- Department of Neurological Surgery, Loyola University Medical Center, Maywood, Illinois, United States.
Correspondence Address:
Daphne Li, Department of Neurological Surgery, Loyola University Medical Center, 2160 S 1st Ave, Maywood - 60153, Illinois, United States.
DOI:10.25259/SNI_593_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daphne Li, Douglas E. Anderson, Russ P. Nockels. Surgical correction of pediatric spinal deformities with coexisting intraspinal pathology: A case report and literature review. 03-Aug-2021;12:381
How to cite this URL: Daphne Li, Douglas E. Anderson, Russ P. Nockels. Surgical correction of pediatric spinal deformities with coexisting intraspinal pathology: A case report and literature review. 03-Aug-2021;12:381. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11023
Abstract
Background: Surgical correction of spinal deformities with coexisting intraspinal pathology (SDCIP) requires special consideration to minimize risks of further injury to an already abnormal spinal cord. However, there is a paucity of literature on this topic. Here, the authors present a pediatric patient with a residual pilocytic astrocytoma and syringomyelia who underwent surgical correction of progressive postlaminectomy kyphoscoliosis. Techniques employed are compared to those in the literature to compile a set of guidelines for surgical correction of SDCIP.
Methods: A systematic MEDLINE search was conducted using the following keywords; “pediatric,” “spinal tumor resection,” “deformity correction,” “postlaminectomy,” “scoliosis correction,” “intraspinal pathology,” “tethered cord,” “syringomyelia,” or “diastematomyelia.” Recommendations for surgical technique for pediatric SDCIP correction were reviewed.
Results: The presented case demonstrates recommendations that primarily compressive forces on the convexity of the coronal curve should be used when performing in situ correction of SDCIP. Undercorrection is favored to minimize risks of traction on the abnormal spinal cord. The literature yielded 13 articles describing various intraoperative techniques. Notably, seven articles described use of compressive forces on the convex side of the deformity as the primary mode of correction, while only five articles provided recommendations on how to safely and effectively surgically correct SDCIP.
Conclusion: The authors demonstrated with their case analysis and literature review that there are no clear current guidelines regarding the safe and effective techniques for in situ correction and fusion for the management of pediatric SDCIP.
