- Department of Neurosurgery, Fukuoka Neurosurgical Hospital, Fukuoka, Japan.
- Department of Neurosurgery, Go Neurosurgical Clinic, Fukuoka, Japan.
Correspondence Address:
Shinichiro Yoshida, Department of Neurosurgery, Fukuoka Neurosurgical Hospital, Fukuoka, Japan.
DOI:10.25259/SNI_201_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shinichiro Yoshida1, Kousei Maruyama1, Takuto Kuwajima1, Yoshiaki Hama1, Hiroya Morita1, Yuichiro Ota1, Noriaki Tashiro1, Fumihiro Hiraoka1, Hiroto Kawano1, Shigetoshi Yano1, Hiroshi Aikawa1, Yoshinori Go2, Kiyoshi Kazekawa1. Successful use of an LVIS device to treat unruptured distal aneurysm of the superior cerebellar artery at a vascular bifurcation. 20-May-2022;13:208
How to cite this URL: Shinichiro Yoshida1, Kousei Maruyama1, Takuto Kuwajima1, Yoshiaki Hama1, Hiroya Morita1, Yuichiro Ota1, Noriaki Tashiro1, Fumihiro Hiraoka1, Hiroto Kawano1, Shigetoshi Yano1, Hiroshi Aikawa1, Yoshinori Go2, Kiyoshi Kazekawa1. Successful use of an LVIS device to treat unruptured distal aneurysm of the superior cerebellar artery at a vascular bifurcation. 20-May-2022;13:208. Available from: https://surgicalneurologyint.com/surgicalint-articles/11608/
Abstract
Background: Aneurysms of the distal superior cerebellar artery (SCA) account for only a small proportion of all cerebral aneurysms. Reports of the use of flow diverters (FDs) started to appear in 2013. We obtained good results from placement of a low-profile visualized intraluminal support device (LVIS) to treat unruptured distal aneurysm of the SCA at a vascular bifurcation.
Case Description: A 65-year-old man presented at our hospital with sudden peripheral facial nerve palsy and suspected subarachnoid hemorrhage. Investigational cerebral angiography revealed an aneurysm at the bifurcation of the caudal and rostral trunks of the SCA. An LVIS was placed with the aim of obtaining flow diversion, and cerebral angiography 6 months after this procedure showed disappearance of aneurysm with preservation of the distal SCA.
Conclusion: Twelve cases of the use of FDs to treat aneurysms of the SCA have been reported previously. However, none of those reports described FD use to treat an aneurysm at a vascular bifurcation, as in the present case. Our results suggested that LVIS placement with the aim of obtaining flow diversion may be useful for the treatment of aneurysms at such sites.
Keywords: FRED, Neuroendovascular, Flow-diverter, Aneurysm
INTRODUCTION
Aneurysms of the superior cerebellar artery (SCA) account for only a small proportion of all cerebral aneurysms, and aneurysms of the distal SCA are even more uncommon.[
We inserted a low-profile visualized intraluminal support device (LVIS) (MicroVention, Tustin, CA, USA) with the aim of obtaining flow diversion to treat an unruptured distal aneurysm of the SCA at a vascular bifurcation. Six months later perfusion to the bifurcating vessels was maintained while the aneurysm had been completely obliterated. We, therefore, report this case together with a discussion of the literature.
CASE DESCRIPTION
Patient
A 65-year-old, male.
Chief complaint
Facial nerve palsy.
Case history
The patient noticed a sudden right facial palsy. CT at a local hospital revealed a hyperdense area in the right lateral pons, and the patient was referred to our hospital with suspected SAH.
Examination on admission
Right facial nerve palsy was observed. The patient had no headache, Kernig’s sign, and nuchal rigidity. Lumbar puncture showed that a cerebrospinal pressure of 10 cmH2O and CSF was colorless and clear.
