- Department of Neurosurgery, Sasebo Chuo Hospital, Nagasaki, Japan
- Department of Neurosurgery, Fukuoka University Hospital and Faculty of Medicine, Fukuoka University, Fukuoka, Japan
Correspondence Address:
Toshio Higashi
Department of Neurosurgery, Fukuoka University Hospital and Faculty of Medicine, Fukuoka University, Fukuoka, Japan
DOI:10.4103/2152-7806.163176
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takemoto K, Higashi T, Sakamoto S, Inoue T. Successful sinus restoration for transverse-sigmoid sinus dural arteriovenous fistula complicated by multiple venous sinus occlusions: The usefulness of preoperative computed tomography venography. Surg Neurol Int 18-Aug-2015;6:137
How to cite this URL: Takemoto K, Higashi T, Sakamoto S, Inoue T. Successful sinus restoration for transverse-sigmoid sinus dural arteriovenous fistula complicated by multiple venous sinus occlusions: The usefulness of preoperative computed tomography venography. Surg Neurol Int 18-Aug-2015;6:137. Available from: http://surgicalneurologyint.com/surgicalint_articles/successful-sinus-restoration-for-transverse%e2%80%91sigmoid-sinus/
Abstract
Background:Although sinus restoration for transverse-sigmoid sinus (TSS) dural arteriovenous fistula (DAVF) has rarely been reported over the past decade, its advantage and indication still remain unclear. Herein, we discuss the indications and technical aspects of this therapy with a review of the literature.
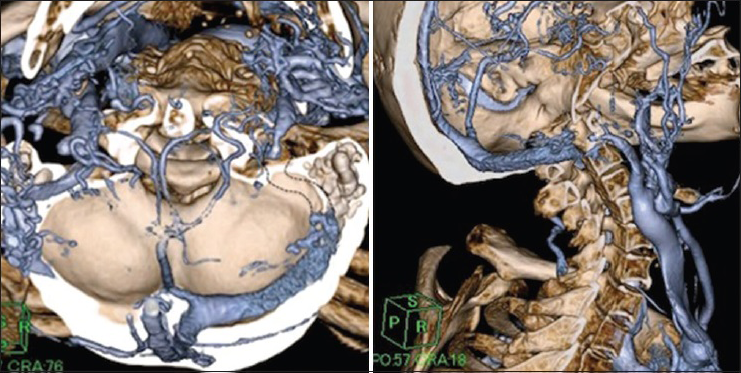
Case Description:A 79-year-old female was referred to our department with generalized convulsion. An angiogram revealed a DAVF at the junction of the right TSS. The right sigmoid and left transverse sinuses were occluded, which resulted in remarkable leptomeningeal venous reflux and cerebral venous congestion. A preoperative computed tomography (CT) venogram precisely revealed the occluded segment of the right sigmoid sinus, which facilitated the sinus restoration with balloon percutaneous transluminal angioplasty and stenting.
Conclusion:Sinus restoration is preferable in patients with severe cerebral venous congestion due to multiple sinus occlusions and/or a restricted collateral venous outlet. CT venography is useful for precise evaluation of the length and configuration of the occluded segment, which thus make it possible to evaluate the feasibility of stenting.
