- Department of Neurological Surgery University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
- Department of Neurology and Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Dr. George Zenonos, Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_355_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vivek Sudhakar1, Zachary Gersey1, Sean P. Polster1, Megan Mantica2, George Zenonos1. Supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids: A case report and literature review. 06-Jul-2021;12:327
How to cite this URL: Vivek Sudhakar1, Zachary Gersey1, Sean P. Polster1, Megan Mantica2, George Zenonos1. Supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids: A case report and literature review. 06-Jul-2021;12:327. Available from: https://surgicalneurologyint.com/surgicalint-articles/10951/
Abstract
Background: Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids is a rare disorder that presents with subacute brainstem symptoms such as ataxia, facial paresthesias, and episodic diplopia, thought to be due to a T-cell medicated perivascular inflammatory process. A supratentorial variant, Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS), has been described in only three patients.
Case Description: A 71-year-old male presented with word-finding difficulties, confusion, and left leg weakness. Radiographic workup demonstrated multiple supratentorial ring-enhancing lesions. PET/CT demonstrated hypermetabolism and susceptibility-weighted imaging demonstrated a hemorrhagic component. Frozen pathology revealed a predominately T-cell and monocyte inflammatory infiltrate. He demonstrated interval improvement to dexamethasone therapy, but then demonstrated worsening of his symptoms following discontinuation.
Conclusion: Given his dramatic response to corticosteroids, he was diagnosed with SLIPPERS. SLIPPERS is an underrecognized diagnostic entity to consider in patients with ring-enhancing lesions and can present with hypermetabolic lesions on PET/CT.
Keywords: CLIPPERS, CNS lymphoma, Neuroimmunology, SLIPPERS