Neuroradiology findings
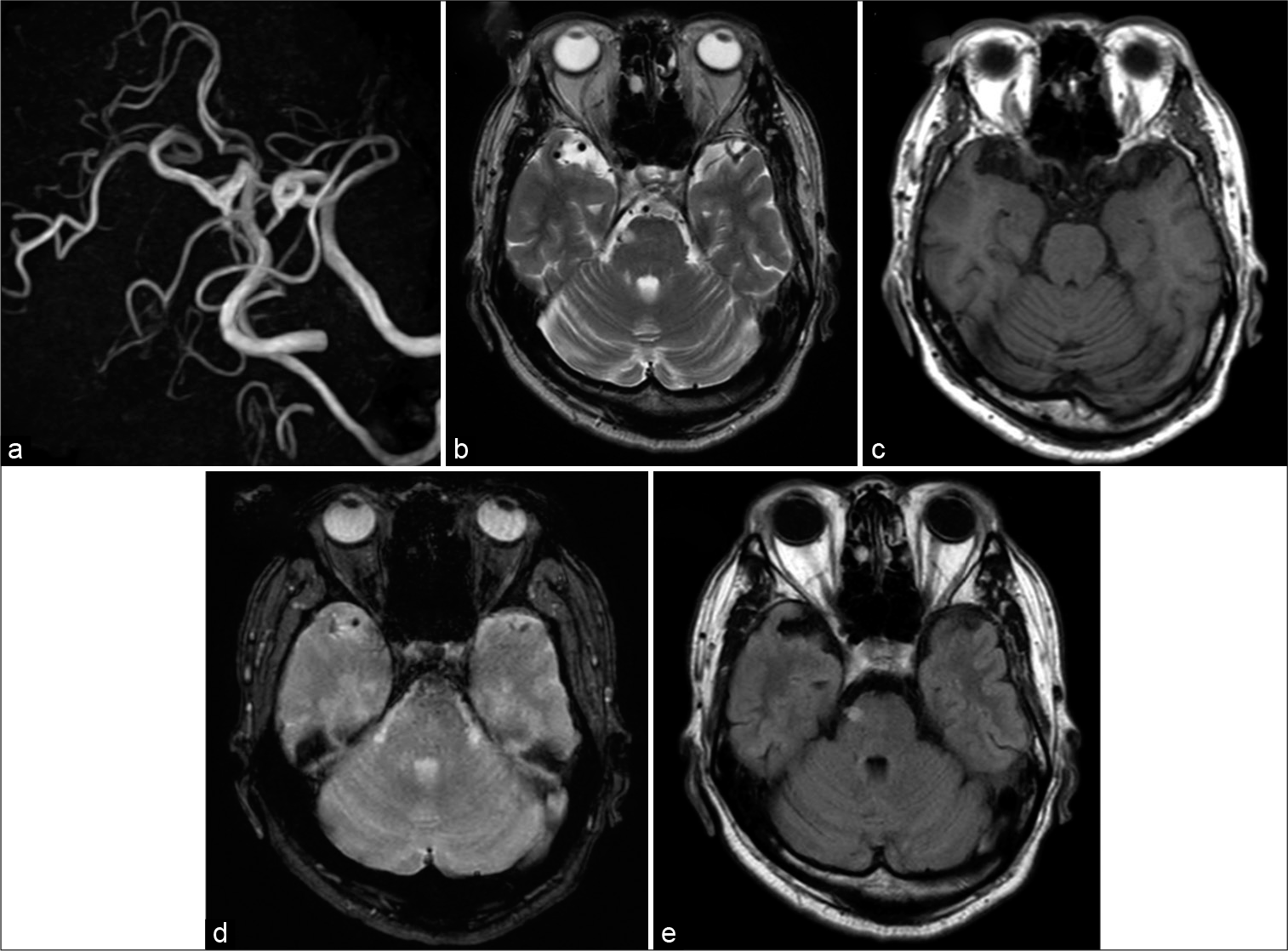
No aneurysm was obviously identifiable on MRI. A spherical, space-occupying lesion appearing hyperintense on T2WI and FLAIR and isointense on T2*WI was observed in the right lateral pons [
Figure 1:
Imaging findings on admission to our hospital. (a) MRA. There are no signs of an aneurysm or other lesion. (b) T2WI. A spherical hyperintensity is evident in the right pons. (c) T1WI. No obvious signs are seen in the right pons. (d) T2*WI. The hyperintensity evident on T2WI is somewhat hyperintense, excluding the possibility of bleeding. (e) FLAIR. A spherical hyperintensity is evident in the right pons.