Keywords: Computed tomography venography, dural arteriovenous fistula, sinus restoration, stent, transverse-sigmoid sinus
INTRODUCTION
Treatment of dural arteriovenous fistulas (DAVFs) at the junction of the right transverse-sigmoid sinus (TSS) can include transvenous coil embolization (TVE) of the affected sinus or transarterial embolization (TAE) using onyx, particularly in patients with advanced lesions such as Cognard Type III and IV and Borden Type III.[
CASE REPORT
A 79-year-old female presented with progressive deterioration of her cognitive function over a period of 10 months. She became bedridden and was referred to our department due to convulsive seizure. She scored only three points with a mini-mental state examination (MMSE) at the time of admission. Magnetic resonance imaging diagnosed prominent DAVF in the right transverse sinus. Numerous flow voids corresponding to varicose veins were observed over the superficial and deep surfaces of the brain. A subsequent diagnostic angiogram showed DAVF at the junction of the right TSS fed by several branches originating from the right external carotid artery, involving the middle meningeal artery, occipital artery, posterior auricular artery, and accessory meningeal artery. The tentorial artery arose from the right internal carotid artery also fed the fistulae [Figure
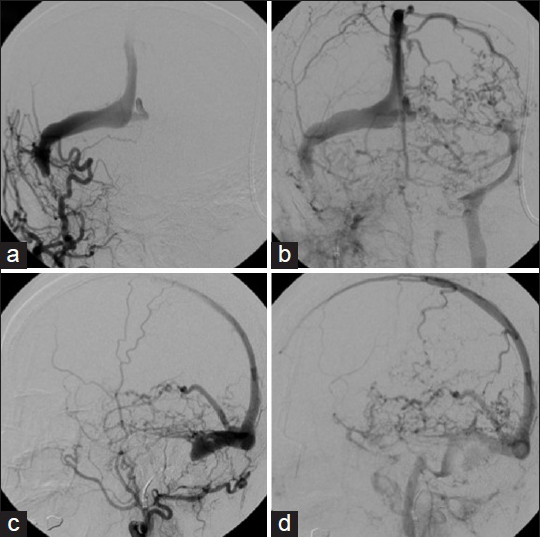
Figure 1
Preoperative angiogram. Right external carotid artery angiogram (a and c: Early phase, b and d: Late phase) showing a transverse-sigmoid sinus dural arteriovenous fistula with occlusive changes in both the right sigmoid sinus and the left transverse sinus. Marked retrograde venous drainage was directed toward the deep venous system through the straight sinus and toward the cerebral hemisphere via the superior sagittal sinus
The cerebral circulatory disturbance was due to venous congestion, which was caused by TSS DAVF and bilateral venous sinus occlusion [
The endovascular procedure was performed under general anesthesia. Bilateral groin access was used. A 4-French diagnostic catheter was advanced into the right external carotid artery to obtain the diagnostic angiograms and roadmaps. An 8-French guiding catheter (Launcher; Medotronic Inc., Minneapolis, MN) was advanced into the right internal jugular vein, and a 0.035” guidewire (Radifocus; Terumo, Tokyo, Japan) over a 4-Fr diagnostic catheter was successfully penetrated through the occluded portion and advanced to the right transverse sinus. Subsequently, the Radifocus wire was replaced with a 0.014” micro guidewire (Chikai; Asahi intecc, Aichi, Japan), which was advanced to the superior sagittal sinus. Balloon angioplasties (Gateway 3 mm × 12 mm; Stryker Neurovascular, Fremont, CA) were repeatedly performed from the distal (closer to the torcula) to the proximal (further from the torcula) portion. A subsequent angiogram showed that antegrade venous flow was restored [
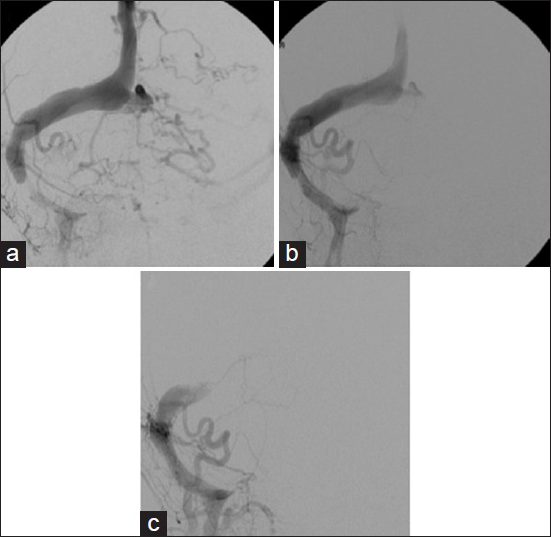
Figure 3
