ICA (white arrow head).
Postoperative course
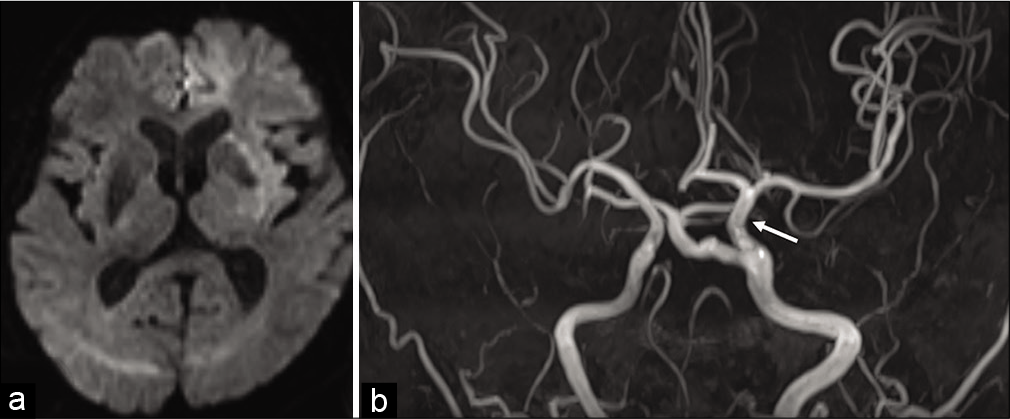
DWI showed no new regions of infarction. MRA showed patency of the left ICA and PPTA [
DISCUSSION
The PPTA is a persistent carotid-vertebrobasilar anastomosis arising from the cavernous ICA and connects with the BA between the origins of the anterior inferior cerebellar arteries (AICAs) and SCAs. PPTAs are classified as medial or lateral according to their clinical course. The medial type enters the posterior fossa from a foramen in the dorsum sellae. The lateral type enters Meckel’s cave, courses posteriorly, bends sharply medially, and connects to the BA.[
Saltzman and Wollschlaeger classified PPTA into three types according to the degree of PCoA development.[
Hiramatsu et al. reported a patient with ICA occlusion with PPTA involvement who presented with ischemia of the posterior circulation.[
Imahori et al. also reported a patient with middle cerebral artery and BA occlusion. MT using Merci Retriever (Concentric Medical, Mountain View, CA, USA) for BA occlusion was performed through PPTA because bilateral VAs were hypoplastic and PPTA was patent. In our case, the location of the occluded vessel was distal to the PPTA. Therefore, it was required to prevent ENT to the posterior circulation through PPTA. When ICA and BA occlusions coexist, the existence of carotid-BA anastomosis should be considered. It is necessary to confirm not only maximum intensity projection imaging but also multiplanar reconstruction imaging of MRA.
MT techniques capable of achieving a high rate of complete recanalization with a low ENT rate have been reported. The BGC contributes to recanalization and prevention of ENT.[
Because prognosis may be worse if the thrombus moves to the BA through the PPTA,[
CONCLUSION
Clinical symptoms and imaging findings are often atypical in the cases of ICA occlusion with PPTA and correct diagnosis may be difficult. A combined MT technique using a BGC would be useful to prevent ENT to the posterior circulation through the PPTA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge the assistance of editorial services that provided language help.
References
1. Brinjikji W, Starke RM, Murad MH, Fiorella D, Pereira VM, Goyal M. Impact of balloon guide catheter on technical and clinical outcomes: A systematic review and meta-analysis. J Neurointerv Surg. 2018. 10: 335-9
2. Fields WS. The significance of persistent trigeminal artery. Carotid-Basilar anastomosis. Radiology. 1968. 91: 1095-101
3. Gasecki AP, Fox AJ, Lebrun LH, Daneault N. Bilateral occipital infarctions associated with carotid stenosis in a patient with persistent trigeminal artery. The collaborators of the North American Carotid Endarterectomy Trial (NASCET). Stroke. 1994. 25: 1520-3
4. Hiramatsu R, Ohnishi H, Kawabata S, Miyachi S, Kuroiwa T. Successful recanalization for internal carotid artery occlusion with persistent primitive trigeminal artery manifesting only as ischemia of the posterior circulation. BMC Neurol. 2016. 16: 41
5. Imahori T, Fujita A, Hosoda K, Kohmura E. Acute ischemic stroke involving both anterior and posterior circulation treated by endovascular revascularization for acute basilar artery occlusion via persistent primitive trigeminal artery. J Korean Neurosurg Soc. 2016. 59: 400-4
6. Klinger-Gratz PP, Schroth G, Gralla J, Jung S, Weisstanner C, Verma RK. Protected stent retriever thrombectomy prevents iatrogenic emboli in new vascular territories. Neuroradiology. 2015. 57: 1045-54
7. Maegerlein C, Berndt MT, Mönch S, Kreiser K, BoeckhBehrens T, Lehm M. Further development of combined techniques using stent retrievers, aspiration catheters and BGC: The PROTECTPLUS technique. Clin Neuroradiol. 2020. 30: 59-65
8. Massari F, Henninger N, Lozano JD, Patel A, Kuhn AL, Howk M. ARTS (Aspiration-Retriever Technique for Stroke): Initial clinical experience. Interv Neuroradiol. 2016. 22: 325-32
9. Maus V, Behme D, Kabbasch C, Borggrefe J, Tsogkas I, Nikoubashman O. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol. 2018. 28: 327-38
10. Mulder M, Lycklama à Nijeholt GJ, Dinkelaar W, De Rooij T, Van Es A, Van Der Kallen BF. Thrombectomy in posterior circulation stroke through persistent primitive trigeminal artery: A case report. Interv Neuroradiol. 2015. 21: 715-8
11. O’Uchi E, O’Uchi T. Persistent primitive trigeminal arteries (PTA) and its variant (PTAV): Analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology. 2010. 52: 1111-9
12. Saltzman GF. Patent primitive trigeminal artery studied by cerebral angiography. Acta Radiol. 1959. 51: 329-36
13. Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): A prospective registry study. Lancet Neurol. 2009. 8: 724-30
14. Weon YC, Choi SH, Hwang JC, Shin SH, Kwon WJ, Kang BS. Classification of Persistent Primitive Trigeminal Artery (PPTA): A reconsideration based on MRA. Acta Radiol. 2011. 52: 1043-51