INTRODUCTION
Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS) was first described by Pittock et al. in eight patients who presented with various brainstem symptoms such as episodic diplopia, ataxia, and facial paresthesias.[
CASE DESCRIPTION
History, physical examination, and baseline imaging
A 71-year-old male presented with a 3-month history of word-finding difficulties, confusion, and left leg weakness. CT head demonstrated several ill-defined hypodense areas within the right parietal and occipital subcortical white matter. MRI of the brain demonstrated a contrast-enhancing 3.2 cm lesion in the right occipital lobe, a 1.8 cm enhancing lesion in the right precentral gyrus, and multiple smaller enhancing lesions in the right periventricular region with associated vasogenic edema but no mass effect [
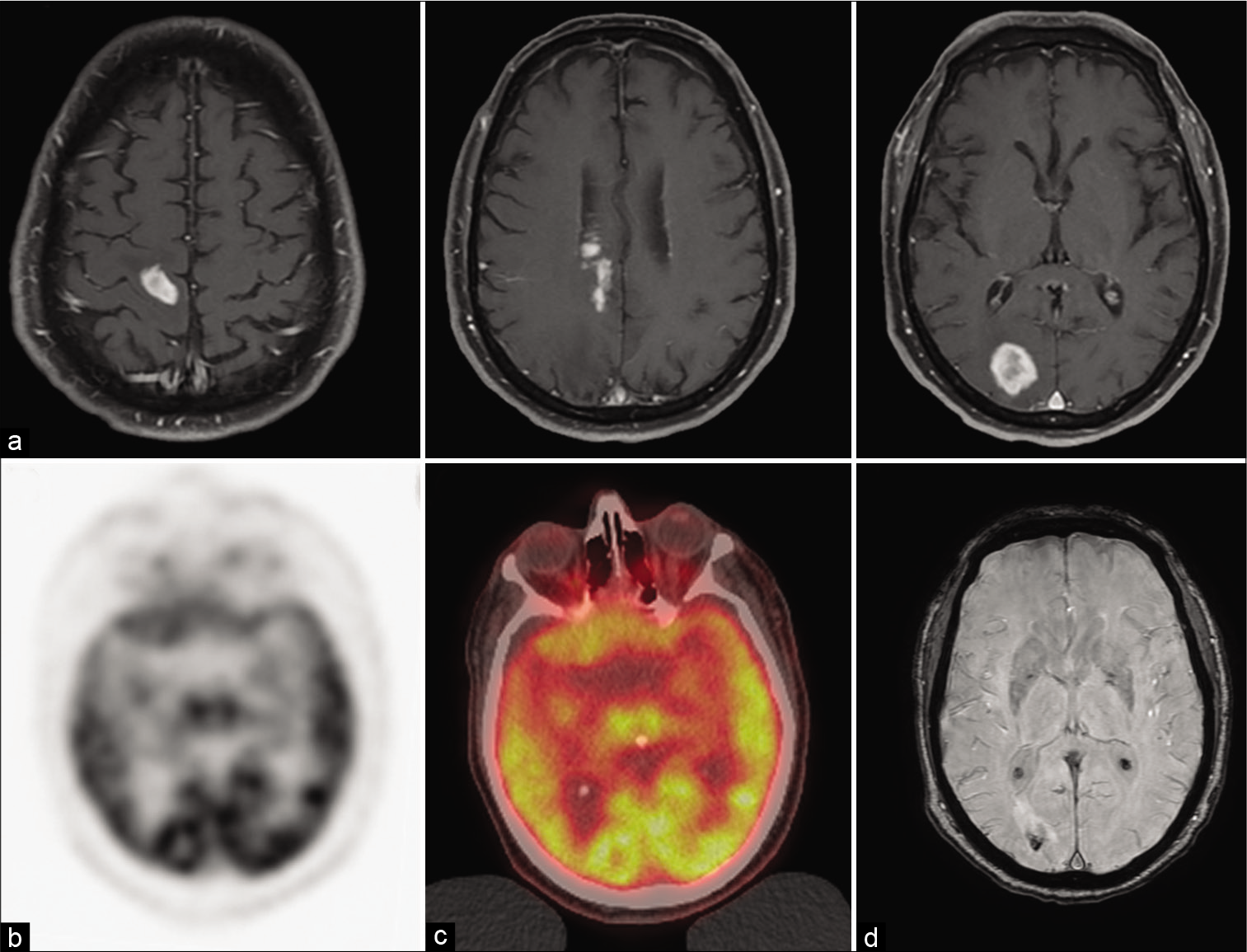
Figure 1:
Initial pre-operative radiographic appearance of mass lesion. (a) Pre-operative axial T1 MRI with contrast demonstrating contrast-enhancing lesions in the right occipital lobe, right precentral gyrus, and within the right periventricular region. (b) Axial PET imaging and (c) PET/CT demonstrating a hypermetabolic lesion in the right posterior occipital lobe. (d) Axial SWAN imaging demonstrates a hemorrhagic component of the right occipital lesion.
Surgical core biopsy
A needle core biopsy was obtained of the right occipital lesion, and intraoperative frozen pathology was thought to be consistent with a lymphoma. Formal pathology, however, only showed an intense inflammatory process [
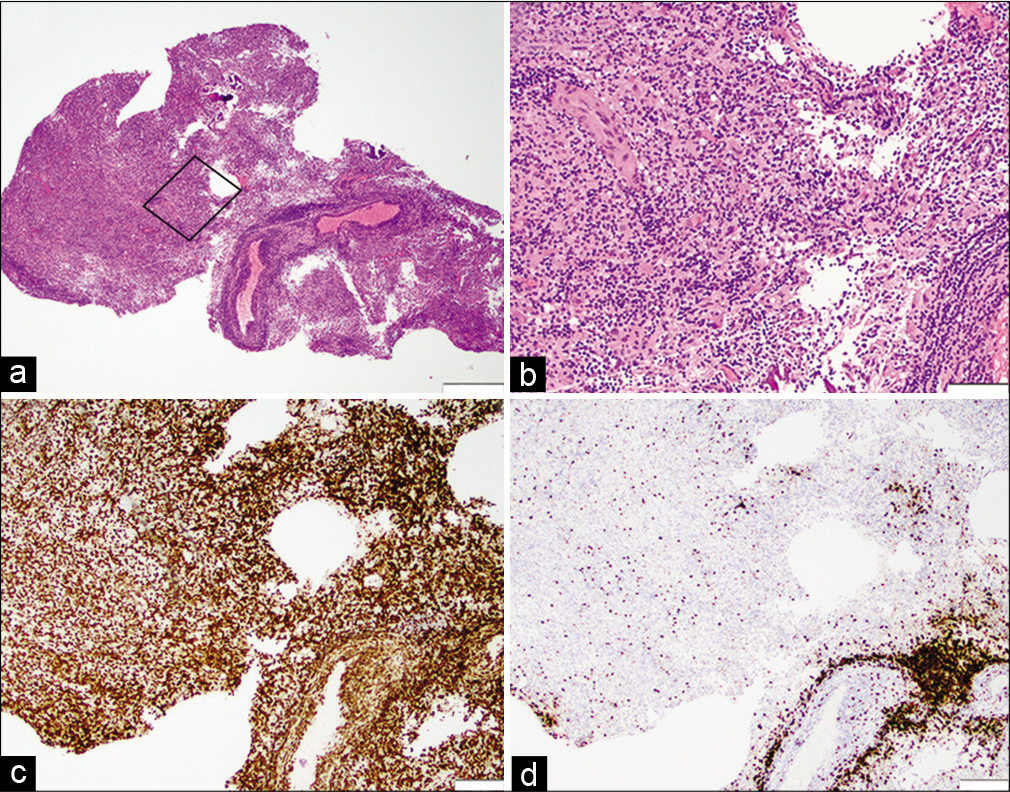
Figure 2:
Histologic characterization of frozen biopsy sample. (a) ×2 and (b) ×10 H and E demonstrating brisk parenchymal and perivascular infiltrate of small lymphocytes in a background of marked reactive astrocytosis. (c) CD20 immunohistochemistry highlights many small B-cells in a predominantly perivascular distribution. (d) CD3 immunohistochemistry highlights numerous small T-cells. Scale bars: 500 µm for (a), 100 µm for (b), 200 µm for (c) and (d).