Keywords: Intramedullary spinal tumor, Intraspinal pathology, Kyphoscoliosis, Pediatric spinal deformity correction
INTRODUCTION
Surgical techniques for the correction of idiopathic pediatric scoliotic deformities are well documented. However, various intraspinal pathologies, such as diastematomyelia, tethered cord, syringomyelia, and intramedullary spinal cord tumors (IMSCTs), create a unique set of considerations to be addressed during surgical planning and management of these three-dimensional spinal deformities. Unfortunately, there is little documentation of the appropriate surgical technique and guidelines for safely performing correction of spinal deformities with coexisting intraspinal pathology (SDCIP).
Here, the authors reviewed the literature on surgical techniques/recommendations for managing pediatric SDCIP, while also presenting an illustrative case of progressive postlaminectomy kyphoscoliosis in a pediatric patient 9 years after subtotal resection of an intramedullary spinal cord tumor (IMSCT).
MATERIALS AND METHODS
A pediatric case of SDCIP with IMSCT was reviewed and accompanied by a literature search of MEDLINE using of the keywords; “pediatric,” “intradural spinal tumor,” “spinal tumor resection,” “deformity correction,” “postlaminectomy,” “intraspinal pathology,” “tethered cord,” “syringomyelia,” or “diastematomyelia” [
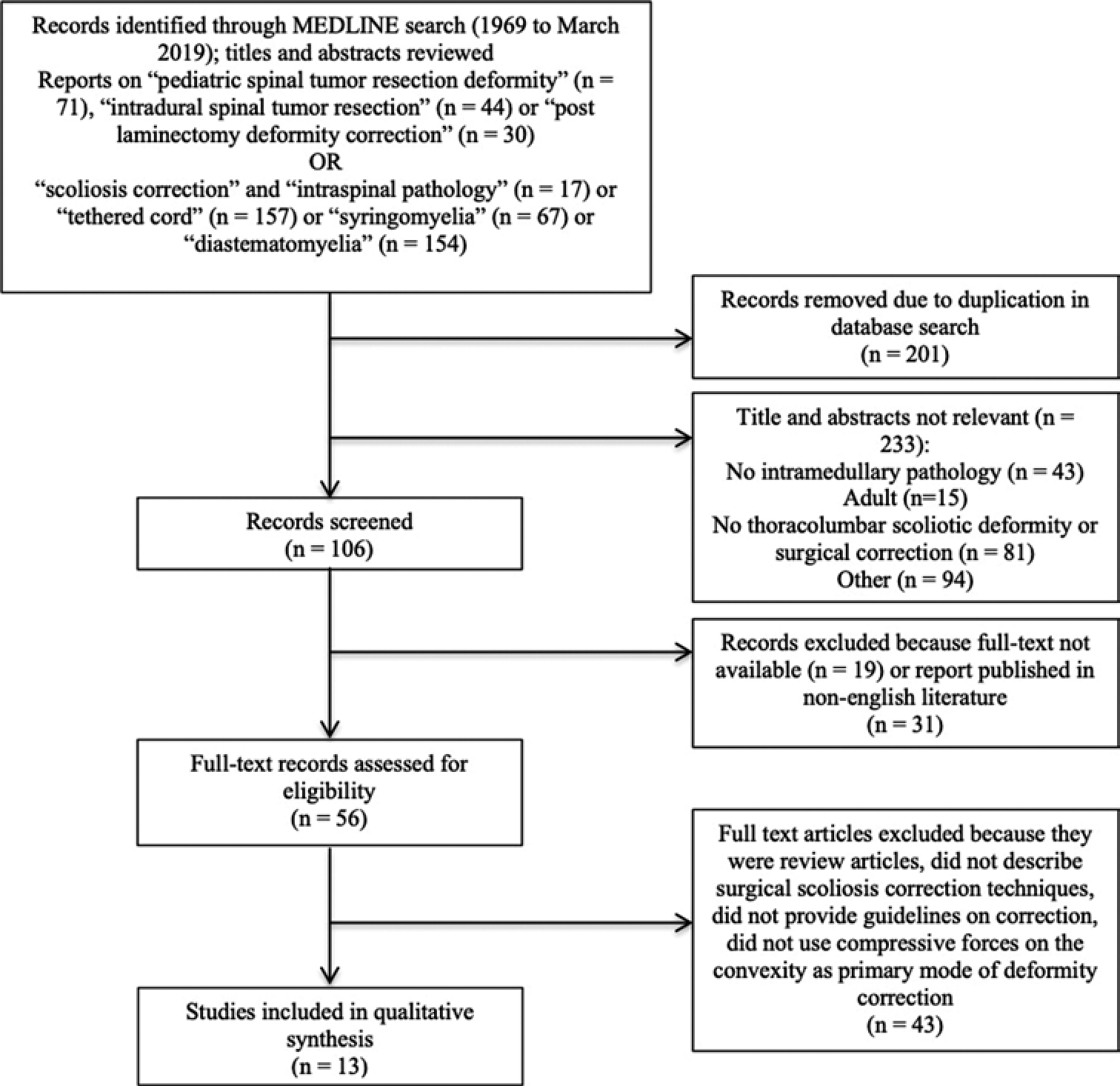
Figure 1:
(a) PRISMA flow diagram of citations identified and evaluated on literature review of scoliotic deformity correction in patients after spinal cord tumor resection. (b) PRISMA flow diagram of citations identified and evaluated on literature review of scoliotic deformity correction in patients with other intraspinal pathology.
CASE REPORT
History
In 2007, at the age of 2, the patient underwent thoracic six (T6) to lumbar two (L2) laminectomies, for subtotal resection (STR) of a pilocytic astrocytoma with expansion duraplasty [
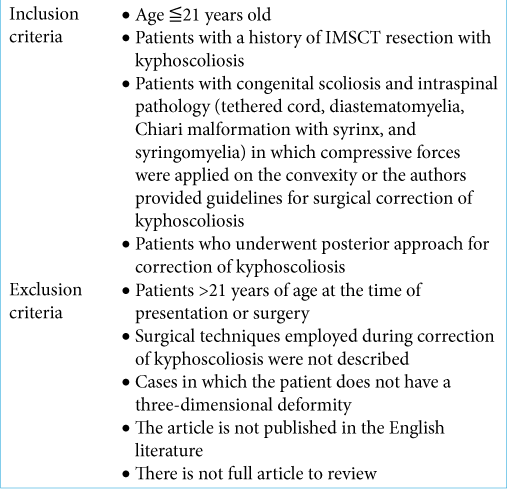
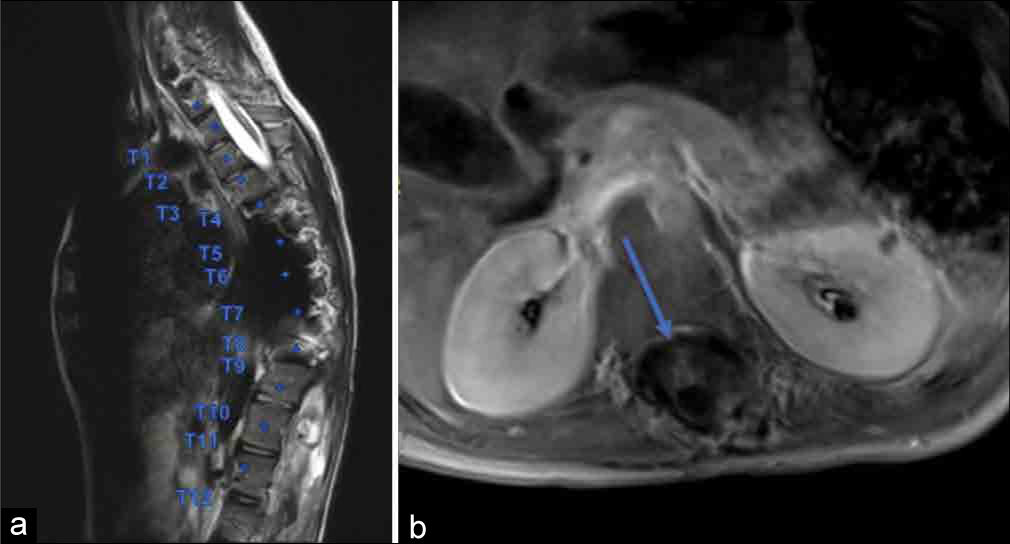
Figure 2:
T1 postcontrast thoracic (a) and lumbar (b) and T2 noncontrast thoracic (c) and lumbar (d) sagittal midline views of patient’s postoperative MRI demonstrate an expansile, intramedullary astrocytoma extending from T7 to L3 is demonstrated with associated syringohydromyelia extending from C2 to T7 with a remodeled and expanded spinal canal after decompressive laminectomies were performed from T7 to L3.
