- Department of Neurosurgery, University of the Witwatersrand, Medical School, Johannesburg, South Africa.
- Department of Neurosurgery, Helen Joseph Hospital, Johannesburg, South Africa.
Correspondence Address:
Blessing Ndlovu, Department of Neurosurgery, University of the Witwatersrand, Medical School, Johannesburg, South Africa.
DOI:10.25259/SNI_810_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Blessing Ndlovu1, Mohammed Ouwais Abdul Sattar2, Mlamuli Mzamo Mkhaliphi2, Keletso Leola1, Morena Nthuse Mpanza2, John Richard Ouma1, Christos Profyris2. Supraorbital eyebrow approach: A single-center experience. 02-Dec-2022;13:566
How to cite this URL: Blessing Ndlovu1, Mohammed Ouwais Abdul Sattar2, Mlamuli Mzamo Mkhaliphi2, Keletso Leola1, Morena Nthuse Mpanza2, John Richard Ouma1, Christos Profyris2. Supraorbital eyebrow approach: A single-center experience. 02-Dec-2022;13:566. Available from: https://surgicalneurologyint.com/surgicalint-articles/12035/
Abstract
Background: Keyhole neurosurgery is the notion of safely removing brain and skull base lesions through smaller and more precise openings that lessen collateral damage to the surrounding scalp, brain, blood vessels, and nerves. The traditional frontal and pterional approaches require large craniotomies and this predisposes patients to significant and avoidable morbidity. With the growing expectation for minimally invasive surgery, we present our experience with the supraorbital keyhole craniotomy for surgical lesions in the anterior cranial fossa and parasellar regions.
Methods: We retrospectively analyzed and evaluated all cases of neoplastic, vascular, trauma, and infective pathologies of the anterior fossa and parasellar regions treated using a keyhole approach, the supraorbital eyebrow (SOE) approach from January 2018 to June 2022. Treatment outcomes were evaluated based on pathology.
Results: A total of 50 patients underwent a SOE craniotomy during the study period (28 females and 22 males). Their average age ranged from 12 to 86 years, with a mean age of 47.4 years. All patients had anterior skull base and/or anterior frontal lobe pathologies: (23 tumors, 17 ruptured aneurysms, five traumatic frontal hematomas, three extradural empyema, one cerebral cavernous malformation, and one traumatic frontal skull base fracture with dural tear and CSF leak). Gross total tumor resection was achieved in 87% of cases (13 meningiomas of which six were giant, three gliomas, two craniopharyngiomas, and two cerebral metastases). Clip ligation occlusion rate for our aneurysm cases was 100% and intraoperative rerupture was observed in three cases. Mean ICU stay was 2.2 days for the entire series. The overall 30-day mortality rate for our series was 16% (eight deaths). This was highest in the ruptured aneurysm subgroup, with all 5 mortality cases in the aneurysmal subgroup presenting as World Federation of Neurological Surgeons (WFNS) grades ≥ III. 4 of the deaths were in WFNS IV and V patients. The most frequent perioperative complication was transient periorbital swelling which resolved within 7 days. It was observed in 18 of the 50 patients. The next common complications in descending frequency were eyebrow alopecia (three cases), supraorbital hypoesthesia (two cases), CSF leak (two cases), and surgical site infection (one case). There was one approach-related intraoperative complication secondary to carotid injury in a giant meningioma redo case. Conversion to a larger craniotomy was never necessary. Clinical outcome for our cases was evaluated according to the Modified Rankin Scale (mRS) at 3-month postsurgery. A good clinical outcome (mRS ≤ 2) was achieved for 78% of our patients.
Conclusion: The SOE approach craniotomy is an effective minimally invasive approach for various pathologies of the anterior cranial base and parasellar regions. With experience, giant tumors and complex vascular pathology can be addressed with this keyhole approach.
Keywords: Aneurysm, Brain tumor, Empyema, Eyebrow, Supraorbital
INTRODUCTION
Over the past half century, improvements in microsurgical techniques, refinement of microinstruments, and advanced preoperative diagnostic imaging together with accumulation of microsurgery experience have enabled the evolution of microneurosurgical techniques and a reduction of surgery-related trauma. These progressive developments have made it possible for neurosurgeons to treat more complicated lesions through smaller craniotomies.[
Keyhole neurosurgery is a relatively new and minimally invasive concept of microsurgery based on tailored, targeted, and direct techniques.[
The supraorbital eyebrow (SOE) approach is a minimally invasive keyhole technique that may be utilized to access surgical lesions located at the anterior skull base and within the parasellar region. It is a less invasive alternative to the traditional pterional, orbitozygomatic, or bifrontal approaches. Using a small eyebrow incision and a strategically placed craniotomy that is flush with the orbital roof, the supraorbital approach offers a direct subfrontal surgical trajectory to anteriorly located skull base tumors and anterior circulation vascular lesions. The approach adheres to the keyhole principle, whereby a small well-placed craniotomy allows wide access to deeper surgical lesions without the need for fixed brain retraction.[
This paper evaluates the indications, techniques, advantages, and limitations of the supraorbital keyhole approach through an eyebrow skin incision as a minimally invasive approach through a retrospective analysis of our own experience as a neurosurgical unit in a resource-limited setting.
MATERIALS AND METHODS
We retrospectively reviewed all cases of neoplastic, vascular, infective, and trauma pathologies of the anterior fossa and parasellar region treated using the SOE approach from January 2018 to June 2022. All inpatient and outpatient records were reviewed and clinical/operative outcomes and complications were analyzed. For tumor patients, we evaluated tumor diagnosis based on histopathology reports and we evaluated extent of resection based on pre- and postoperative magnetic resonance imaging (MRI). Resection rates for tumors were considered as follows: gross-total resection (GTR), when no residual tumor was visible on postoperative MRI; near-total resection (NTR), when >90% of the lesion was resected; and subtotal resection (STR), when <90% of tumor was removed. For patients with ruptured aneurysms, we evaluated clinical presentation and aneurysm site. Aneurysm occlusion rate was evaluated based on pre- and post-operative computed tomography angiography (CTA) imaging.
