- Department of Neurosurgery, Medical Research Institute Kitano Hospital, PIIF Tazuke-Kofukai, Osaka, Japan
- Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan
Correspondence Address:
Hirokuni Hashikata, Department of Neurosurgery, Medical Research Institute Kitano Hospital, PIIF TazukeKofukai, Osaka, Japan.
DOI:10.25259/SNI_547_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hirokuni Hashikata1, Hideki Hayashi1, Wataru Yoshizaki1, Yoshinori Maki2, Hiroki Toda1. Successful treatment of recurrent extracranial hypoglossal schwannoma using the neuroendoscopic transnasal far-medial approach. 09-Aug-2024;15:281
How to cite this URL: Hirokuni Hashikata1, Hideki Hayashi1, Wataru Yoshizaki1, Yoshinori Maki2, Hiroki Toda1. Successful treatment of recurrent extracranial hypoglossal schwannoma using the neuroendoscopic transnasal far-medial approach. 09-Aug-2024;15:281. Available from: https://surgicalneurologyint.com/surgicalint-articles/13029/
Abstract
Background: Extracranial hypoglossal schwannomas are rare, and transcranial skull base surgery can be challenging due to their proximity to the lower cranial nerves, jugular vein, vertebral artery, and carotid artery. The application of neuroendoscopic surgery for extracranial hypoglossal schwannomas has rarely been reported.
Case Description: A 53-year-old woman previously underwent lateral suboccipital surgery for a hypoglossal schwannoma when she was 25 years old. The patient had experienced aggravated dysphagia over the past month. Radiological examination revealed a recurrent extracranial hypoglossal schwannoma invading the left side of the clivus. The neuroendoscopic transnasal far-medial approach was performed, and the recurrent schwannoma was completely removed without any significant perioperative complications or recurrence for 3 years.
Conclusion: Our report highlights the usefulness of the neuroendoscopic transnasal far-medial approach for the removal of recurrent extracranial hypoglossal schwannomas. The neuroendoscopic approach offers a viable and less invasive alternative to traditional transcranial skull-base surgery, especially in complex cases involving critical anatomical structures. The reported case study underscores the potential of neuroendoscopic surgery as a valuable tool in managing challenging skull-base tumors.
Keywords: Extracranial hypoglossal schwannoma, Neuroendoscopic transnasal far-medial approach, Skull-base surgery