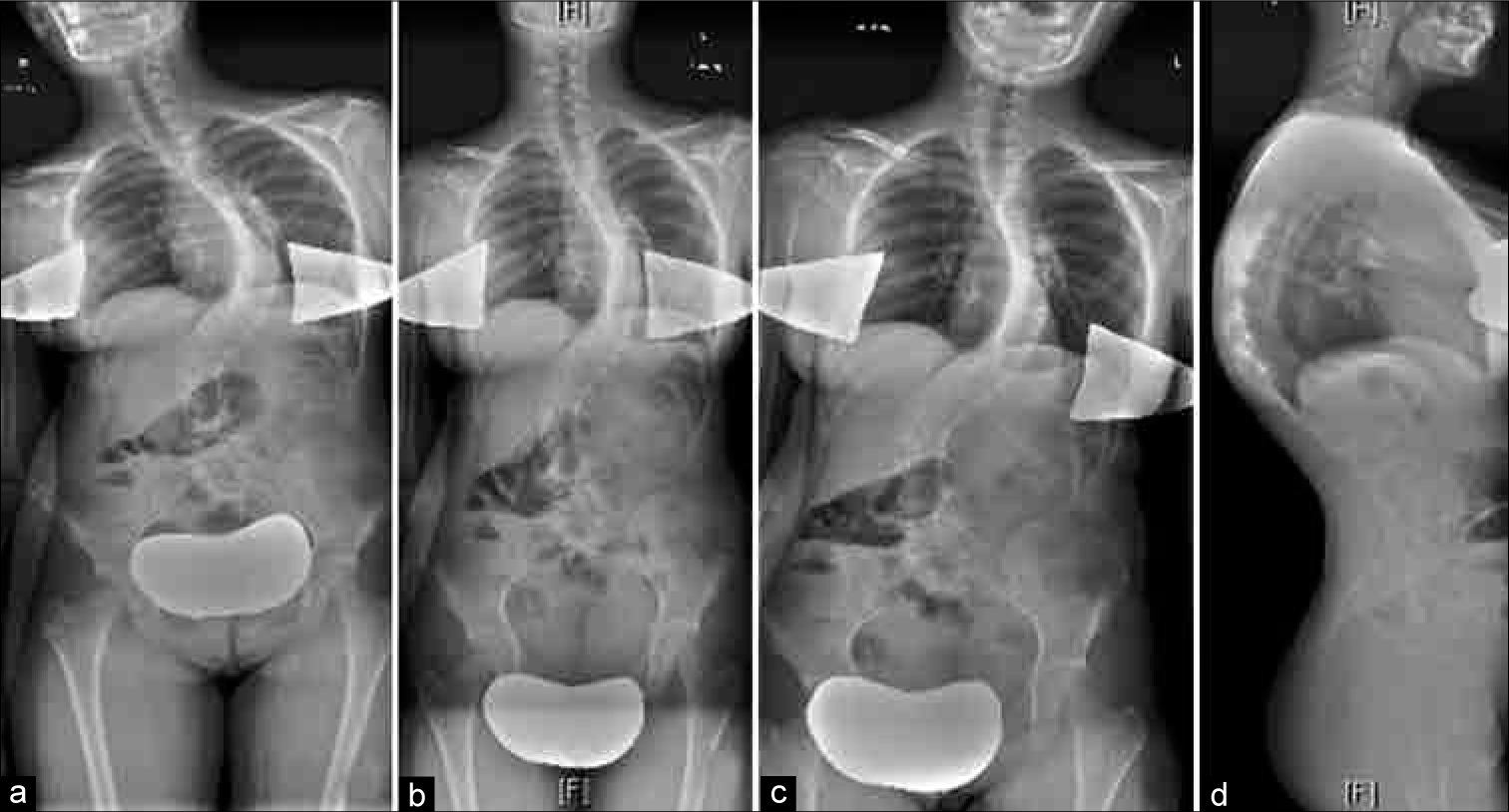
At 5 years of age, the patient had shoulder asymmetry in the horizontal plane and an increased thoracic kyphosis that was initially managed conservatively with external bracing. Over the next few years, the patient’s kyphoscoliosis continued to progress [
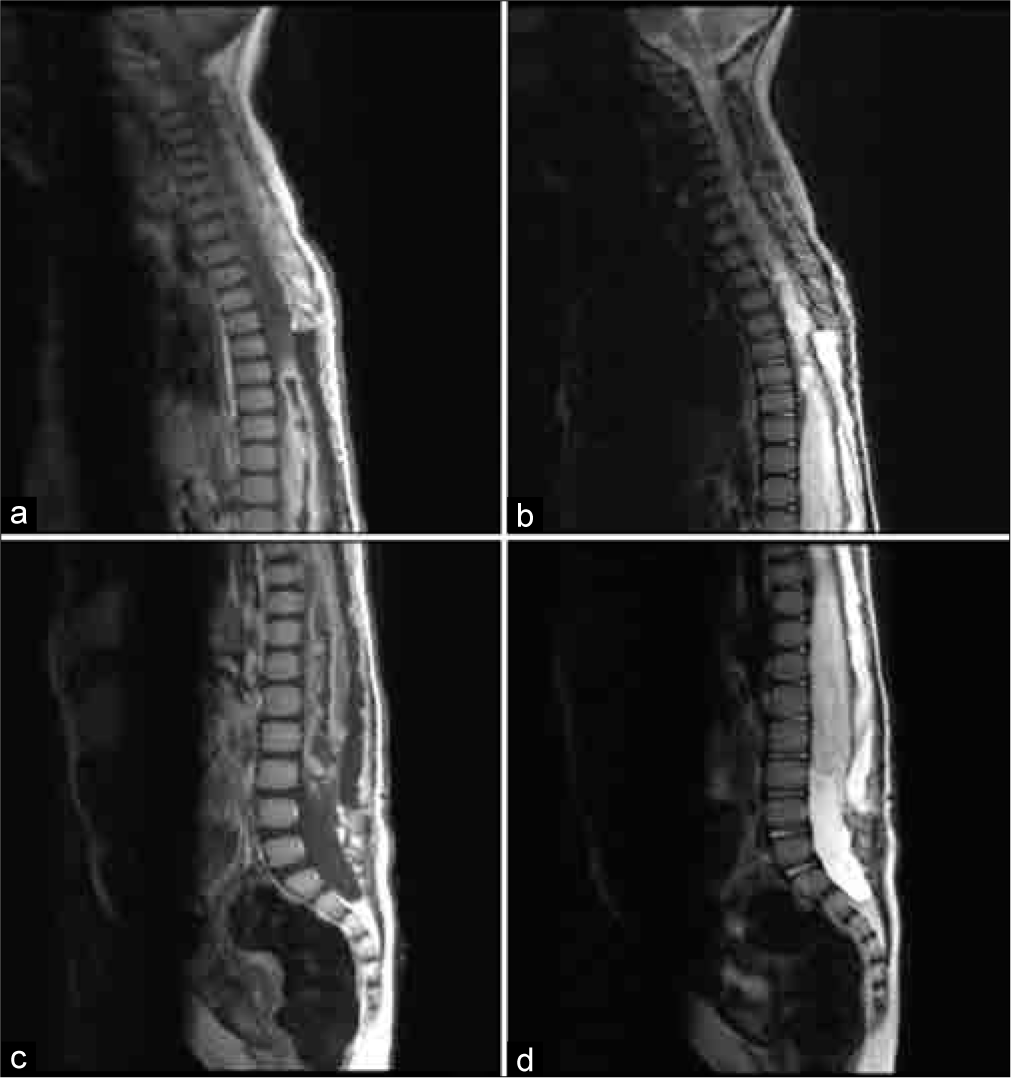
Figure 3:
Serial standing scoliosis radiographs. (a,d) Preoperative AP and lateral radiographs before laminectomy and tumor resection. (b,e) First postoperative standing long-cassette thoracolumbar radiographs, AP and lateral, obtained in 2010, treated with external bracing. (c,f) Interval AP and lateral standing long-cassette thoracolumbar radiographs obtained in 2015 demonstrating a progressive kyphoscoliosis. (g) Continued