Surgical technique
Patients were positioned in a three-pin head holder with the head positioned such that the malar eminence was the highest point in positioning the head. The head was then rotated about 10°–60° to the contralateral side, with the degree of rotation dependent on the precise location of the pathological lesion of interest. A 4–5 cm skin incision was made over the superior orbital rim at the upper limit of the eyebrow [
Figure 1:
Representative case illustrating the surgical technique of the supraorbital eyebrow approach. (a) Proper positioning including head extension and rotation, with the line marking the skin incision made over the superior orbital rim at the upper limit of the eyebrow. (b) Mini-supraorbital craniotomy. (c) Flattening of the orbital roof. (d) Curvilinear durotomy. (e) Dynamic frontal lobe retraction using suction tips, bipolar forceps, and cottonoids to reach and open CSF cisterns to facilitate brain relaxation. (f) Watertight dural closure. (g) Bone flap fixation using low profile titanium plates ensuring that the bone flap is flash with the superior frontal bone edge. (h) Subcuticular 4/0 Prolene suture without knots is used to approximate the skin edges. (i) Nonadherent Telfa dressing is used to cover the wound.
Illustrative cases
Case 1
A 49-year-old female presented with psychosis preceded by many years of progressive headache and personality changes including abulia for which she did not seek medical attention.
Neurologically, she was disoriented however without motor or ophthalmological deficits.
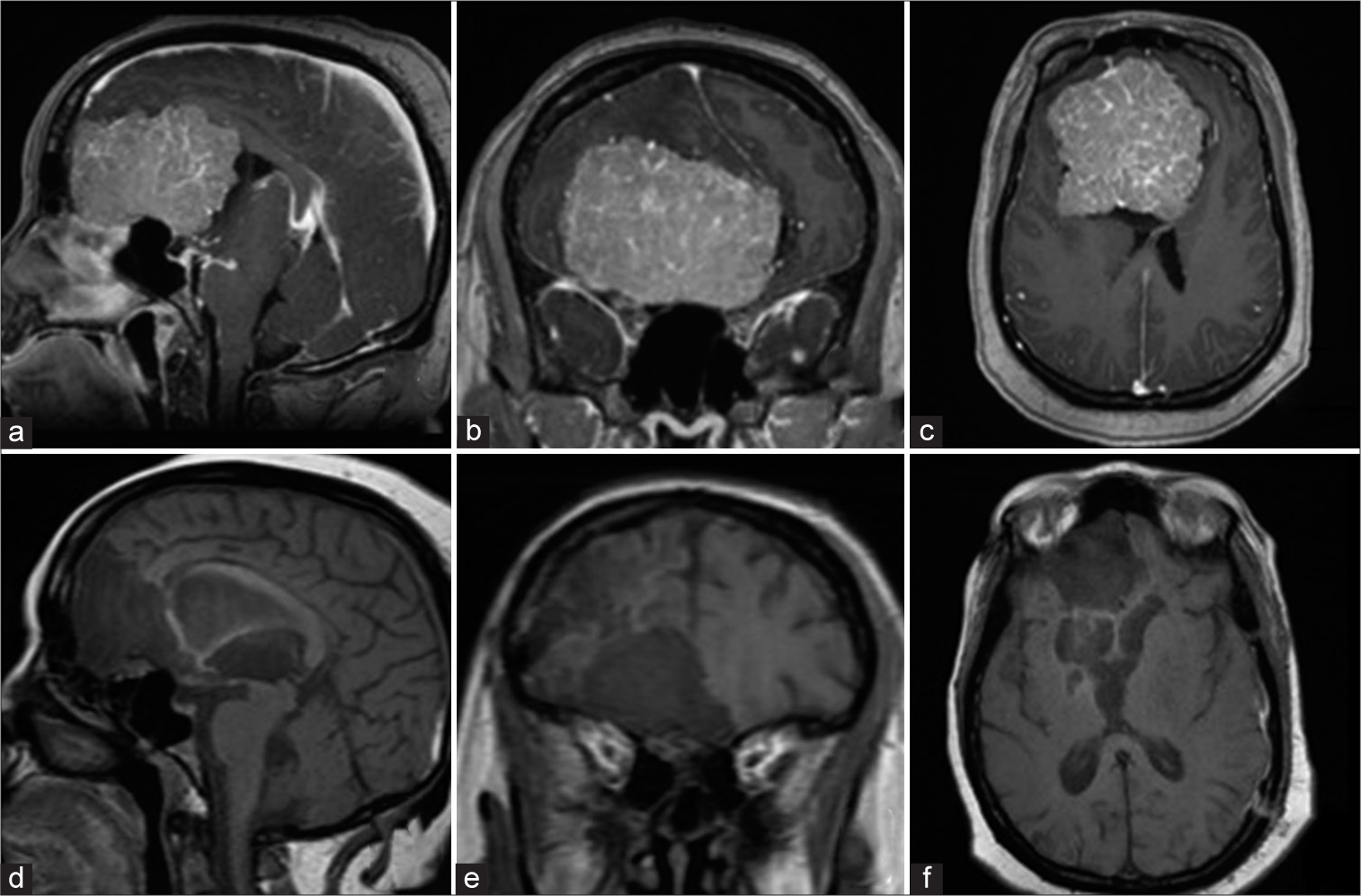
MRI of the brain revealed a large extra-axial homogenously enhancing anterior cranial fossa mass consistent with an olfactory groove meningioma [
Figure 2:
Preoperative postgadolinium-enhanced T1 magnetic resonance imaging (MRI) images (a) sagittal, (b) coronal, and (c) axial views showing a giant olfactory groove meningioma spanning the entire anterior skull base from the posterior table of the frontal sinus to the suprasellar region with significant mass effect on the midbrain, lateral, and third ventricles. Postoperative T1 MRI images (d) sagittal, (e) coronal, and (f) axial views depicted gross-total resection of the meningioma with resolution of the mass effect on the brainstem and ventricles.
The patient underwent operative resection of her tumor through a right SOE craniotomy.