INTRODUCTION
Hypoglossal schwannomas are rare, benign tumors that can grow along the tract of the hypoglossal nerve; however, it is quite rare to see their extracranial extension.[
However, transnasal or transoral neuroendoscopic surgery is currently utilized to approach lower clival and petroclival regions safely.[
In this study, we present a case of a recurrent extracranial hypoglossal schwannoma that was successfully treated with neuroendoscopic surgery, highlighting the effectivity of the transnasal far-medial approach.
CASE PRESENTATION
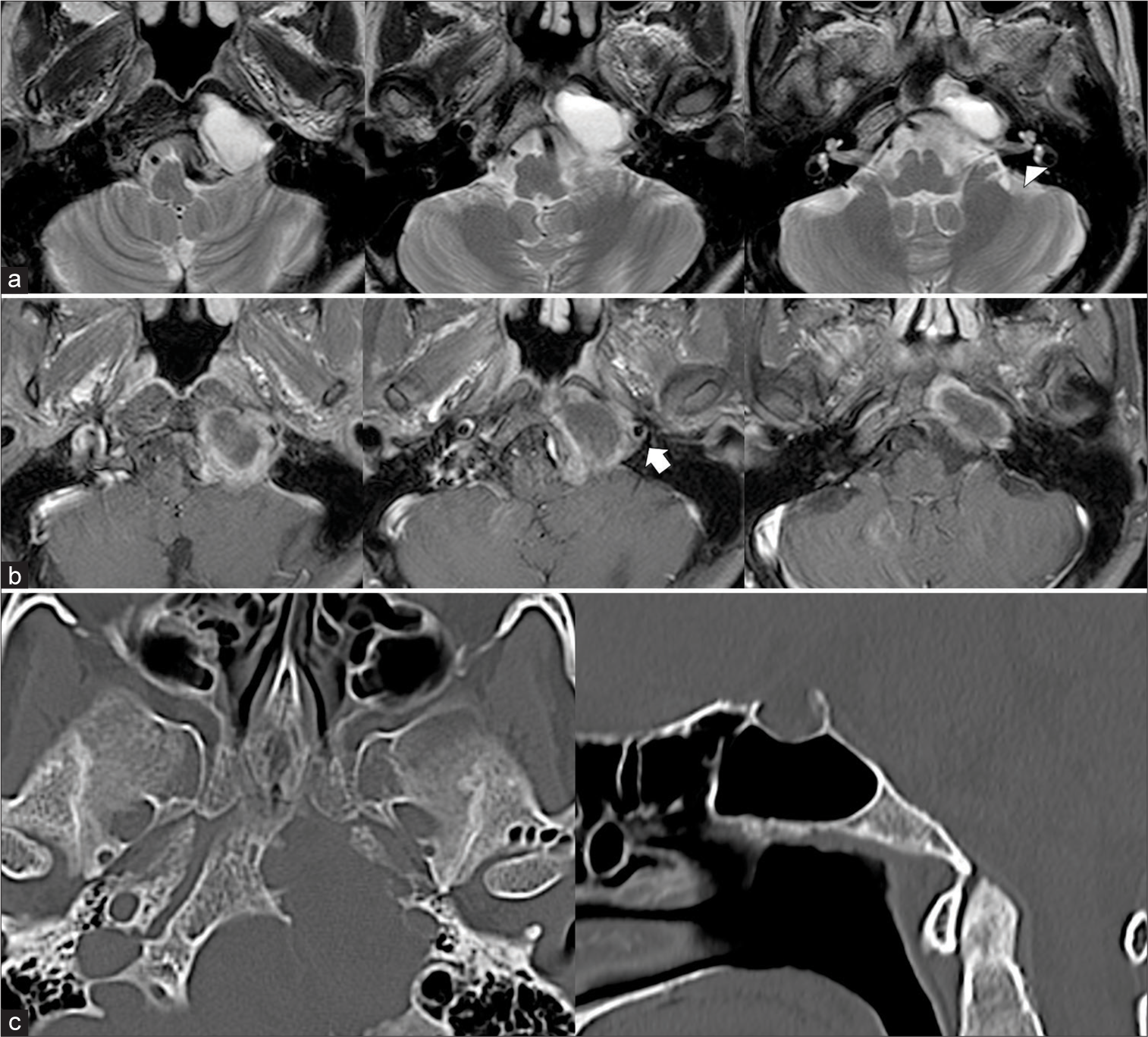
A 53-year-old woman presented with complaints of hoarseness and dysphagia that had been gradually aggravating over the past 3 months. At the age of 25 years, she underwent surgery to remove a left dumbbell-type hypoglossal schwannoma, which resulted in atrophy of the left tongue. Following the initial surgery, she experienced residual tongue atrophy, temporary facial nerve palsy, slight left vocal cord palsy, and dysphagia. Despite these challenges, she remained independent in her daily activities. She continued to attend follow-up appointments at our outpatient clinic until she ceased visiting at the age of 46 years. The patient had experienced aggravated dysphagia in the past month. No significant changes were observed in residual left tongue atrophy, left vocal cord palsy, and soft palate asymmetry. However, a swallowing endoscopy revealed residual saliva in the radix linguae and piriform sinuses. Due to dysphagia, the patient was unable to swallow the general diet. Magnetic resonance imaging revealed a cystic tumor lesion on the left side of the clivus, indicating a residual extracranial hypoglossal schwannoma invading the clivus and compressing the brainstem [
Figure 1:
Preoperative head magnetic resonance (a: T2-weighted images and b: gadolinium-enhanced T1-weighted images) and computed tomography images (c: left, axial images; right, sagittal images). (a and b) The cystic tumor tumoral lesion is located on the left side of the clivus, showing ring enhancement with gadolinium contrast. The lesion extends into the intracranial space, compressing the brain stem and left internal carotid artery (white arrowhead: internal auditory canal, white arrow: internal carotid artery). (c) The tumor has invaded the left side of the clivus.