(a) Following preliminary balloon angioplasty, restoration of the antegrade venous flow was observed on a left external carotid angiogram. (b) Subsequent balloon angioplasty with a peripheral balloon catheter achieved a further improvement in the antegrade venous flow; however, the retrograde sinus flow persisted. (c) Next, a self-expanding stent was successfully deployed, and the retrograde venous flow completely disappeared; the Cognard Type IV dural arteriovenous fistula was converted to a Type I
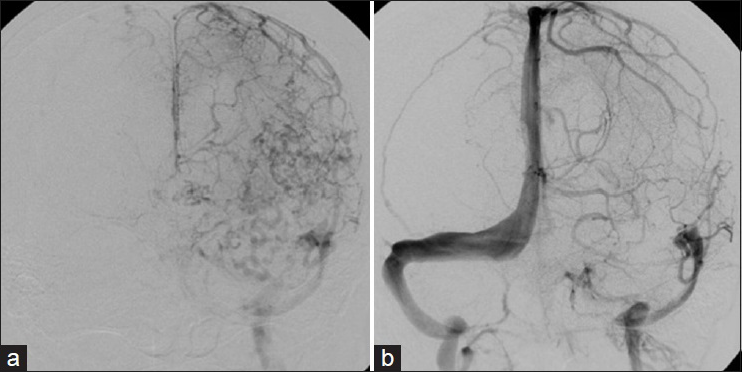
Figure 4
(a) Preoperative left internal carotid angiogram showing severe venous flow impairment. Markedly dilated cortical veins were observed, the cerebral blood flow narrowly returned through either the superficial middle cerebral vein or the vein of Labbe and retrograde venous drainage due to dural arteriovenous fistula was noted. (b) Angiogram obtained 12 months after sinus reconstruction showing a remarkable improvement in the cerebral venous return. The treated right sigmoid sinus was patent
DISCUSSION
Indications for reconstructive therapy
The TVE for TSS DAVFs is a widespread treatment option with high rates of safety and success.[
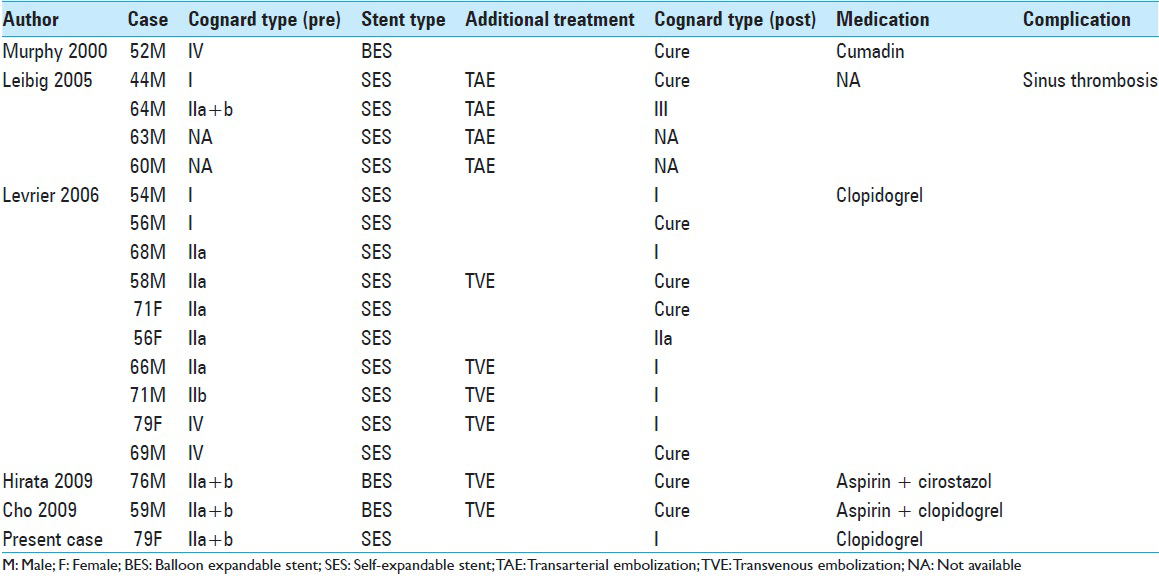
In these reports, almost all cases achieved either a complete cure or transition to a benign status. Liebig et al. reported the adverse events of subsequent occlusion of the stent, which resulted in clinical deterioration.[
Technical aspects of reconstructive therapy
Penetrating a chronically occluded sinus is challenging, even when the occluded segment is short. CT venography is more useful for precisely evaluating the length and configuration of the occluded region and predicting the feasibility of stenting than conventional angiography. In the present case, the angiogram showed opacity in the proximal portion of the occluded sinus. CT venography provided a definitive clue to perform the stenting. After penetrating the occluded sinus, using preliminary balloon angioplasty is recommended. Further navigation of the stent delivery system into stenotic venous sinuses is occasionally difficult because of the stiffness of these divided areas and the acute angle between the internal jugular vein and sigmoid sinus. Therefore, providing adequate support for the guiding system (e.g. using an 8- to 9-Fr guiding catheter) is preferable. To obtain adequate wall apposition and optimal position, the oversized self-expandable stent should be selected and deployed under the roadmap. With respect to the postoperative use of antithrombotic therapy to prevent stent thrombosis, the anticoagulant agent is preferred for peripheral venous stenting.[
CONCLUSION
Although the optimal treatment goal for DAVFs is the complete eradication of fistulae, occluded sinus restoration is preferable in patients with severe cerebral venous congestion due to multiple sinus occlusions and/or a restricted collateral venous outlet. CT venography is useful for precise evaluation of the length and configuration of the occluded segment, which thus make it possible to evaluate the feasibility of stenting.