She had gross-total resection of a WHO Grade I meningothelial meningioma with no neurological deficits postoperatively and complete resolution of her frontal lobe symptoms [
Case 2
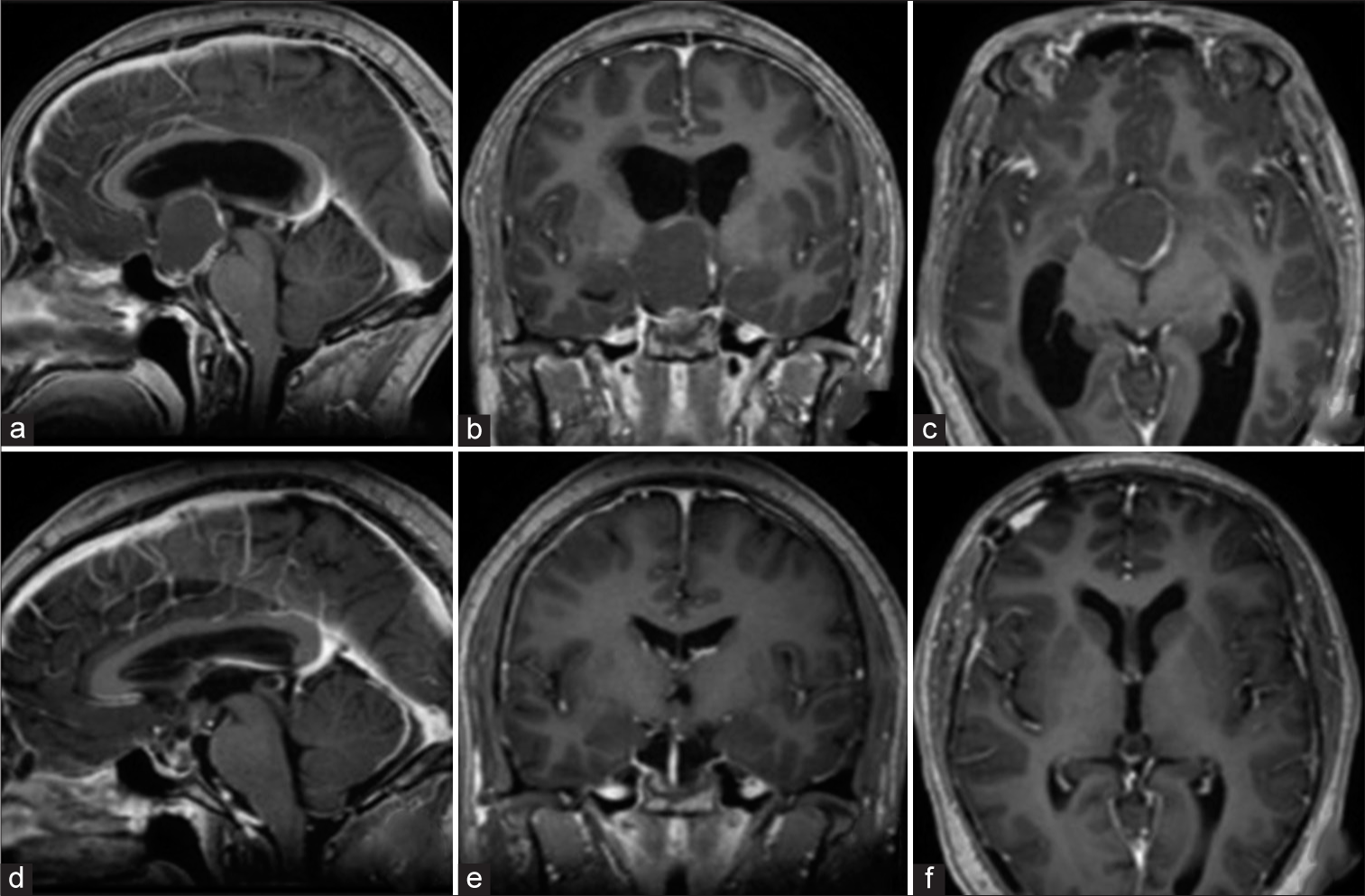
A 19-year-old male university student presented with a 4-month history of headache, intermittent blurred vision, and deterioration of school performance due to inability to concentrate.
On clinical examination, there were no motor deficits. Fundoscopy revealed mild papilledema.
MRI of the brain demonstrated a solid cystic sellarsuprasellar mass with mass effect on the third ventricle causing obstructive hydrocephalus. Imaging characteristics were consistent with a craniopharyngioma [
Figure 3:
Preoperative postgadolinium-enhanced T1 magnetic resonance imaging (MRI) images (a) sagittal, (b) coronal, and (c) axial views depicting a solid cystic sellar-suprasellar mass with mass effect on the third ventricle causing obstructive hydrocephalus, consistent with a craniopharyngioma. Postoperative postgadolinium-enhanced T1 MRI images (d) sagittal, (e) coronal, and (f) axial views showed gross-total removal of the lesion with resolution of the hydrocephalus.
