- Department of Medicine and Surgery, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada,
- Department of Neurosurgery, Cairo University, Cairo, Egypt,
- Department of Neurosurgery, Schulich School of Medicine and Dentistry, Western University, London,
- Department of Neurosurgery, Windsor Regional Hospital, Western University, Windsor, Ontario, Canada.
Correspondence Address:
Mohamed A. R. Soliman
Department of Neurosurgery, Windsor Regional Hospital, Western University, Windsor, Ontario, Canada.
DOI:10.25259/SNI_705_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saba Shahab1, Mohamed A. R. Soliman2, Abdullah F. Alkhamees3, Sydney Eaton1, Elise Quint1, Jacob Im1, Avalon O’Connor1, Erika Haberfellner1, Abdalla Shamisa4. Surgical intervention for spontaneous intracranial hypotension Type 4 CSF leak: A case report. 04-Dec-2020;11:421
How to cite this URL: Saba Shahab1, Mohamed A. R. Soliman2, Abdullah F. Alkhamees3, Sydney Eaton1, Elise Quint1, Jacob Im1, Avalon O’Connor1, Erika Haberfellner1, Abdalla Shamisa4. Surgical intervention for spontaneous intracranial hypotension Type 4 CSF leak: A case report. 04-Dec-2020;11:421. Available from: https://surgicalneurologyint.com/surgicalint-articles/10424/
Abstract
Background: Spontaneous intracranial hypotension (SIH) is a rare condition that can be very debilitating. SIH is well understood to be due to a CSF leak, however, identifying the source of the leak is still a challenge. We are presenting a case of Type 4 CSF leak and reviewing the related literature.
Case Description: A 46-year-old female presenting with intractable orthostatic headaches was diagnosed with SIH. She was unable to mobilize due to the severity of her symptoms. MRI scans of the brain and spine did not identify a source of the leak. After failing conservative therapy and multiple epidural blood patches, the patient underwent surgery which resulted in significant improvement in symptoms.
Conclusion: This study has shown that surgical intervention improves symptoms in patients who do not have an identifiable source of CSF leak. Further studies need to be done to fully understand the role of surgery in Type 4 CSF leaks.
Keywords: Spontaneous intracranial hypotension, Surgery, Type 4 CSF leak
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is a rare condition that occurs in about 5 out of 100,000 individuals. It commonly affects middle-aged individuals and tends to occur more frequently in women.[