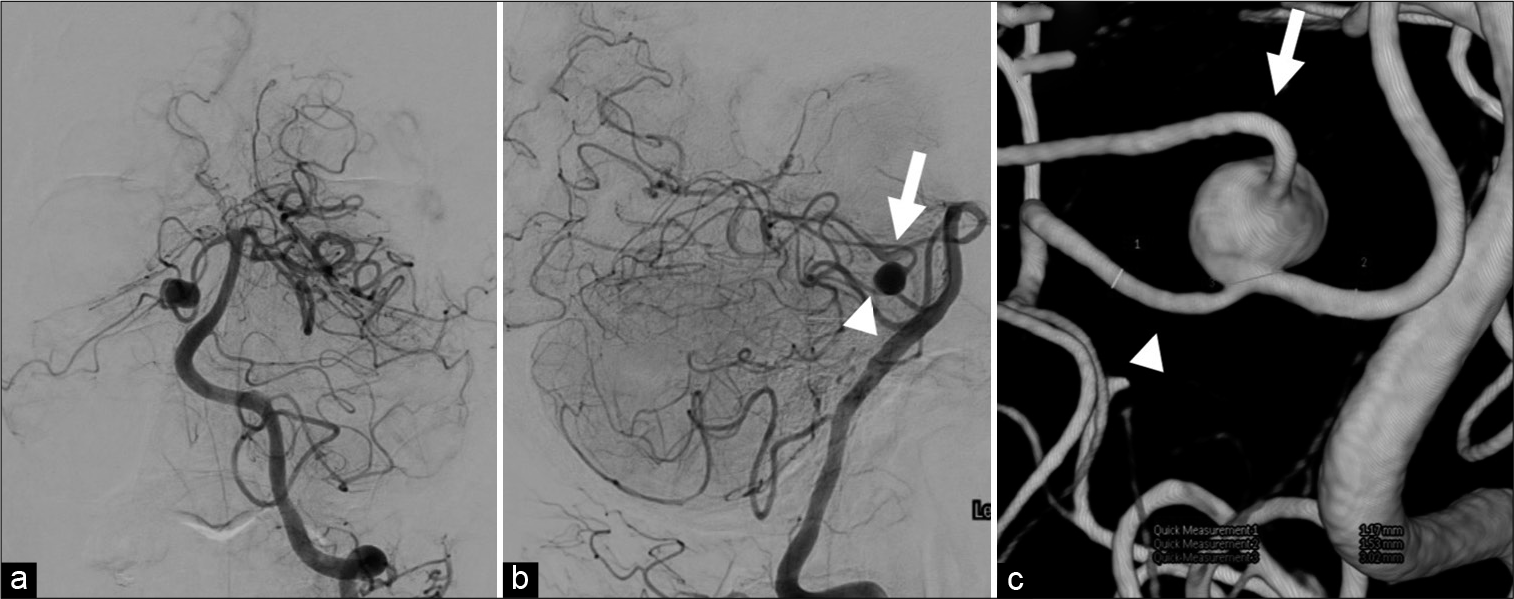
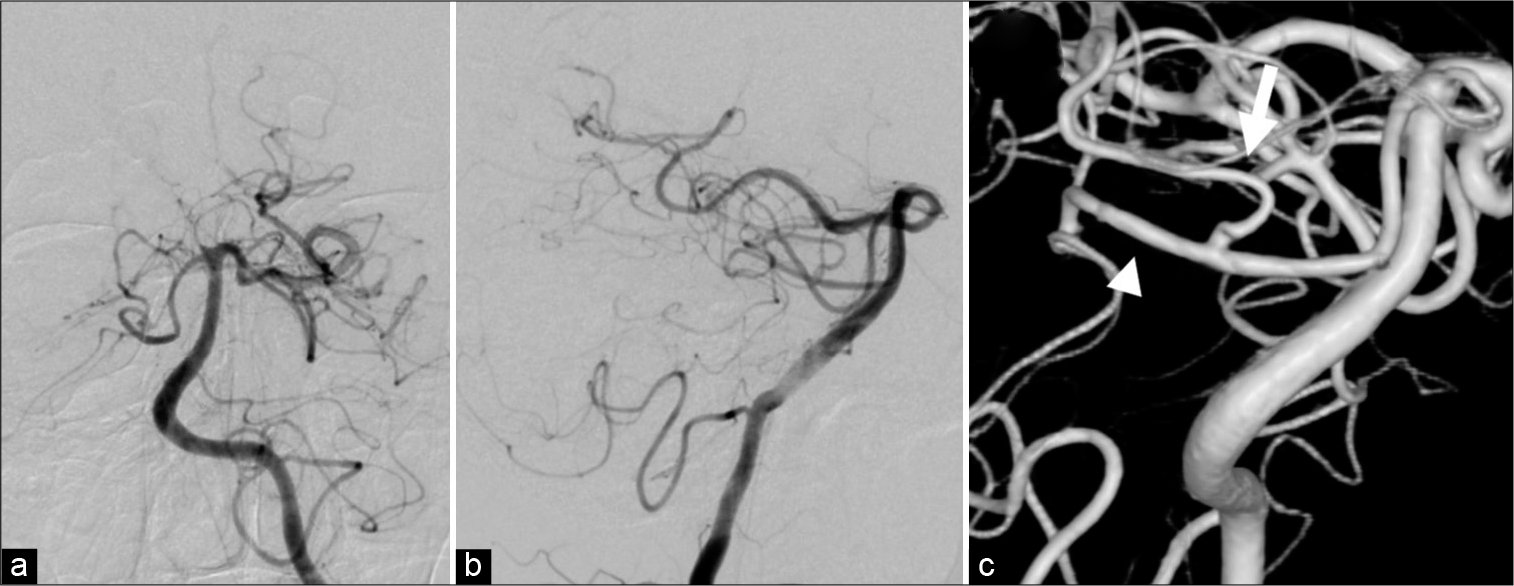
Figure 2:
Imaging before the procedure. (a)DSA Frontal view; (b) DSA lateral view; (c) 3D-RA. The arrows in (b) and (c) indicate the rostral trunk, and the arrowhead in (b) and (c) indicate the caudal trunk. Maximum diameter of the aneurysm is 8.3 mm, diameter of the aneurysm neck is 3 mm, diameter of the vessel distal to the aneurysm is 1.1 mm, and diameter of the vessel proximal to the aneurysm is 1.5 mm.
Treatment strategy
Cranial CT findings were considered indicative of an aneurysm, and lumbar puncture results eliminated the possibility of subarachnoid hemorrhage. Because the maximum aneurysm diameter exceeded 8.3 mm and the patient had suddenly developed peripheral facial nerve palsy, a possible mass effect of the aneurysm could not be ruled out, although this association was unclear, and treatment for an enlarging aneurysm was considered indicated. Occlusion of the parent vessel at a site upstream of the aneurysm or occlusion of the vessels bifurcating from the aneurysm was considered as treatment options. However, given the risk of ischemic complications, the decision was made to place an LVIS with the aim of obtaining flow diversion while sparing both the parent vessel and the vessels bifurcating from the aneurysm.
Ethical considerations
The cerebral endovascular treatment, including the off-label use of LVIS, was approved by the review board at Fukuoka Neurosurgical Hospital, and consent was obtained from the patient after he had been provided with a full explanation of the significance and purpose of the treatment and its risks and complications. Publication of this case report was approved by the hospital review board, and consent was obtained from the patient and his family.