The patient underwent a right SOE craniotomy and gross-total resection was achieved [
Case 3
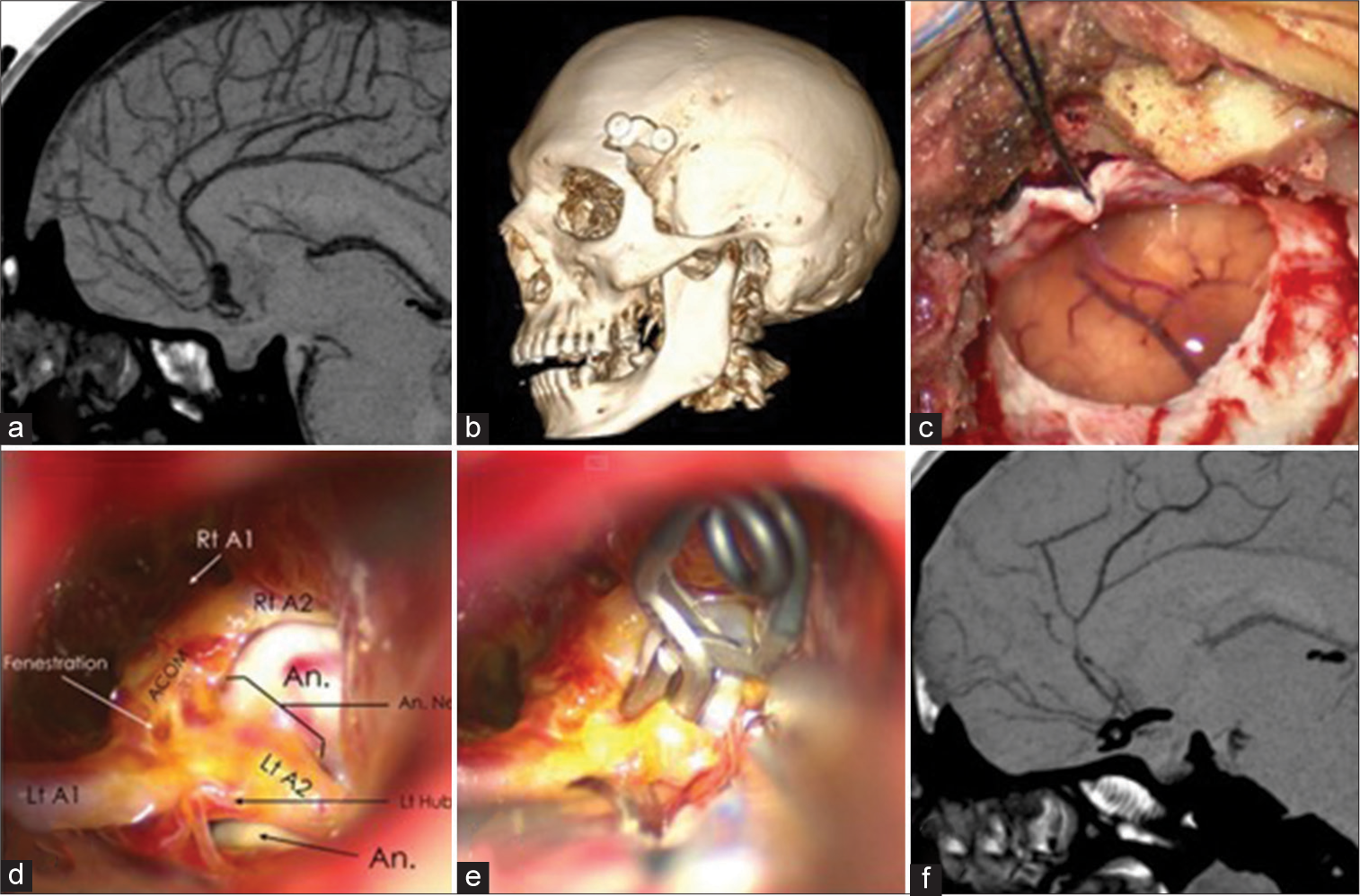
A 42-year-old male presented with a sudden occipital headache with associated neck stiffness, photophobia, and confusion.
On admission, he had a GCS of 14/15 with nuchal rigidity but no motor deficits.
Computed tomography (CT) scan of the brain showed thick subarachnoid hemorrhage (SAH) in the subfrontal region. Subsequent CTA confirmed a ruptured anterior communicating artery (AComA) aneurysm [
Figure 4:
Preoperative sagittal computed tomography angiography (CTA) imaging showing an anterior communicating artery aneurysm (a). Intraoperative microscopic images confirming subarachnoid hemorrhage (c) and microsurgical exposure of the aneurysm and the surrounding vascular anatomy (d). Successful clip ligation of the aneurysm illustrated intraoperatively (e) and confirmed on CTA imaging on the 1st postoperative day (f). Postoperative 3D reconstruction of the skull depicting the size of the keyhole craniotomy (b).
The aneurysm was clip ligated successfully through right SOE craniotomy with no intraoperative complications [
Case 4
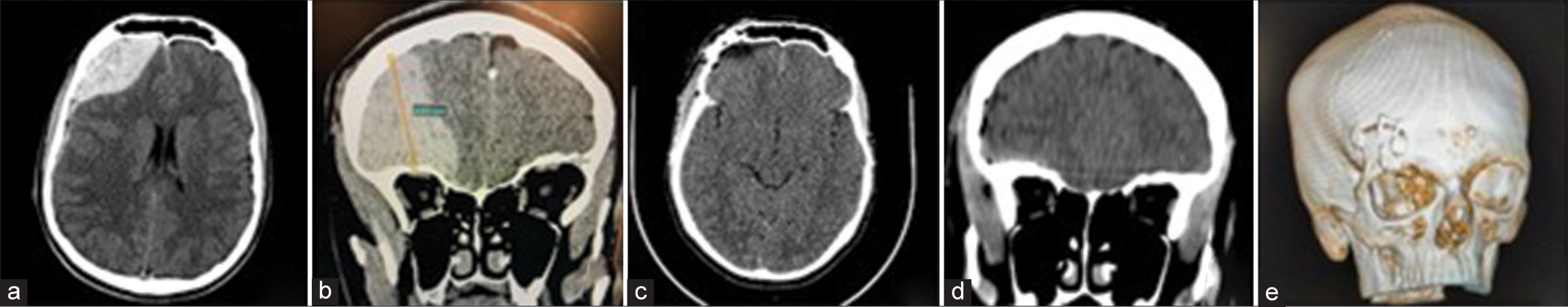
A 16-year-old male presented with headache and vomiting following a fall from a bicycle.
On admission, he was fully conscious with no focal neurological deficits. CT scan of the brain showed an acute right-sided frontal extradural hematoma with significant mass effect [
He underwent a right-sided SOE craniotomy with successful clot evacuation and relief of mass effect.
Figure 5:
Axial (a) and coronal (b) computed tomography (CT) images showing a right frontal acute extradural hematoma with significant frontal lobe compression and contralateral midline shift which was successfully treated through the supraorbital eyebrow approach with complete clot evacuation and relief of the mass effect as shown on the postoperative axial (c), coronal (d), and 3D skull reconstruction (e) CT images. (b) Height of hematoma (yellow line), measuring 4.61cm (shown in blue).