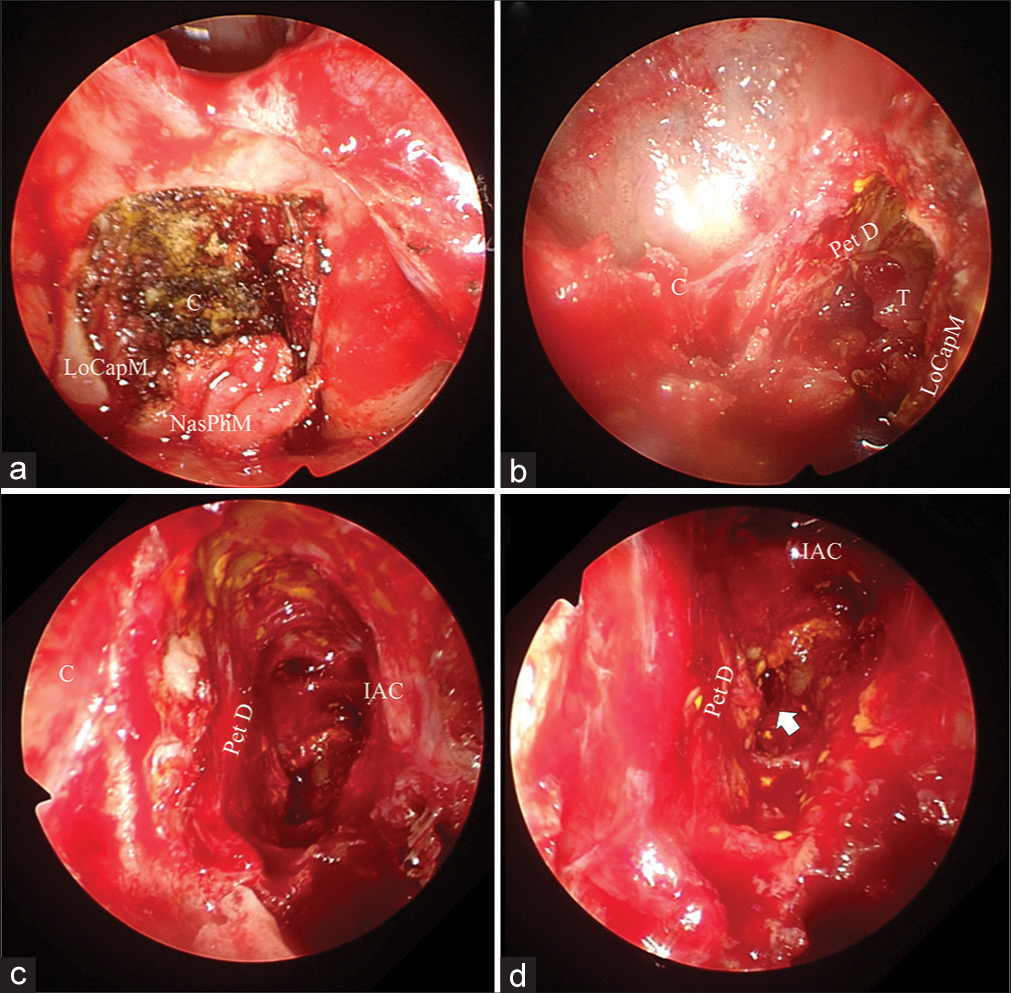
The patient was sedated under general anesthesia and subjected to the neuroendoscopic endonasal far-medial approach to access the tumor lesion. The anterior wall of the sphenoid sinus was approached through the left nasal cavity. The mucosa on the anterior wall of the sphenoid sinus and epipharynx was peeled to expose the sphenoid bone and clivus, avoiding arterial injury guided by intraoperative navigation and Doppler ultrasonography [
Figure 2:
Intraoperative neuroendoscopic findings. (a) The clivus becomes visible after the nasal pharyngeal membrane is detached caudally. (b) The yellowish tumor lesion is identified lateral to the clivus and dorsal to the longus capitis muscle. (c and d) Views using a neuroendoscope angled at 30°. After subtotal resection of the tumor, the dura of the petrous bone and the inner wall of the internal auditory canal are exposed. The tumor invading the hypoglossal canal (white arrow) is also removed. (C: Clivus; IAC: Internal auditory canal; LoCapM: Longus capitis muscle; NasPhM: Nasal pharyngeal membrane; PetD: Dura of the petrous bone; T: Tumor).
Figure 3:
Postoperative head magnetic resonance (a: T2-weighted images and b: gadolinium-enhanced T1-weighted images) and computed tomography images (c: left, axial images; right, sagittal images). (a and b) Cystic and ring-enhanced tumors are completely removed. Brainstem compression by the tumor is also resolved. (c) The access route from the sphenoid sinus to the clivus is observed.
DISCUSSION
Herein, we describe a case of a recurrent hypoglossal nerve schwannoma that was successfully treated using the neuroendoscopic endonasal far-medial approach. The schwannoma was completely resected, and no postoperative complications occurred.