Endovascular treatment
The right femoral artery was punctured and a 6-Fr short sheath was put in place. A 6-Fr Roadmaster (Goodman, Aichi, Japan) was introduced into the V2 portion of the left vertebral artery. A SHOURYU HR 4 mm × 10 mm balloon catheter (Kaneka Medix, Osaka, Japan) was placed in the V3 portion of the left vertebral artery in case of rupture. A Headway 21 (MicroVention/Terumo, Tustin, CA, USA) was inserted, and introduced into the right proximal SCA using a Radifocus guide wire M (GT WIRE) 90° (MicroVention/Terumo). After confirming the aneurysm and the course of the parent vessel, the Headway 21 was introduced into the SCA caudal trunk distal to the aneurysm, which was in the direction of progression of the Headway 21. However, selection of the SCA caudal trunk proved impossible with the GT WIRE 90° because of the curve of microwire tip is very strong, so the aneurysm was secured with a CHIKAI 0.014-inch (Asahi Intecc, Aichi, Japan) with the tip shaped into a double angle, and the Headway 21 was introduced [
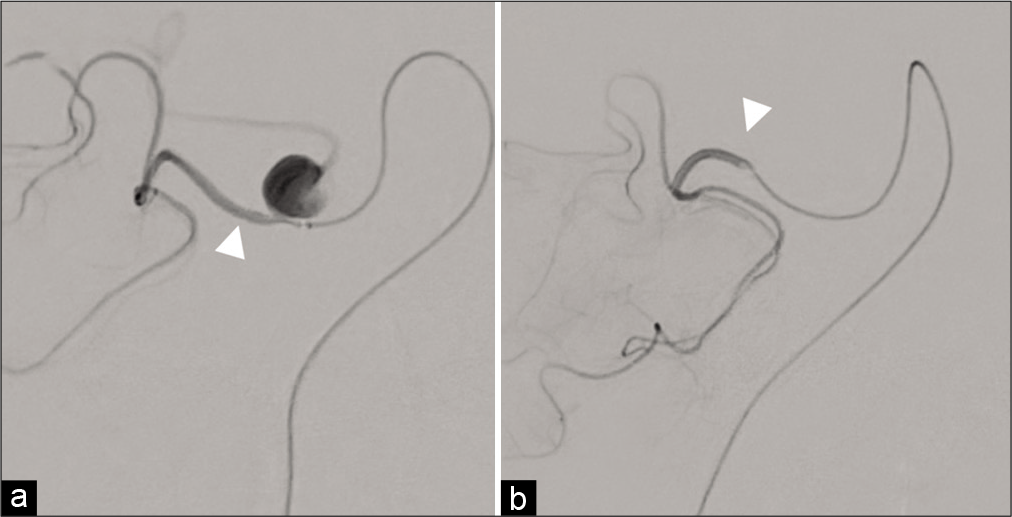
Figure 4:
Postprocedure imaging (a) postprocedure cone-beam CT. A 3.5 × 17-mm low-profile visualized intraluminal support device (LVIS) has been deployed to cover the neck of the aneurysm without cutting off perfusion in the caudal or rostral trunk of the superior cerebellar artery. (b) Postprocedure cerebral angiography. After LVIS placement, an obvious eclipse sign is evident in the aneurysm. Sufficient flow diversion effect was considered likely to be achieved, and the procedure was concluded.
Postprocedure course
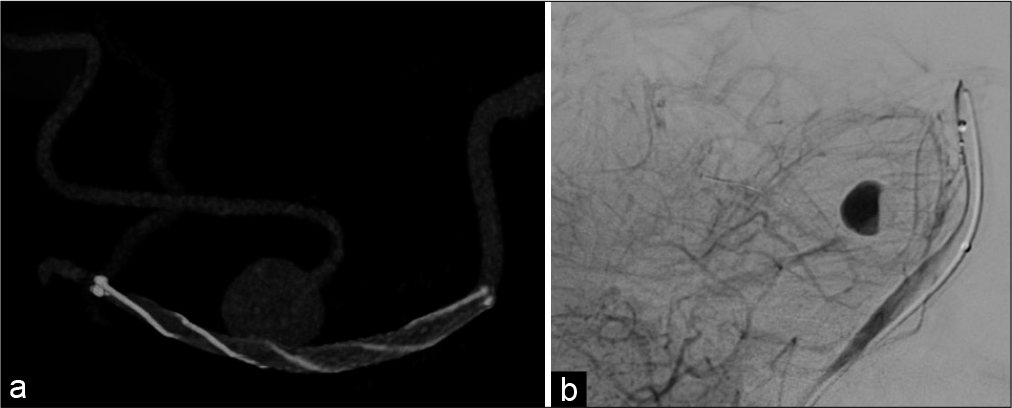
No postprocedure neurological abnormalities were evident, and the patient was, therefore, discharged with a modified Rankin Scale score (mRS) of 0. Cerebral angiography conducted 6 months after the procedure showed that perfusion in the SCA caudal trunk and rostral trunk was preserved while complete obliteration of the O’Kelly-Marotta grading scale (OKM) grade D aneurysm was observed [
Figure 5:
Imaging at 6 months postprocedure. (a) DSA Frontal view; (b) DSA lateral view; (c) 3D-RA. The aneurysm is completely obliterated, and assessed as O’Kelly-Marotta grading scale Grade D. Perfusion in the rostral trunk (arrow) and caudal trunk (arrowhead) of the superior cerebellar artery bifurcating from the aneurysm is preserved.