Postoperatively, his symptoms resolved completely, with radiological evidence of total extradural hematoma evacuation [
RESULTS
Series demographic and clinical characteristics
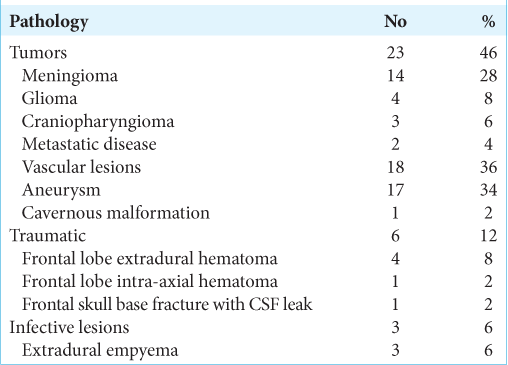
Our case series included 50 patients: 28 females and 22 males. Their average age ranged from 12 to 86 years, with a mean age of 47.4 years. All patients had anterior skull base and/or anterior frontal lobe pathologies (23 tumors, 17 ruptured aneurysms, five traumatic frontal hematomas, three extradural empyema, one cerebral cavernous malformation, and one traumatic anterior fossa dural tear and CSF leak) [
Series neoplasms
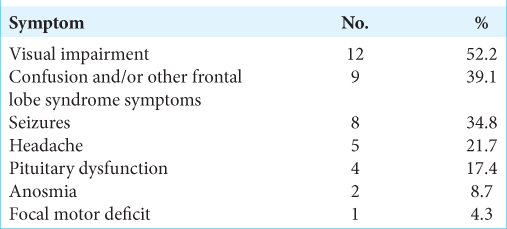
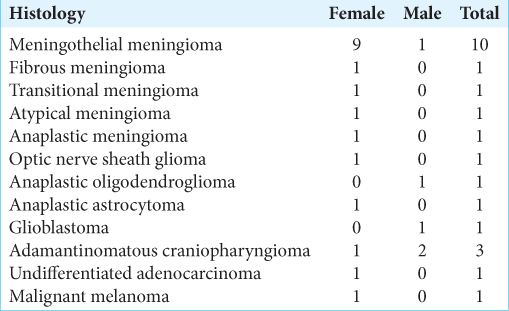
Neoplasms comprised the bulk of the lesions in our series (23 cases), of which meningiomas were the most common tumors (14 cases), followed by gliomas (four cases), craniopharyngiomas (three cases), and cerebral metastases (two cases). Six of the 14 meningiomas were giant meningiomas – with a diameter ≥6 cm.
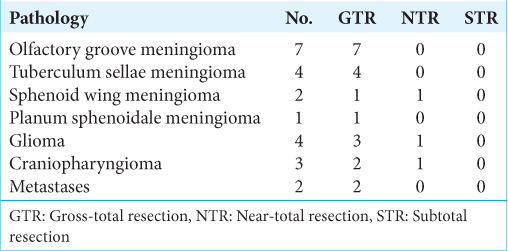
The presenting symptoms in patients with tumors in our case series were related to mass effect on structures around the anterior cranial fossa and/or the frontal lobe [
Visual impairment was the most frequent presenting complaint (52.2%) followed by frontal lobe symptoms (39.1%) and seizures (34.8%). Other common presenting symptoms were headache, anosmia, and pituitary dysfunction. Only one patient presented with a focal motor deficit (hemiplegia) [
The histopathological diagnoses for the presented tumor series are presented in
Gross-total tumor resection was achieved in 20 of the 23 cases (13 meningiomas, three gliomas, two craniopharyngiomas, and two cerebral metastases). The remaining three cases were a NTR due to adherence to critical neurovascular structures [
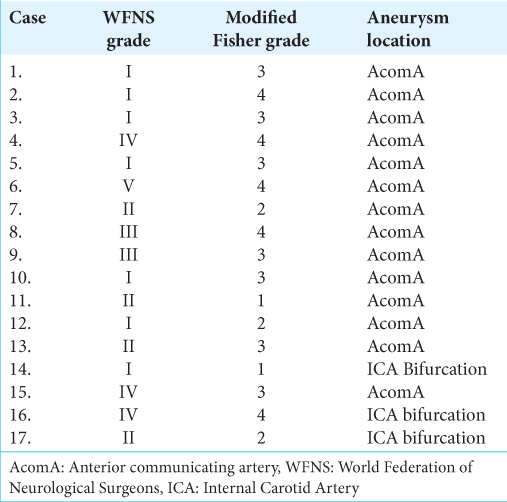
Series vascular lesions
Aneurysms were the next most common pathological entity operated on through a SOE approach (17 cases). All aneurysms in the current series were of the anterior circulation: AComA (14 cases) and the internal carotid artery bifurcation (three cases). All aneurysms treated had presented with acute SAH. The cohort comprised of eight males and nine females. The age of patients ranged from 35 to 71 years with a mean age of 50.2 years.
According to the Modified Fisher’s grade of SAH on head CT before the operation, the cohort comprised two cases of Grade 1 (11.8%), three cases of Grade 2 (17.6%), seven cases of Grade 3 (41.2%), and five cases of Grade 4 (29.4%) [
A total of seven patients were WFNS I (41.2%), four were WFNS II (23.5%), two were WFNS III (11.8%), three were WFNS IV (17.6%), and one was WFNS V (5.9%) [
Intraoperative aneurysm rupture during surgical clipping was observed in 3 cases (17.6%). The clip ligation occlusion rate for our aneurysm cases determined by CTA on the 1st postoperative day was 100%. None of the patients undergoing aneurysm clip ligation through the SOE approach required conversion to a pterional microsurgical approach.
We had a single case of a frontal lobe cavernoma presenting with recurrent seizures. GTR of the lesion was achieved through the SOE approach with no perioperative complications.
Series infective lesions
Three cases of frontal epidural empyema secondary to complicated paranasal sinusitis were successfully drained through the SOE approach. Postoperative CT scans before discharge revealed complete evacuation and no reaccumulation of pus, and hence, none of the cases needed operative redrainage.