References
1. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995. 82: 166-79
2. Choi BJ, Lee TH, Kim CW, Choi CH. Reconstructive treatment using a stent graft for a dural arteriovenous fistula of the transverse sinus in the case of hypoplasia of the contralateral venous sinuses: Technical case report. Neurosurgery. 2009. 65: E994-6
3. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995. 194: 671-80
4. Gutierrez A, Do HM, Marks MP. Alteration in the venous drainage of a dural arteriovenous fistula following angioplasty. AJNR Am J Neuroradiol. 2004. 25: 1086-8
5. Halbach VV, Higashida RT, Hieshima GB, Mehringer CM, Hardin CW. Transvenous embolization of dural fistulas involving the transverse and sigmoid sinuses. AJNR Am J Neuroradiol. 1989. 10: 385-92
6. Hirata E, Higashi T, Iwamuro Y, Watanabe Y, Ando M, Arakawa Y. Angioplasty and stent deployment in acute sinus thrombosis following endovascular treatment of dural arteriovenous fistulae. J Clin Neurosci. 2009. 16: 725-7
7. Ihn YK, Kim MJ, Shin YS, Kim BS. Dural arteriovenous fistula involving an isolated sinus treated using transarterial onyx embolization. J Korean Neurosurg Soc. 2012. 52: 480-3
8. Kallmes DF, Jensen ME, Cloft HJ, Kassell NF, Dion JE. Percutaneous transvenous coil embolization of a Djindjian type 4 tentorial dural arteriovenous malformation. AJNR Am J Neuroradiol. 1997. 18: 673-6
9. Kirsch M, Liebig T, Kühne D, Henkes H. Endovascular management of dural arteriovenous fistulas of the transverse and sigmoid sinus in 150 patients. Neuroradiology. 2009. 51: 477-83
10. Levrier O, Métellus P, Fuentes S, Manera L, Dufour H, Donnet A. Use of a self-expanding stent with balloon angioplasty in the treatment of dural arteriovenous fistulas involving the transverse and/or sigmoid sinus: Functional and neuroimaging-based outcome in 10 patients. J Neurosurg. 2006. 104: 254-63
11. Liebig T, Henkes H, Brew S, Miloslavski E, Kirsch M, Kühne D. Reconstructive treatment of dural arteriovenous fistulas of the transverse and sigmoid sinus: Transvenous angioplasty and stent deployment. Neuroradiology. 2005. 47: 543-51
12. McBane RD, Leadley RJ, Baxi SM, Karnicki K, Wysokinski W. Iliac venous stenting: Antithrombotic efficacy of PD0348292, an oral direct Factor Xa inhibitor, compared with antiplatelet agents in pigs. Arterioscler Thromb Vasc Biol. 2008. 28: 413-8
13. Murphy KJ, Gailloud P, Venbrux A, Deramond H, Hanley D, Rigamonti D. Endovascular treatment of a grade IV transverse sinus dural arteriovenous fistula by sinus recanalization, angioplasty, and stent placement: Technical case report. Neurosurgery. 2000. 46: 497-500