progression of scoliosis seen on subsequent AP long-cassette thoracolumbar radiographs obtained in 2016. (h) Hand radiographs obtained to evaluate patient’s bone age in 2015, which was determined to be advanced of her chronologic age.
Figure 4:
Interval postoperative MRI obtained to evaluate for tumor recurrence or progression revealed new enhancing 6 mm nodule at level of T11/12, deemed clinically insignificant in context of progressive kyphoscoliosis and stable in appearance on subsequent MRIs. (a) T2 noncontrast image of thoracic spine in sagittal plane, with evidence of significant coronal deformity as well as T2 hyperintense cystic lesions in the lower thoracic spine. (b) T1 postcontrast image of the thoracic spine at the inferior aspect of T11 with evidence of enhancing nodule (blue arrow).
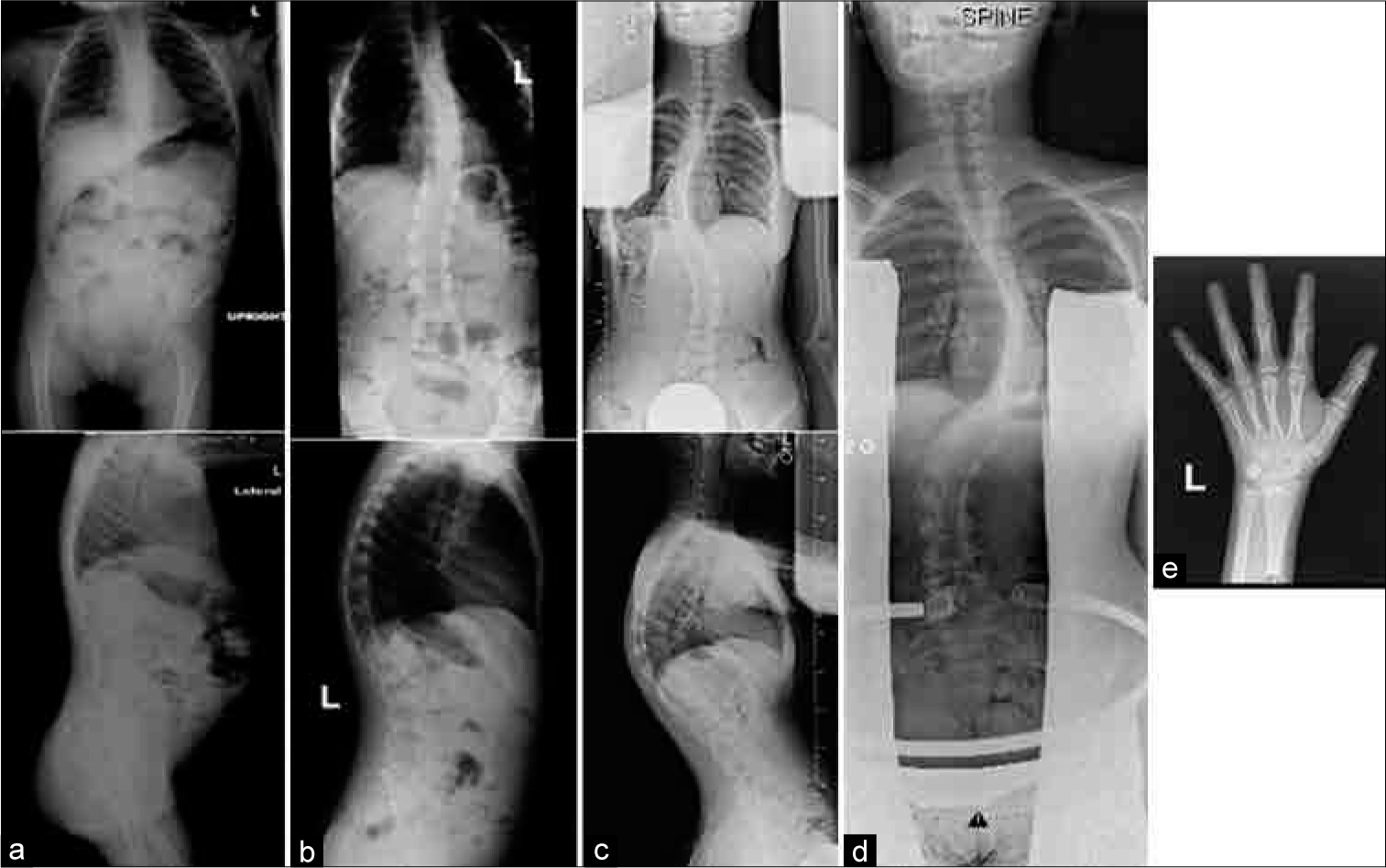
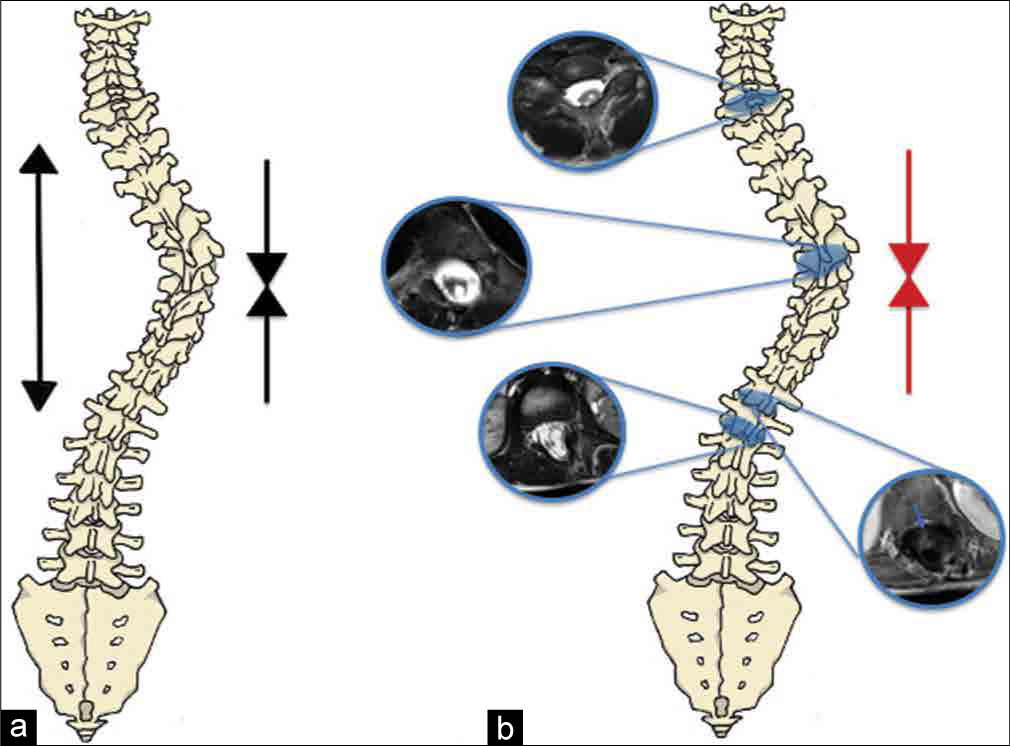
Figure 5:
Preoperative standing scoliosis radiographs including right lateral bending (a), upright AP (b), left lateral bending (c), and upright lateral (d) views. These films show a Lenke type 3+ scoliotic curve – levoscoliosis of the thoracic spine with cobb angle 46° and apex at T8, as well as a dextroscoliosis of the lumbar spine with a Cobb angle of 41° and apex at L2. There was minimal improvement of the patient’s coronal deformity on lateral bending. The patient also has a thoracic kyphosis of 80 degrees. The optimal lowest instrumented vertebra was determined by the neutralization of the L2-3 disc space on left-sided bending radiographs (c).