DISCUSSION
Aneurysms located on the SCA account for only 1.7% of all cerebral aneurysms, and aneurysms of the distal SCA are even more uncommon, at 0.2%.[
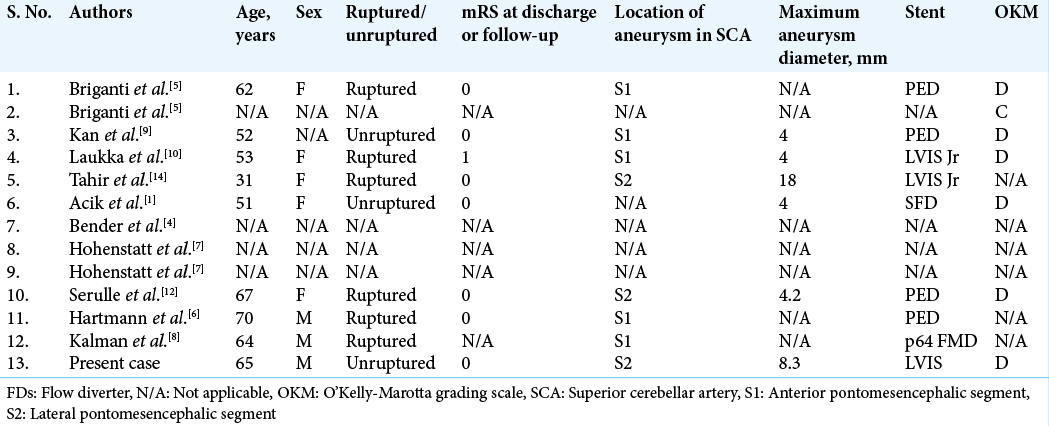
Since 2013, scattered reports have described treatment with the aim of obtaining a flow-diverting effect, as in the present case. To the best of our knowledge, 12 such cases have been reported [
We considered the combined occlusion of the aneurysm parent vessel and the bifurcating vessels in the present case, but were wary of the risk of ischemic complications due to vascular occlusion. In fact, a case in which open decompression was conducted after SCA occlusion treatment has been reported,[
In our patient, the SCA caudal trunk, as the vessel distal to the aneurysm, was chosen as the parent vessel for LVIS placement because it ran in the same direction as the direction of advancement of microcatheter. The SCA rostral trunk coursed at right angles to the direction of advancement of microcatheter, and was therefore not chosen as the parent vessel because introduction of microcatheter was considered too difficult to introduce. Because microcatheter manipulation in distal vessels is difficult, selecting a vessel into which they can be introduced as easily as possible may contribute to the success of treatment.