CASE REPORT
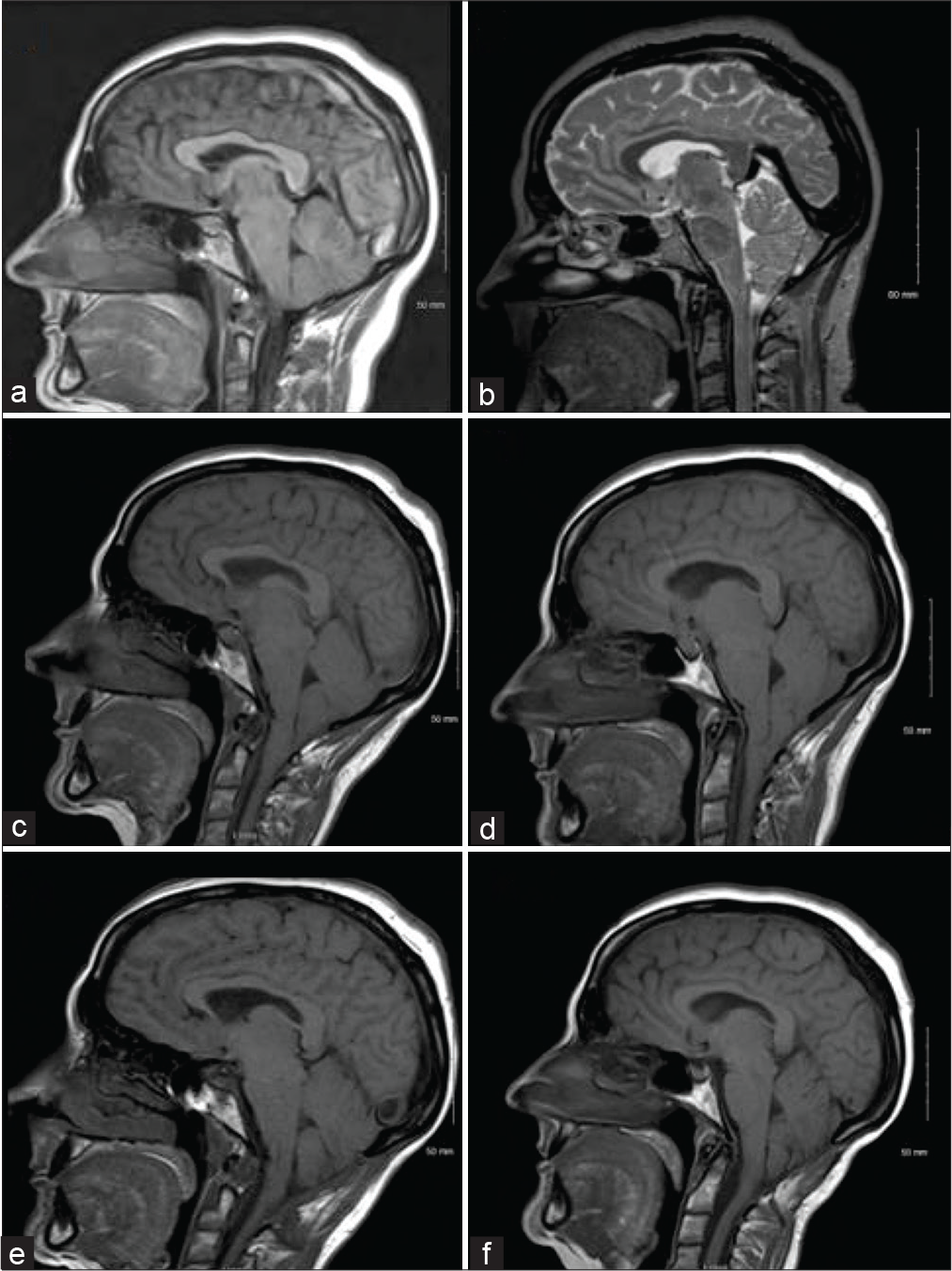
A 46-year-old female presented with severe bifrontal orthostatic headaches with vomiting. She could not continue working due to her symptoms. MRI scan of the brain showed pachymeningeal enhancement and a progressive acquired Chiari malformation in keeping with findings of intracranial hypotension [
Figure 1:
Progression of the cerebellar ectopia. The patient’s symptoms began in September 2007 and posterior fossa decompression was done in June 2012. (a) April 2008, (b) October 2008, (c) December 2011 (showing acquired Chiari malformation, flattening of the pons, and sagging of the cerebellar tonsils slightly below the level of the C1 arch), (d) February 2012, (e) September 5, 2012, (f) December 2014.
Surgical procedures
Posterior fossa decompression
The patient was intubated, her head was held in Sugita pins and she was turned prone on the table. The patient was given preoperative antibiotics. A midline incision was made between the level of C2 and the occiput. The lower part of the occipital bone and the foramen magnum was removed. As the tonsils were going below the C1 level on the MRI, a C1 laminectomy was also conducted. The dura was opened with the arachnoid left intact with no evidence of CSF leak. The lower part of the cerebellar tonsils was seen at the upper edge of the C2 lamina. A duraplasty was done using a piece of fascia lata graft with no attempt to dissect the arachnoid or the tonsils and the incision was closed in layers.
Open thoracic and lumbar blood patching
A midline incision was made over the T11-T12 spinous process. The T11 and T12 spinous process and lamina were exposed in subperiosteal fascial dissection. A laminotomy at the T11-T12 level was done on the patient’s left side. The ligamentum flavum was removed and a 6 French (Fr) pediatric catheter was passed in the epidural space cranially for 20 cm. A laminotomy at the T11-T12 level was also done on the right side with an epidural catheter passed caudally into the lumbar spine for 15 cm. Venous blood was collected from an intravenous line in the patient’s forearm and 10 CCs were injected into the thoracic spine and 8 CCs in the lumbar spine while withdrawing the catheter. The catheters were removed, and the incision was closed in layers.