Operation
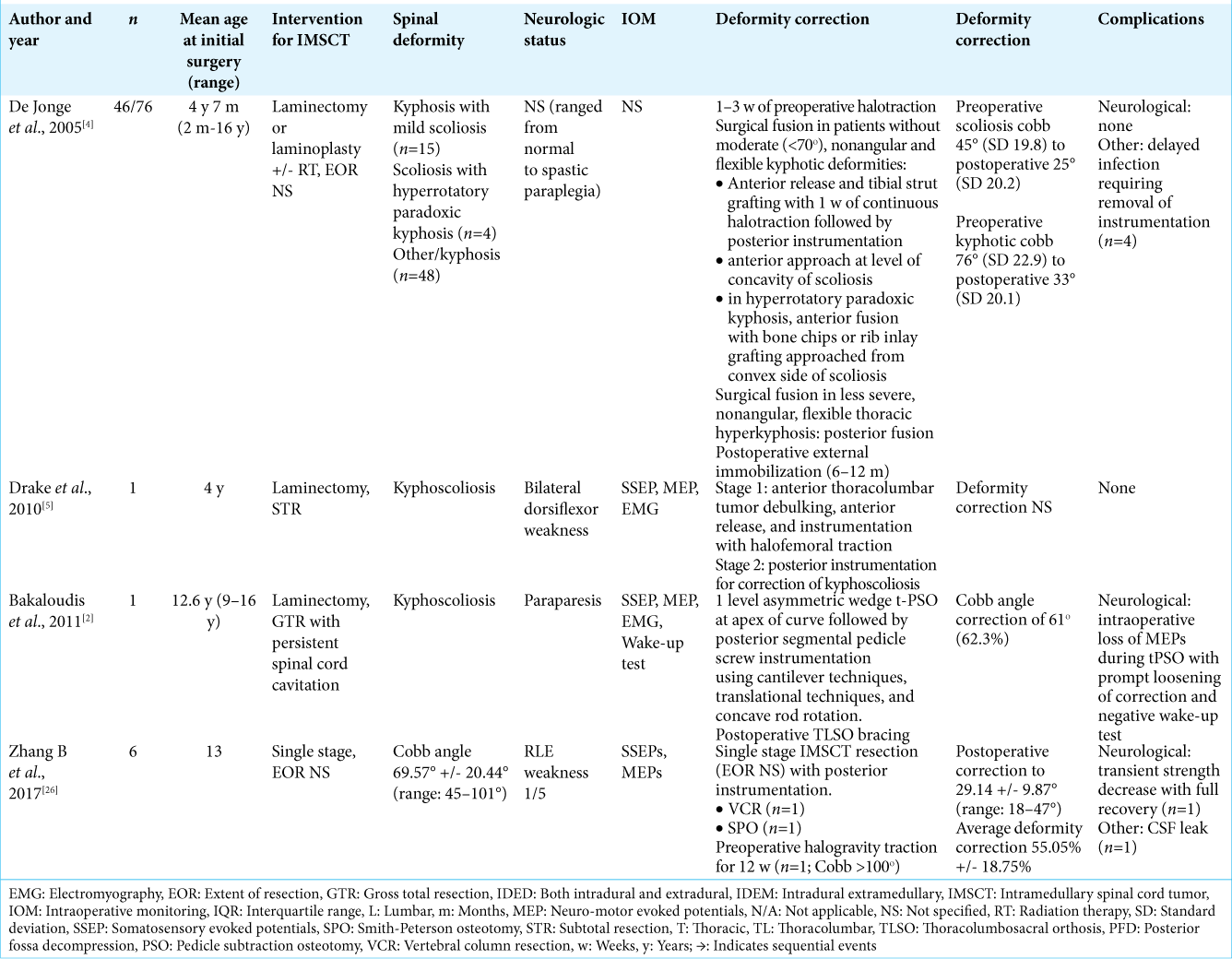
Laminectomies and facetectomies from T3-T12 ensured mobility of thoracic spine and extensive Smith-Petersen type osteotomies were undertaken from T5 to T11 to aid with correction of the kyphotic deformity. Pedicle screw fixation was performed and 5.5 mm CoCh rods, placed bilaterally from T3 to L2. Correction of the patient’s coronal and sagittal deformity was accomplished utilizing a combination of cantilever and in situ compression maneuvers. The patient’s coronal deformity was primarily fixed through compression of the convex aspect of her curve [
Figure 6:
(a) Typical distraction and compressive forces (black arrows) placed along apex of coronal deformity in the absence of intraspinal pathology. (b) Utilization of primarily compressive forces (red arrows) along convexity of the curve to prevent over lengthening the spinal canal in the presence of intraspinal pathology, as was the case in our patient. Select axial T2-weighted noncontrast and one T1-weighted postcontrast MRI cross-sections of her spine highlight progressive intradural tumor (blue circles), cysts, and syringomyelia.
Postoperative course
The patient’s postoperative standing scoliosis radiographs demonstrated significant reduction of her kyphoscoliosis [
LITERATURE REVIEW
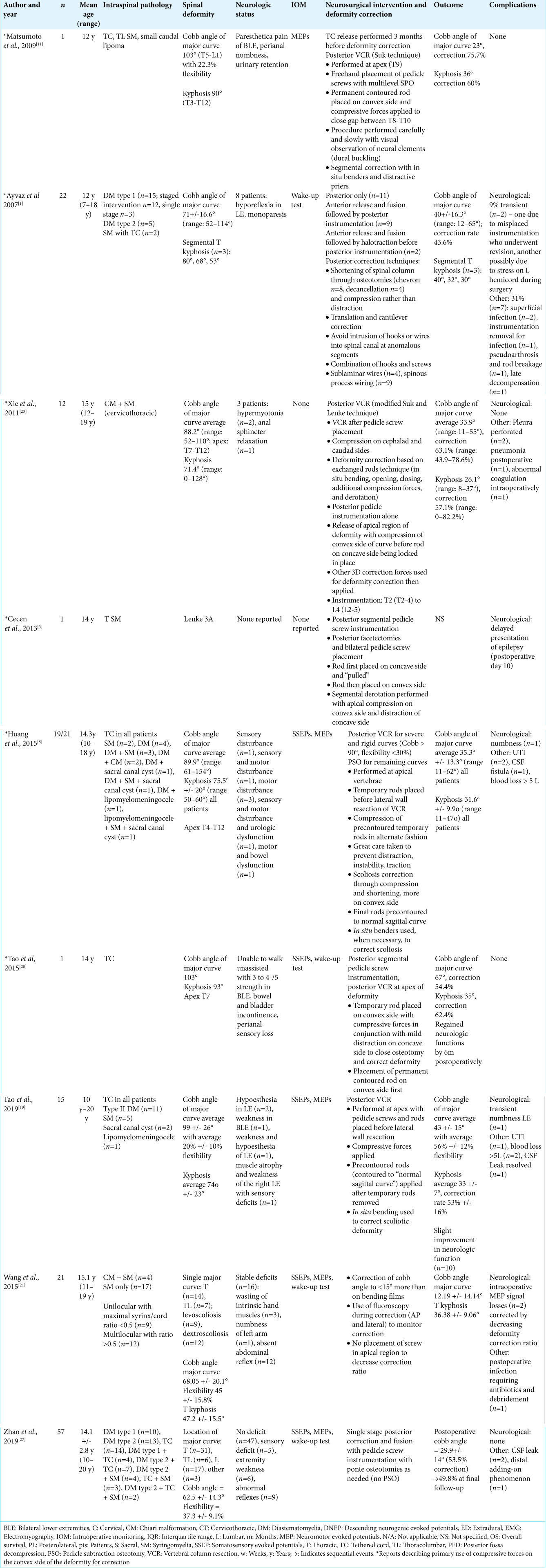
Our review of the literature yielded four articles that described intraoperative approaches and techniques for the management of postlaminectomy spinal deformity in pediatric patients after IMSCT resection [
Surgical approaches described varied between single-stage posterior surgery versus staged deformity correction procedures with anterior release followed by posterior fusion. Nine articles described the use of osteotomies or posterior vertebral column resection to correct kyphoscoliotic deformities without lengthening the spinal column.[
Neuromonitoring, with SSEPs or MEPs, was used in all but two articles reviewed.[
DISCUSSION
The reported incidence of progressive spinal deformity after childhood resection of IMSCTs ranges from 16 to 80%, with increased incidence after laminectomies in the cervical or thoracic spine, and in younger patients.[
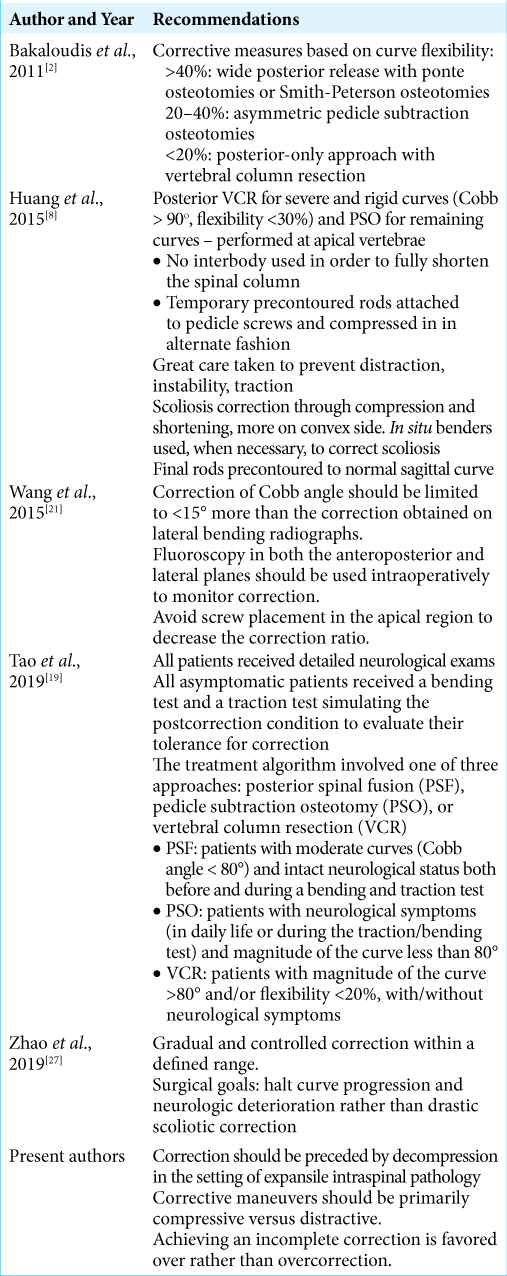
Given the authors’ experience, as illustrated in the presented case, and the prevalence of postlaminectomy spinal deformity requiring fusion, the authors sought to review the English literature and discuss surgical techniques currently used, to guide recommendations for safe maximal spinal deformity correction. The authors focused the review primarily on articles that discussed in situ deformity correction.[
Having extensively reviewed the literature, the authors of this article would agree with recommendations favoring incomplete correction, rather than overcorrection, due to the increased risks of symptomatic spinal cord pathology. Expansile intraspinal pathology should be decompressed before deformity correction. Notably, a portion of articles in our literature review described rod rotation and translation primarily from the concave side[
