- Department of Neurosurgery, Baylor Scott and White, Temple, Texas, United States
- Department of Neurological Surgery, Baylor Scott and White, Temple, Texas, United States.
Correspondence Address:
William Trent Richardson, Department of Neurosurgery, Baylor Scott and White, Temple, Texas, United States.
DOI:10.25259/SNI_475_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: William Trent Richardson1, Lokeshwar Sai Santosh Bhenderu2, Jose M. Soto2, David Garrett2. Surgical management of an ossified giant lumbar pseudomeningocele: A case report. 14-Jul-2023;14:244
How to cite this URL: William Trent Richardson1, Lokeshwar Sai Santosh Bhenderu2, Jose M. Soto2, David Garrett2. Surgical management of an ossified giant lumbar pseudomeningocele: A case report. 14-Jul-2023;14:244. Available from: https://surgicalneurologyint.com/surgicalint-articles/12429/
Abstract
Background: Pseudomeningoceles (PMs) are infrequent complications of spine surgery resulting from incidental durotomy and subsequent extravasation of cerebrospinal fluid. Giant PMs (GPMs), defined as ≥8 cm in major diameter, are rarely reported in the literature and present a challenge due to a lack of clear guidelines for surgical management.
Case Description: Here, the authors discuss the successful surgical management of a 25.3 cm lumbar GPM that became calcified 3 years following an initial T10-S2 laminectomy with instrumented fusion performed at an outside-hospital.
Conclusion: This report focuses on the successful 3-year delayed surgical intervention for the management of an ossified GPM.
Keywords: Durotomy, Giant, Ossification, Pseudomeningocele
INTRODUCTION
Pseudomeningocele (PM) is an uncommon complication of spine surgery (0.07–2%) attributed to an iatrogenic durotomy that results in the extradural accumulation of cerebrospinal fluid (CSF).[
CASE SUMMARY
History
A 76-year-old Caucasian male presented with chronic back pain following a T10-S2 laminectomy with instrumentation and L6-S1 fusion performed at outside-hospital 3 years ago. Notably, the PM was noted soon after surgery, but no surgery was performed. The patient complained of worsening “positional” back pain and a “clicking” sensation while walking, accompanied by the right lower extremity radiculopathy (paresthesias in right foot) but with an intact neurological examination.
Diagnostic electromyographies (EMGs) and magnetic resonance (MR) studies
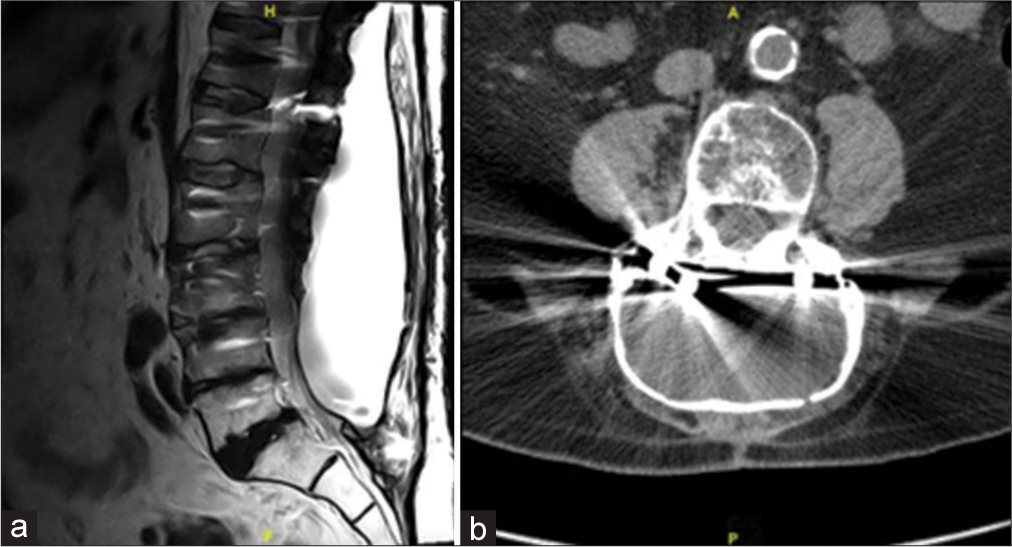
The EMGs showed bilateral denervation in the L3/L4 nerve root distributions, while MR/computed tomography studies showed a large posterior fluid collection with calcified margins [
Surgery and postoperative outcome
Through a midline lumbar incision, a large calcified cystic mass was encountered that drained clear yellow fluid. There was marked calcification encompassing the instrumentation that was previously placed T10-S2; notably, the rods at L4-5 had hairline fractures without displacement. All instrumentation was removed. An extensive calcified membrane covered the prior laminectomy site from T11 to L4; while from L5 – distally, a thick fibrous scar covered the dura. Finally, the thoracolumbar sacral fascia was reapproximated with interrupted 0 Vicryl sutures followed by superficial layer closures using inverted vertical mattress 2-0 Vicryl and 3-0 Vicryl sutures; the skin was approximated with stainless steel clips. Postoperatively, the patient was neurologically intact within 135 days; his pain was well-controlled (i.e., without paresthesias), he had no residual motor deficit, and radiographically, PM did not reaccumulate [
DISCUSSION
Incidental durotomy is one of the most common complications of spine surgery, (3–5% in primary 7–17% in revision surgery). PM may develop postoperatively due to the continued accumulation of CSF in the extrathecal space; some may spontaneously resolve, while others continue to accumulate CSF potentially resulting in GPM.
Calcification of PMs is a rarely reported event, reportedly occurring up to 10.3 years after surgery.[
CONCLUSION
Here, a 76-year-old male underwent successful repair of a 25.3 cm lumbar GPM that developed and ossified following a T11-L4 laminectomy with instrumented fusion 3 years prior.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akhaddar A, Boulahroud O, Boucetta M. Nerve root herniation into a calcified pseudomeningocele after lumbar laminectomy. Spine J. 2012. 12: 273
2. Couture D, Branch CL. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003. 15: E6
3. Enke O, Dannaway J, Tait M, New CH. Giant lumbar pseudomeningocele after revision lumbar laminectomy: A case report and review of the literature. Spinal Cord Ser Cases. 2018. 4: 82
4. Goel A. Ossified pseudomeningocele. J Neurosurg Pediatr. 2009. 3: 79
5. Narverud SF, Ramli NB, Chandran H, Ganesan D. Calcified pseudomeningocele of the lumbar spine: A review. Eur Spine J. 2013. 22: S443-9
6. Ruggiero C, Barbato M, Spennato P, Russo C, Cicala D, Cinalli G. Repair of giant lumbosacral pseudomeningocele with fast-resorbing polymer mesh in a pediatric patient operated for posterior dysraphism. Childs Nerv Syst. 2020. 36: 1777-80
7. Shifrin LZ, Frish E, Ben-Arie J. Postsurgical lumbar calcified extradural cyst. Report of a case. Spine (Phila Pa 1976). 1990. 15: 229-31
8. Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010. 11: 53