DISCUSSION
We presented a case where a patient with an unidentifiable CSF leak, debilitating headaches, and intracranial hypotension had significant improvements in symptoms and functional outcome after surgery. We reviewed the PubMed using the search terms “spontaneous intracranial hypotension” and “type 4 CSF leak.” In about 10–30% of patients with SIH, symptoms persist even after repeated epidural blood patches.[
The headaches seen in patients with spontaneous intracranial hypotension are postulated to occur due to low intracranial CSF volume.[
CONCLUSION
The current evidence, including the case presented in this report, shows that surgical intervention can be an effective way to manage SIH in patients who fail to respond to conservative management. Surgery is rarely considered a treatment option for Type 4 CSF leaks. As there is a paucity of case–control studies, cohort studies, and randomized controlled trials on this topic, the current level of evidence is weak and is only based on case series and case reports. Thus, further studies need to be conducted to fully understand the efficacy of targeted blood patches for clinical improvement in SIH with an unknown etiology of CSF leak, and to date, the management of these types of CSF leaks should be individualized to try to obtain the best patients’ outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beck J, Häni L, Ulrich CT, Fung C, Jesse CM, Piechowiak E. Diagnostic challenges and therapeutic possibilities in spontaneous intracranial hypotension. Clin Transl Neurosci. 2018. 2: 1-11
2. Chan SM, Chodakiewitz YG, Maya MM, Schievink WI, Moser FG. Intracranial hypotension and cerebrospinal fluid leak. Neuroimaging Clin N Am. 2019. 29: 213-26
3. Cho KI, Moon HS, Jeon HJ, Park K, Kong DS. Spontaneous intracranial hypotension: Efficacy of radiologic targeting vs blind blood patch. Neurology. 2011. 76: 1139-44
4. Davenport RJ, Chataway SJ, Warlow CP. Spontaneous intracranial hypotension from a CSF leak in a patient with Marfan’s syndrome. J Neurol Neurosurg Psychiatry. 1995. 59: 516-9
5. Davidson B, Nassiri F, Mansouri A, Badhiwala JH, Witiw CD, Shamji MF. Spontaneous intracranial hypotension: A review and introduction of an algorithm for management. World Neurosurg. 2017. 101: 343-9
6. Feltracco P, Galligioni H, Barbieri S, Ori C. Thoracic epidural blood patches in the treatment of spontaneous intracranial hypotension: A retrospective case series. Pain Physician. 2015. 18: 343-8
7. Inenaga C, Tanaka T, Sakai N, Nishizawa S. Diagnostic and surgical strategies for intractable spontaneous intracranial hypotension, Case report. J Neurosurg. 2001. 94: 642-5
8. Rettenmaier LA, Park BJ, Holland MT, Hamade YJ, Garg S, Rastogi R. Value of targeted epidural blood patch and management of subdural hematoma in spontaneous intracranial hypotension: Case report and review of the literature. World Neurosurg. 2017. 97: 27-38
9. Riley DS, Barber MS, Kienle GS, Aronson JK, von SchoenAngerer T, Tugwell P. CARE guidelines for case reports: Explanation and elaboration document. J Clin Epidemiol. 2017. 89: 218-35
10. Schievink WI, Maya MM, Jean-Pierre S, Nuño M, Prasad RS, Moser FG. A classification system of spontaneous spinal CSF leaks. Neurology. 2016. 87: 673-9
11. Schievink WI, Morreale VM, Atkinson JL, Meyer FB, Piepgras DG, Ebersold MJ. Surgical treatment of spontaneous spinal cerebrospinal fluid leaks. J Neurosurg. 1998. 88: 243-6
12. Schievink WI, Reimer R, Folger WN. Surgical treatment of spontaneous intracranial hypotension associated with a spinal arachnoid diverticulum, Case report. J Neurosurg. 1994. 80: 736-9
13. Schievink WI. A novel technique for treatment of intractable spontaneous intracranial hypotension: Lumbar dural reduction surgery. Headache. 2009. 49: 1047-51
14. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006. 295: 2286-96