The authors acknowledge that the literature review summary provided in
CONCLUSION
As illustrated in the present case, SDCIP can be safely and effectively surgically corrected using compressive maneuvers of the convexity of the curve with the goals of gradual and conservative correction to reduce the increased neurovascular risks secondary to an expanded and abnormal spinal cord.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Daphne Li, Douglas Anderson, and Russ Nockels. The first draft of the manuscript was written by Daphne Li and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
1. Ayvaz M, Alanay A, Yazici M, Acaroglu E, Akalan N, Aksoy C. Safety and efficacy of posterior instrumentation for patients with congenital scoliosis and spinal dysraphism. J Pediatr Orthop. 2007. 27: 380-6
2. Bakaloudis G, Lolli F, Silvestre M, Greggi T, Astolfi S, Martikos K. Thoracic pedicle subtraction osteotomy in the treatment of severe pediatric deformities. Eur Spine J. 2011. 20: 95-104
3. Cecen GS, Gulabi D, Oltulu I, Onay T. Generalized epileptic seizure in an adolescent idiopathic scoliosis (AIS) patient with syringomyelia after deformity correction surgery. Int J Surg Case Rep. 2013. 4: 740-3
4. de Jonge T, Slullitel H, Dubousset J, Miladi L, Wicart P, Illés T. Late-onset spinal deformities in children treated by laminectomy and radiation therapy for malignant tumours. Eur Spine J. 2005. 14: 765-71
5. Drake J, Zeller R, Kulkarni AV, Strantzas S, Holmes L. Intraoperative neurophysiological monitoring during complex spinal deformity cases in pediatric patients: Methodology, utility, prognostication, and outcome. Childs Nerv Syst. 2010. 26: 523-44
6. Gokaslan ZL, Quinones-Hinojosa A.editorsManagement of Intramedullary Spinal Cord Tumors. Philadelphia, PA: Elsevier; 2012. Ch. 188: 2135-43
7. Hall JE, Herndon WA, Levine CR. Surgical treatment of congenital scoliosis with or without Harrington instrumentation. J Bone Joint Surg Am. 1981. 63: 608-19
8. Huang JH, Yang WZ, Shen C, Chang MS, Li H, Luo ZJ. Surgical treatment of congenital scoliosis associated with tethered cord by thoracic spine-shortening osteotomy without cord detethering. Spine (Phila Pa 1976). 2015. 40: E1103-9
9. Ito M, Abumi K, Kotani Y, Takahata M, Sudo H, Hojo Y. Simultaneous double-rod rotation technique in posterior instrumentation surgery for correction of adolescent idiopathic scoliosis. J Neurosurg Spine. 2010. 12: 293
10. Li Z, Lei F, Xiu P, Yang X, Wang L, Feng G. Surgical treatment for severe and rigid scoliosis: A case-matched study between idiopathic scoliosis and syringomyelia-associated scoliosis. Eur Spine J. 2019. 19: 87-94
11. Matsumoto M, Watanabe K, Tsuji T, Ishii K, Takaishi H, Nakamura M. Progressive kyphoscoliosis associated with tethered cord treated by posterior vertebral column resection: A case report. Spine (Phila Pa 1976). 2009. 34: E965-8
12. Noordeen MH, Taylor BA, Edgar MA. Syringomyelia. A potential risk factor in scoliosis surgery. Spine (Phila Pa 1976). 1994. 19: 1406-9