Postoperatively, he was started on high-dose dexamethasone. However, this was discontinued once the formal pathology was available. A follow-up brain MRI after 1 month demonstrated a decrease in the size of all enhancing lesions. MRI of the total spine was without evidence of disease. Dexamethasone was subsequently tapered off given initial concern for sentinel lymphomatous lesions.
CSF studies, ordered 2 months after the patient’s biopsy, were unremarkable for autoimmune, bacterial, viral, fungal, parasitic, or inflammatory etiologies. CSF flow cytometry was limited by the low cellularity of the specimen but revealed a predominance of CD5+ T cells. Repeat MRI brain off of corticosteroids demonstrated an interval increase in size and conspicuity of all previously observed enhancing lesions, and the decision was made to perform an excisional biopsy of the right occipital lesion.
Surgical excisional biopsy
The patient was brought to the operating room for excisional biopsy of the right occipital lesion. He was positioned supine with his head placed in the Mayfield head holder. The field was prepped and draped, and an incision was made down to the bone. A burr hole was made, and a craniotomy was turned over the lesion as confirmed with image-guidance. There was a pale tan pink discoloration of the brain. Several biopsies were obtained, and then the lesion was resected under the microscope and sent for pathology.
Pathology
Further histological analysis demonstrated areas of macrophages/lymphocytes with markedly reactive astrocytes that showed quick transition to reactive less inflamed cortex. The lymphocytic population appeared small, but polymorphous, containing scattered plasma cells. There was marked perivascular inflammation but no fibrinoid necrosis. Flow cytometric and immunohistochemical workup failed to demonstrate a definitely clonal lymphocyte population. There was no evidence of demarcated myelin loss or a vasculitic process.