Series traumatic lesions
One patient with a traumatic anterior fossa fracture complicated by a dural tear and CSF leak was efficaciously treated using the SOE approach. Primary dural closure was achieved with addition of an onlay of dural substitute as reinforcement. The CSF fistula resolved.
Four cases of a traumatic frontal supraorbital epidural hematomas and one case of an intracerebral frontal lobe hematoma underwent keyhole evacuation of their bleeds through the SOE approach with complete clot drainage and relief of mass effect.
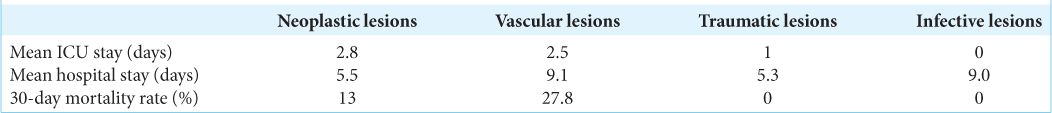
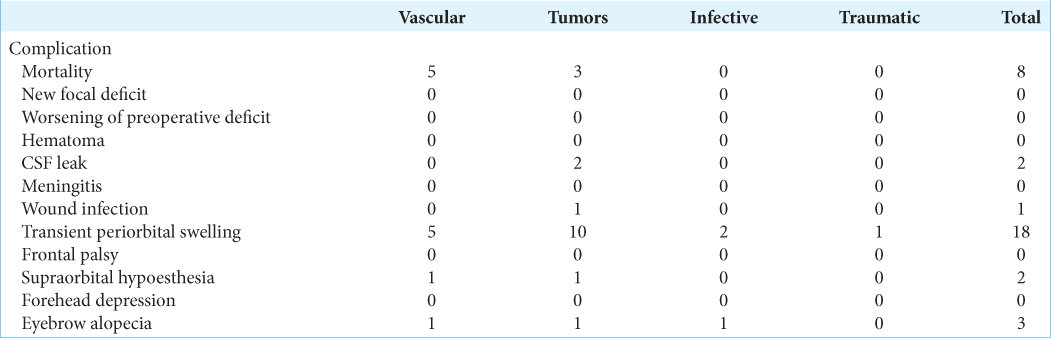
Series outcomes and complications
The mean ICU stay was 2.2 days for the entire series. Patients with infective pathologies did not warrant ICU admission in our resource-constrained setting. The mean ICU stay for the trauma patients was a single day. The aneurysm group had the highest mean total hospital stay due to the extensive in-hospital care needed for management acute aneurysmal subarachnoid hemorrhage. The patients with empyema also stayed relatively longer in hospital as their management warranted at least 7 days of intravenous antibiotics and repeat imaging a week postsurgical drainage [
The mortality rate was higher in the ruptured aneurysm subgroup, five of 17 patients (29.4%) compared to that of the tumor subgroup, 13% (three of 23 patients). All five mortalities in the aneurysmal subgroup presented with WFNS grades of III–V. Four of the patients demised secondary to complications of delayed cerebral ischemia and the other patient demised secondary to neurogenic pulmonary edema. Within the tumor subgroup, there were three mortalities. All three patients had a giant meningioma (≥6 cm diameter). One of the mortalities was due to carotid artery injury. This patient was a redo case who had received radiation therapy before surgery. The other two patients had presented with poor preoperative statuses, both were immobile, blind, and were dependent with activities of daily living. These two patients demised as a result of pulmonary embolism. None of the patients with infective or traumatic lesions died within 30 days. The overall 30-day mortality rate for our series was 16%.
Conversion to a larger craniotomy was not necessary in any of the cases in this series.
The most frequent perioperative complication was transient periorbital swelling which resolved within 7 days. It was observed in 18 of the 50 patients. The next common complications in descending frequency were eyebrow alopecia (three cases), supraorbital hypoesthesia (two cases), CSF leak (two cases), and surgical site infection (one case). The CSF leaks resolved within 5 days of lumbar drain insertion with neither of the cases developing meningitis. None of our patients developed a new neurological deficit or worsening of preoperative deficits. We did not encounter postoperative intracranial hematoma (ICH), frontal palsy, or forehead depression [
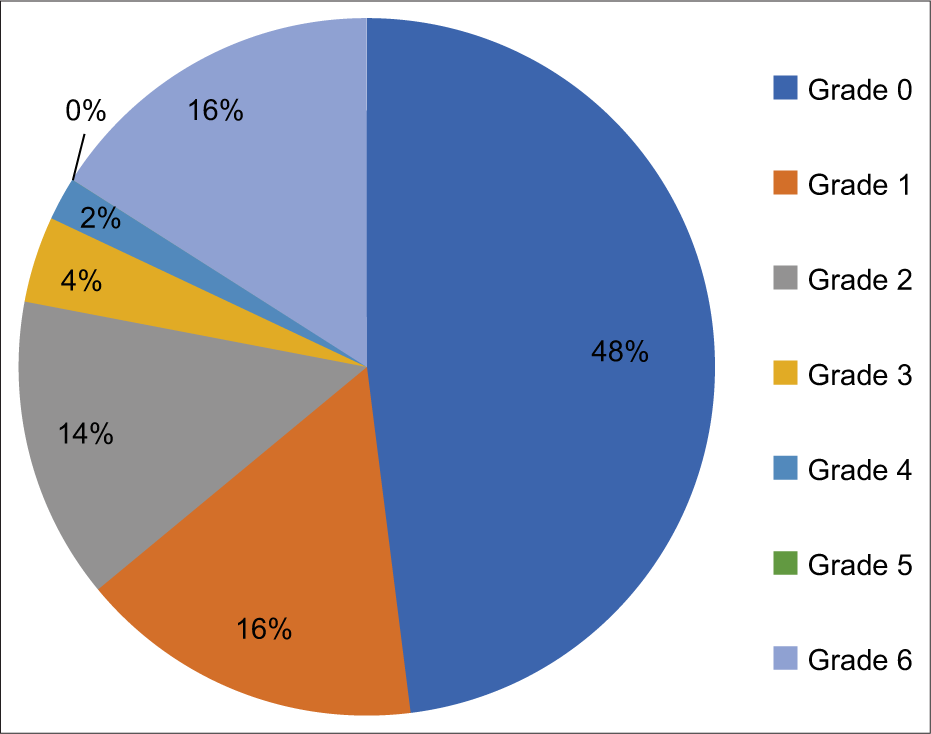
Clinical outcome of our cases was evaluated according to the Modified Rankin Scale (mRS) at 3-month postsurgery. A good clinical outcome (mRS ≤ 2) was achieved for 78% of our patients [
DISCUSSION
Our series presents 50 keyhole supraorbital approach operations for a diverse range of anterior fossa and parasellar pathologies. The majority of supraorbital approaches were utilized for a range of different neoplastic cases, with meningioma being the most common tumor. Our series also presents a reasonable volume of cerebral aneurysms managed successfully through a supraorbital approach. Finally, we also demonstrated that the supraorbital approach can be successfully utilized for both trauma and infective cases.