13. Qiu Y, Zhu F, Wang B, Yu Y, Zhu Z, Qian B. Comparison of surgical outcomes of lenke type 1 idiopathic scoliosis: Vertebral coplanar alignment versus derotation technique. J Spinal Disord Tech. 2011. 24: 492-9
14. Senkoylu A, Cetinkaya M. Correction manoeuvres in the surgical treatment of spinal deformities. EFORT Open Rev. 2017. 2: 135-40
15. Sha S, Qiu Y, Sun W, Han X, Zhu W, Zhu Z. Does surgical correction of right thoracic scoliosis in syringomyelia produce outcomes similar to those in adolescent idiopathic scoliosis?. J Bone Joint Surg Am. 2016. 98: 295-302
16. Singrakhia M, Malewar N, Jangle A. Intraspinal anomalies in early onset scoliosis: Current concepts. J Pediatr Neurosci. 2018. 13: 294-301
17. Sudo H, Ito M, Abe Y, Abumi K, Takahata M, Nagahama K. Surgical treatment of lenke 1 thoracic adolescent idiopathic scoliosis with maintenance of kyphosis using the simultaneous double-rod rotation technique. Spine (Phila Pa 1976). 2014. 39: 1163-9
18. Sun L, Song Y, Liu L, An Y, Zhou C, Zhou Z. Bilateral apical vertebral derotation technique by vertebral column manipulation compared with vertebral coplanar alignment technique in the correction of lenke Type 1 idiopathic scoliosis. BMC Musculoskelet Disord. 2013. 14: 175
19. Tao H, Yang K, Li T, Yang W, Feng C, Li H. Is it possible to correct congenital spinal deformity associated with a tethered cord without prophylactic intradural detethering?. Clin Orthop Relat Res. 2019. 477: 1689-97
20. Tao HR, Yang TL, Chang MS, Li H, Zhang DW, Fan HB. Successful treatment of a patient with congenital kyphoscoliosis associated with tethered cord. J Neurosurg Spine. 2015. 22: 64-9
21. Wang G, Sun J, Jiang Z, Cui X, Cui J. One-stage correction surgery of scoliosis associated with syringomyelia: Is it safe to leave untreated a syrinx without neurological symptom?. J Spinal Disord Tech. 2015. 28: E260-4
22. Winn HR, Youmans JR.editors. Youmans Neurological Surgery. Philadelphia, PA: Saunders; 2011. Ch. 290:
23. Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Yang Z. One-stage and posterior approach for correction of moderate to severe scoliosis in adolescents associated with Chiari I malformation: Is a prior suboccipital decompression always necessary?. Eur Spine J. 2011. 20: 1106-13
24. Yao KC, McGirt MJ, Chaichana KL, Constantini S, Jallo GI. Risk factors for progressive spinal deformity following resection of intramedullary spinal cord tumors in children: An analysis of 161 consecutive cases. J Neurosurg. 2007. 107: 463-8
25. Yasuoka S, Peterson HA, MacCarty CS. Incidence of spinal column deformity after multilevel laminectomy in children and adults. J Neurosurg. 1982. 57: 441-5
26. Zhang BB, Tao HR, Wu TL, Wang L, Duan CG, Zhang T. Safety and efficacy of single-stage surgical treatment for congenital scoliosis associated with intraspinal mass. Sci Rep. 2017. 7: 41229
27. Zhao Q, Shi B, Sun X, Liu Z, Su H, Li Y. Do untreated intraspinal anomalies in congenital scoliosis impact the safety and efficacy of spinal correction surgery? A retrospective case-control study. J Neurosurg Spine. 2019. 31: 40-5