Post-operative course
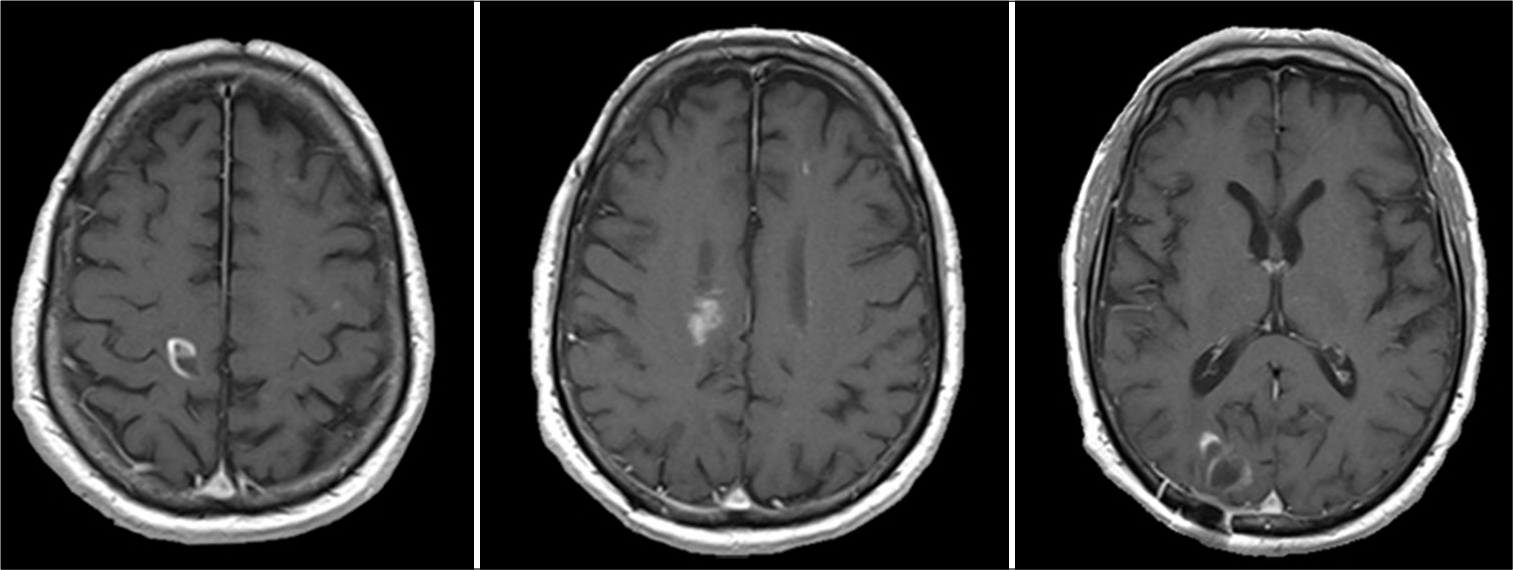
Two weeks postoperatively, he had worsening behavioral outbursts, frequent mood fluctuations, poor comprehension, and worsening balance. Given the clinical deterioration, he was restarted on high-dose dexamethasone. The following MRI demonstrated post-surgical changes with significant decrease in the size of the right occipital lesion [
DISCUSSION
In the two cases described by Armand et al., inflammatory ring-enhancing lesions were observed that were confined to the supratentorial space.[
CONCLUSION
This case demonstrates similarities with previously described SLIPPERS cases while also expanding the pathological phenotype. Our patient is the first report of pathologic lesions showing hypermetabolism on PET/CT. SLIPPERS, as a mimic of primary CNS lymphoma with FDG avidity on PET imaging, is important for neurologists to recognize as it is highly steroid responsive. Further characterization of the cerebral perivascular inflammatory infiltrate is needed to guide diagnosis and whether patients that have disease that has relapsed or become refractory to steroids would respond to an anti-CD3 antibody in the event of corticosteroid failure or relapse.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank our patient for allowing the details of his case to be shared.
References
1. Armand C, Graber J, Lado F, LaSala P, Weidenheim K. SLIPPERS: Supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids: A case report (P5.118). Neurology. 2015. 84: P5.118
2. Horng S, Crary J, Fabian M. A case of SLIPPERS (supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids) presenting with isolated cognitive dysfunction (P1.336). Neurology. 2017. 88: P1.336
3. Pittock SJ, Debruyne J, Krecke KN, Giannini C, van den Ameele J, de Herdt V. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain. 2010. 133: 2626-34