In our patient, we used an LVIS with the aim of obtaining a flow-diverting effect. However, it must be remembered that although Chao has described the flow-diverting effects of LVIS devices,[
In the present case, we used the eclipse sign in the aneurysm as a sign to conclude the procedure. The presence of layered stagnation of the contrast agent in the aneurysm, known as the “eclipse sign,” following FDs placement is said to be more common in aneurysm patients with a high postprocedure obliteration rate.[
CONCLUSION
Our results suggested that LVIS placement with the aim of obtaining flow diversion in the treatment of unruptured distal SCA aneurysms with a vascular bifurcation may provide good flow-diverting effects without causing divided vessel occlusion, and may achieve complete aneurysm obliteration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Acik V, Daglioglu E, Akmangit I, Alagoz F, Sayin B, Arat A. Endovascular treatment of superior cerebellar artery aneurysms. Turk Neurosurg. 2019. 29: 564-9
2. Alurkar A, Karanam LS, Nayak S, Oak S. Endovascular management of fusiform superior cerebellar artery aneurysms: A series of three cases with review of literature. J Clin Imaging Sci. 2012. 2: 47
3. Anil G, Sein L, Nga V, Teo K, Chou N, Yeo TT. Dissecting distal cerebellar artery aneurysms: options beyond a parent vessel sacrifice. Neurosurg Rev. 2020. 43: 771-80
4. Bender MT, Colby GP, Jiang B, Lin LM, Campos JK, Xu R. Flow diversion of posterior circulation cerebral aneurysms: A single-institution series of 59 cases. Neurosurgery. 2019. 84: 206-16
5. Briganti F, Leone G, Cirillo L, de Divitiis O, Solari D, Cappabianca P. Postprocedural, midterm, and long-term results of cerebral aneurysms treated with flow-diverter devices: 7-year experience at a single center. Neurosurg Focus. 2017. 42: E3
6. Hartmann A, Hoffmann KT, Sander C, Quaeschling U, Schob S.editors. Superior cerebellar artery aneurysm: Spontaneous subarachnoid hemorrhage and stent-assisted coil occlusion of a ruptured aneurysm at the superior cerebellar artery origin and of an unruptured small basilar artery bifurcation aneurysm, bacterial endocarditis, early major aneurysm recurrence with oculomotor palsy, and treatment of the “mycotic” aneurysm by flow diverter implantation, with resolution of the aneurysm and good clinical recovery. The Aneurysm Casebook. Switzerland: Springer; 2020. p. 1523-1532
7. Hohenstatt S, Arrichiello A, Conte G, Craparo G, Caranci F, Angileri A. Branch vessel occlusion in aneurysm treatment with flow diverter stent. Acta Biomed. 2020. 91: e2020003
8. Kalman M, AlMatter M, Perez MA, Niehaus L, Henkes H.editors. Superior cerebellar artery aneurysm: Spontaneous SAH, occlusion of a mid-sized, wide-necked superior cerebellar artery aneurysm with a medina device and coils; subsequent coil compaction, treated with flow diversion using a p64. The Aneurysm Casebook. Switzerland: Springer; 2020. p. 1513-22
9. Kan P, Srinivasan VM, Mbabuike N, Tawk RG, Ban VS, Welch BG. Aneurysms with persistent patency after treatment with the pipeline embolization device. J Neurosurg. 2017. 126: 1894-8
10. Laukka D, Rautio R, Rahi M, Rinne J. Acute treatment of ruptured fusiform posterior circulation posterior cerebral, superior cerebellar, and posterior inferior cerebellar artery aneurysms with FRED flow diverter: Report of 5 cases. Oper Neurosurg (Hagerstown). 2019. 16: 549-56
11. Möhlenbruch MA, Herweh C, Jestaedt L, Stampfl S, Schönenberger S, Ringleb PA. The FRED flow-diverter stent for intracranial aneurysms: Clinical study to assess safety and efficacy. AJNR Am J Neuroradiol. 2015. 36: 1155-61
12. Serulle Y, Khatri D, Fletcher J, Pappas A, Heidbreder A, Langer D. Fusiform superior cerebellar artery aneurysm treated with flow diversion: A case report. Surg Neurol Int. 2020. 11: 330
13. Shigeru M, Hiroyuki O, Ryo H, Ryoukichi Y, Toshihikio K. Flow diverter for large carotid cavernous aneurysms. Surg Cereb Stroke (Jpn). 2018. 46: 50-7
14. Tahir R, Asmaro KP, Haider S, Kole M. Ruptured distal superior cerebellar artery dissecting aneurysm treated with a flow-diverting device: Case report and review of literature. Cureus. 2018. 10: e2918
15. Wang C, Tian Z, Liu J, Jing L, Paliwal N, Wang S. Flow diverter effect of LVIS stent on cerebral aneurysm hemodynamics: A comparison with Enterprise stents and the Pipeline device. J Transl Med. 2016. 14: 199