Hypoglossal schwannomas are generally treated with craniotomy; however, this surgical approach has the disadvantages of high mortality and morbidity. With the development of surgical techniques and microanatomical knowledge, safe and effective craniotomies have been performed.[
Neuroendoscopic transoral or transnasal surgery is less invasive for skull-base tumors.[
Neuroendoscopic surgery is less invasive than craniotomies as the internal jugular vein and lower cranial nerves do not have to be exposed; this is one advantage of neuroendoscopic surgery. Unlike previous tumors growing from the midline anatomical structures, such as the clivus or its dura, the neuroendoscopic endonasal far-medial approach can be helpful for treating hypoglossal schwannomas growing from the hypoglossal canal.[
CONCLUSION
We report a case of recurrent hypoglossal schwannoma that was successfully treated using the neuroendoscopic transnasal far-medial approach. As neuroendoscopic surgery is less invasive than craniotomy, recurrent extracranial hypoglossal schwannoma can be approached with this surgical method. However, the usefulness of this method should be evaluated in further similar cases.
Ethical approval
The research/study approved by the Institutional Review Board at Medical Research Institute KITANO HOSPITAL, PIIF Tazuke-kofukai, number P221000400, dated October 17, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ali MS, Algattas H, Zenonos GA, Wang EW, Snyderman CH, Gardner PA. Endoscopic endonasal far-medial approach: 2-dimensional operative video. Oper Neurosurg. 2024. 26: 346
2. Bal J, Bruneau M, Berhouma M, Cornelius JF, Cavallo LM, Daniel RT. Management of non-vestibular schwannomas in adult patients: A systematic review and consensus statement on behalf of the EANS skull base section Part III: Lower cranial nerve schwannomas, jugular foramen (CN IX, X, XI) and hypoglossal schwannoma (XII). Acta Neurochir (Wien). 2022. 164: 299-319
3. Benet A, Prevedello DM, Carrau RL, Rincon-Torroella J, Fernandez-Miranda JC, Prats-Galino A. Comparative analysis of the transcranial “far lateral” and endoscopic endonasal “far medial” approaches: surgical anatomy and clinical illustration. World Neurosurg. 2014. 81: 385-96
4. Bindal S, El Ahmadieh TY, Plitt A, Aoun SG, Neeley OJ, El Tecle NE. Hypoglossal schwannomas: A systematic review of the literature. J Clin Neurosci. 2019. 62: 162-73
5. Derka S, Ebeling M, Pietzka S, Vairaktari G, Stavrianos S, Schramm A. Extracranial hypoglossal schwannoma: Case report and literature review. In Vivo. 2024. 38: 1489-97
6. Emengen A, Yilmaz E, Gökbel A, Uzuner A, Cabuk B, Anik I. Rarely used endoscopic transnasal transdiaphragmatic technique in patients with suprasellar extension: A tertiary Center’s experience with eleven patient cases. World Neurosurg. 2024. 184: e674-81
7. Karadag A, Yuncu ME, Middlebrooks EH, Tanriover N. Endoscopic trans-eustachian tube approach: Identifying the precise landmarks, a novel radiological and anatomical evaluation. Surg Radiol Anat. 2024. 46: 625-34
8. Labib MA, Zhao X, Houlihan LM, Abramov I, Inoue M, Martinez-Perez R. A two-stage combined anterolateral and endoscopic endonasal approach to the petroclival region: An anatomical study and clinical application. Acta Neurochir (Wien). 2022. 164: 1899-910
9. Morera VA, Fernandez-Miranda JC, Prevedello DM, Madhok R, Barges-Coll J, Gardner P. “Far-medial” expanded endonasal approach to the inferior third of the clivus. Oper Neurosurg. 2010. 66: ons211-20
10. Morinaga Y, Akutsu H, Kino H, Tanaka S, Miyamoto H, Matsuda M. Endoscopic endonasal extreme far-medial approach for a lower clivus osteochondroma in a patient with hereditary multiple exostoses: Illustrative case. J Neurosurg Case Lessons. 2021. 1: CASE2153
11. Nonaka Y, Grossi PM, Bulsara KR, Taniguchi RM, Friedman AH, Fukushima T. Microsurgical management of hypoglossal schwannomas over 3 decades: A modified grading scale to guide surgical approach. Neurosurgery. 2011. 69: ons121-40 discussion ons140
12. Silveira-Bertazzo G, Manjila S, London NR, Prevedello DM. Techniques and challenges of the expanded endoscopic endonasal access to the ventrolateral skull base during the “farmedial” and “extreme medial” approaches. Acta Neurochir (Wien). 2020. 162: 597-603
13. Tabari A, Nasirmohtaram S, Mohammadi HR, Zeinalizadeh M, Sadrehosseini SM. Anterior endoscopic sublabial transmaxillary access to middle cranial base lesions. Head Neck. 2024. 46: 1028-42
14. Vargas Gálvez CR, López Arbolay O, Ortiz Machín MM. Minimally invasive approach for skull base meningiomas. Neurocirugia (Engl Ed). 2024. 35: 127-35