Patient ages in our series spanned 12 to 86 years and there was a female preponderance of 28 females to 22 males.
Review of our series tumor subset revealed a gross-total resection rate of 87%. For the remainder of cases, NTR was achieved. The supraorbital approach was not limited by tumor size as six of the meningiomas that we resected were giant tumors – diameter ≥6 cm. Furthermore, gross-total resection could also be achieved for glioblastoma, craniopharyngioma, and metastatic disease. Our results are comparable to other series that have opted for keyhole-based tumor resection. Reich and Perneczky reported a gross-total resection rate of 89.2% for skull base meningiomas in the largest reported keyhole supraorbital approach series to date.[
Within our cerebral aneurysm subgroup, 100% clip ligation occlusion was achieved without any acute perioperative complications. All deaths in the aneurysm subgroup were in patients who presented with WFNS subarachnoid haemorrhage grades of ≥ III and the mortalities were a result of complications of SAH. It is important to note that all aneurysms clipped in our series were acutely ruptured and intraoperative rerupture was encountered in only three of the 17 cases. All rerupture cases were managed successfully and there was no need for conversion to a larger craniotomy in our series. Again, our results are comparable to other series that have employed a supraorbital approach for clipping of cerebral aneurysms. In a series of 129 aneurysms clipped through a supraorbital craniotomy by Czirják et al., only two cases could not be completely clipped. In the same series, premature rupture of the aneurysm before clipping occurred in two cases for which both were managed satisfactorily.[
The literature on the management of traumatic and infective lesions through the SOE approach is limited to a few case reports. To the best of our knowledge, no comparable literature was available for the management of traumatic frontal epidural hematoma through the SOE approach. Park et al. reported eight cases of traumatic ICHs successfully treated using this keyhole approach while Oh and Hwang endoscopically evacuated 13 traumatic ICHs through the SOE approach.[
Noggle et al. as well as Hallak et al. each reported three cases of frontal epidural empyema in pediatric patients who were evacuated through the SOE approach.[
The use of endoscopy is a valuable adjunct when conducting the SOE approach. Within our tumor subseries, it was invaluable for our meningioma cases. Following tumor resection, endoscopy allowed for inspection of the tumor bed to ensure residual tumor was resected. Furthermore, endoscopy, particularly with a 30° endoscope, was extremely valuable for our tuberculum sellae meningioma cases. Endoscopy allowed us to resect tumor below the tuberculum sella – a region not visualized microscopically due to the angle being below the line of sight that a microscope can achieve. Finally, for very large tumors, where nerves or vessels were being encased, endoscopy was used to appreciate these critical neurovascular relationships. For our vascular series, endoscopy with a 30° endoscope allowed visualization of potential perforating vessels that were present on the posterior aspect of visualized cerebral vessels. On occasion, this information altered the surgical clipping strategy that would have been employed with pure microscopic view.
The SOE approach offers several advantages compared to conventional craniotomies. There is minimal brain exposure to the outside environment, potentially reduced accidental iatrogenic surgical trauma, and fixed brain retraction is limited or altogether absent. This significantly decreases approach-related surgical morbidity and shortens hospitalization. Mean ICU stay in our series was 2.2 days. Several other authors have reported similar findings of relatively shorter ICU and overall hospital stay.[
Good clinical outcome in our case series according to the mRS at 3 months postsurgery was achieved for 78% of our patients. Patients not achieving a good outcome were largely the result of death in patients with high-grade WFNS SAH and patients presenting with poor preoperative status as a result of giant meningiomas. In our vascular series subgroup, four of the five patients that demised were WFNS Scores IV and V. This is in line with literature analyzing outcomes in poor SAH grade patients. Bogossian et al. analyzed outcomes in 353 Grade IV and V WFNS SAH patients and demonstrated a 57% mortality and 74% unfavorable outcome in this group of patients.[
The traditional subfrontal approaches are associated with frequent cosmetic issues including scaring, cranial depressions, temporalis muscle wasting, injury to the frontalis branch of the facial nerve, supraorbital hypoesthesia, and alopecia.[
The goal of keyhole surgery is to achieve the greatest therapeutic effect while causing the least iatrogenic injury.[
For the SOE approach, the working angle for surgical tools is relatively restricted when compared to the conventional approaches. However, with adequate preoperative planning, extensive review of imaging, precise intraoperative patient positioning, frequent trajectory adjustment, neuronavigation, and brain relaxation with liberal use of lumbar drainage, most anterior skull base and parasellar lesions can be surgically managed successfully through this keyhole approach. Importantly, this can be done with very little brain retraction, with the use of a fixed retractor being employed in only a handful of acutely ruptured aneurysm cases. In our experience, the SOE approach is our first-line approach for the majority of pathologies in the anterior fossa and parasellar regions. Some of the circumstances that may lead us to opt for a mini-pterional as opposed to a SOE approach are presence of significant tumor below the anterior aspect of the sphenoid wing, which makes visualization and safe resection difficult. In our aneurysm series, we prefer to utilize a SOE approach for the majority of ACom aneurysms and ICA bifurcation aneurysms. We utilize a mini-pterional approach for other anterior circulation aneurysms. The ACom aneurysms cases where we did not use the SOE approach were in those patients with multiple aneurysms clipped through a single approach. We also had a single case with an inferiorly pointing ACom aneurysm which at that time was deemed high risk for premature rupture if approached via the SOE. This case was also early on in our SOE approach series.
Limitations faced in our series to a large extent are the result of our practice being based in a middle-income setting. This leads to equipment limitations as well as human resource constraints. A large part of the SOE craniotomy cases in our series was conducted with the use of an outdated microscope until 2020. We also faced human resource challenges, in particular the unavailability of a dedicated neurosurgical theater nursing team. Furthermore, our patients are admitted to a general ICU with severe bed occupancy pressure. This potentially exacerbated the poor outcomes we achieved with our giant meningioma patients that had poor preoperative functional status and our ruptured aneurysm patients who presented with WFNS Grade ≥III.
CONCLUSION
The SOE craniotomy is an effective minimally invasive approach. It requires a limited skin incision, very little soft-tissue dissection, and a small craniotomy, therefore, carrying minimal approach-related morbidity and satisfactory cosmetic results. Our series of 50 cases demonstrates that the SOE keyhole approach can be a useful keyhole approach in tackling various pathologies of the anterior cranial base and parasellar regions. We demonstrate that adequate planning allows for the treatment of neoplastic, vascular, traumatic, and infective pathologies. We also demonstrate that complex pathology and large lesions do not necessitate larger craniotomies and can be adequately treated with a supraorbital approach. With experience, this approach can potentially lead to excellent patient outcomes with little morbidity.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Czirják S, Nyáry I, Futó J, Szeifert GT. Bilateral supraorbital keyhole approach for multiple aneurysms via superciliary skin incisions. Surg Neurol. 2002. 57: 314-23
2. Da Silva CE, de Freitas PE. Large and giant skull base meningiomas: The role of radical surgical removal. Surg Neurol Int. 2015. 29;6: 113
3. Fonseca RB, Correia AO, Vieira R.S. Comparative study between minimally invasive supraorbital craniotomy and pterional craniotomy for treating anterior circulation cerebral aneurysms in a low-resource setting. Sci Rep. 2021. 11: 5555
4. Gazzeri R, Nishiyama Y, Teo C. Endoscopic supraorbital eyebrow approach for the surgical treatment of extraaxial and intraaxial tumors. Neurosurg Focus. 2014. 37: E20
5. Gouvêa Bogossian EG, Diaferia D, Minini A, Djangang N, Menozzi M, Peluso L. Time course of outcome in poor grade subarachnoid hemorrhage patients: A longitudinal retrospective study. BMC Neurol. 2021. 21: 196
6. Hallak H, Abou-Al-Shaar H, Mallela AN, McDowell MM, Jabbour N, Padia R. The eyebrow approach for the management of pediatric frontal epidural abscesses secondary to diffuse sinusitis. Pediatr Neurosurg. 2022. 57: 213-21
7. Iacoangeli M, Nocchi N, Nasi D, DI Rienzo A, Dobran M, Gladi M. Minimally invasive supraorbital keyhole approach for the treatment of anterior cranial fossa meningiomas. Neurol Med Chir (Tokyo). 2016. 56: 180-5
8. Lan Q. Clinical application of keyhole techniques in minimally invasive neurosurgery. Chin Med J (Engl). 2006. 119: 1327-30
9. Lan Q, Sughrue M, Hopf NJ, Mori K, Park J, AndradeBarazarte H. International expert consensus statement about methods and indications for keyhole microneurosurgery from international society on minimally invasive neurosurgery. Neurosurg Rev. 2021. 44: 1-17
10. Meixensberger J, Meister T, Janka M, Haubitz B, Bushe KA, Roosen K. Factors influencing morbidity and mortality after cranial meningioma surgery-a multivariate analysis. Acta Neurochir Suppl. 1996. 65: 99-101
11. Narayan V, Bir SC, Mohammed N, Savardekar AR, Patra DP, Nanda A. Surgical management of giant intracranial meningioma: Operative nuances, challenges, and outcome. World Neurosurg. 2018. 110: e32-41
12. Noggle JC, Sciubba DM, Nelson C, Garcés-Ambrossi GL, Ahn E, Jallo GI. Supraciliary keyhole craniotomy for brain abscess debridement. Neurosurg Focus. 2008. 24: E11
13. Oh HJ, Hwang SC. Supraorbital endoscopic evacuation for traumatic intracerebral hematomas in the frontal lobe. J Korean Neurosurg Soc. 2022. 65: 846-52
14. Ormond DR, Hadjipanayis CG. The supraorbital keyhole craniotomy through an eyebrow incision: Its origins and evolution. Mini Invasive Surg. 2013. 2013: 296469
15. Park E, Moon SK, Eom KS. Comparison of the surgical approaches for frontal traumatic intracerebral hemorrhage. J Trauma Injury. 2019. 32: 71-9
16. Pernecsky A, Müller-Forell W, Van Lindert E, Frites G, editors. Keyhole Concept in Neurosurgery. Stuttgart, Germany: Thieme Medical Publishersany; 1999. p.
17. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55 discussion 242-55
18. Seaman SC, Ali MS, Marincovich A, Osorno-Cruz C, Greenlee JD. Single surgeon experience with minimally invasive supraorbital craniotomy versus bifrontal craniotomy for anterior skull base meningiomas. Surg Neurol Int. 2020. 11: 458
19. Van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: Concept and technique. Surg Neurol. 1998. 49: 481-9
20. Wiedemayer H, Sandalcioglu IE, Wiedemayer H, Stolke D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Mini Invasive Neurosurg. 2004. 47: 221-5
21. Wilson DA, Duong H, Teo C, Kelly DF. The supraorbital endoscopic approach for tumors. World Neurosurg. 2014. 82: e243-56
22. Ziai K, Shah S, Daggubati LC, Zacharia BE, Lighthall JG. The supraorbital approach via an eyebrow incision: Analysis of cosmetic outcomes using the scar cosmesis assessment rating scale. J Craniofac Surg. 2022. 33: 307-11