- Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Correspondence Address:
Md Rezaul Amin, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
DOI:10.25259/SNI_731_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Md Rezaul Amin, Md Tauhidur Rahman, A. B. M. Manwar Hossain, Tahsina Quader, KM Tarikul Islam. Surgical management of craniocervical junction tuberculosis with atlanto-axial dislocation – A case report and review of the literature. 06-Oct-2023;14:359
How to cite this URL: Md Rezaul Amin, Md Tauhidur Rahman, A. B. M. Manwar Hossain, Tahsina Quader, KM Tarikul Islam. Surgical management of craniocervical junction tuberculosis with atlanto-axial dislocation – A case report and review of the literature. 06-Oct-2023;14:359. Available from: https://surgicalneurologyint.com/surgicalint-articles/12577/
Abstract
Background: There are few guidelines on how to best manage craniovertebral junction (CVJ) tuberculosis (TB). Certainly, timely tissue diagnosis, immobilization of the neck, and decompression of CVJ with appropriate stabilization are the mainstays of treatment for TB at the CVJ.
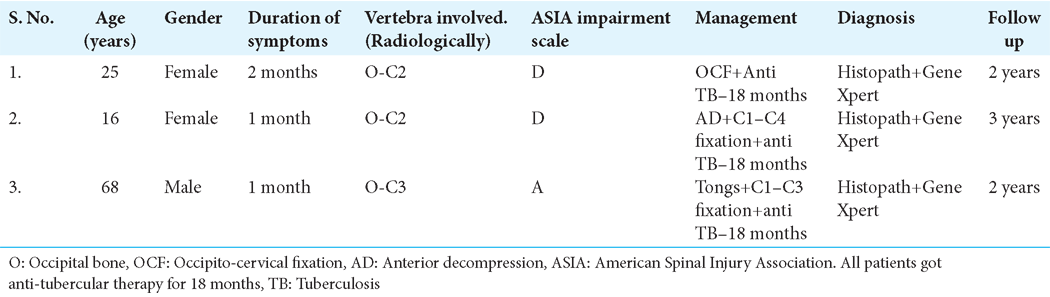
Case Description: Three patients, ages 16–68, presented with CVJ TB with atlanto-axial dislocation responsible for progressive quadriparesis/plegia. Based on X-rays, magnetic resonance, and computed tomography studies, patients underwent timely decompressions and fusions followed by antitubercular drug treatment.
Conclusion: Early diagnosis, proper decompression with fusion, treated with anti-TB drug for proper period were keys to managing TB involving the craniocervical junction in these three patients.
Keywords: Anti-tubercular therapy, Atlanto-axial dislocation, Craniovertebral junction, Kyphotic deformity, Tuberculosis
INTRODUCTION
The incidence of tuberculosis (TB) in the spine is <1%.[
CASE 1
History and presentation
A 25-year-old Asian male presented with 2 months of severe neck pain (i.e., focally tender on exam), a progressive bilateral quadriparesis; 3/4 bilateral motor function, bilateral diffuse hyperreflexia/Hoffman’s Signs, Babinski responses, and a definite C2 sensory level (American Spinal Injury Association, ASIA D). Cervical X-rays showed an osteolytic C1 lesion with instability of the Atlanto-Axial dislocation (AAD). The magnetic resonance imaging (MRI) confirmed CVJ instability while also demonstrating a pre-vertebral collection contributing to marked anterior cord compression [
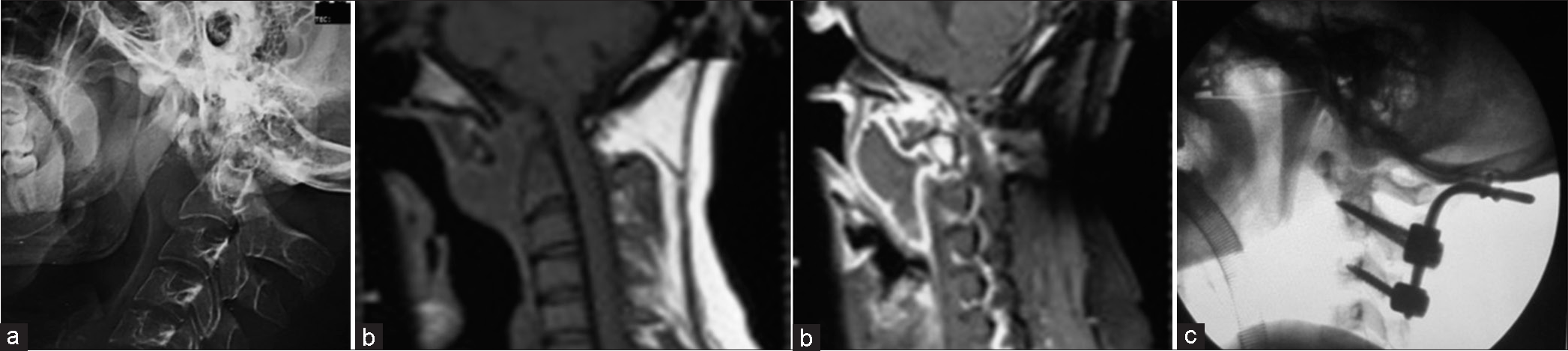
Figure 1:
(a) X-ray cervical spine lateral view showing increased atlanto dental interval (13 mm) with radio dense shadow in between. (b) Magnetic resonance imaging cervical spine in sagittal T1-weighted image and contrast showing prevertebral retro-oropharyngeal abscess. (c) Immediate postoperative cervical X-ray days showed beautiful correction.
Surgery
Prone skeletal tong traction corrected the AAD (Atlanto-Axial-Dens) malalignment. At surgery, following the occiput to C2 exposure, the C1 lateral masses were clearly eroded. With minimal distraction, pus immediately extruded from the prevertebral space; it was washed and followed by an occipito-cervical fusion (i.e., including the use of C2/C3 lateral mass screws). He wore a rigid cervical collar for 1 month, followed by a soft collar for 2 months. Within 2 postoperative weeks, he could walk independently, and at 2 postoperative months was neurologically intact.
CASE 2
History and presentation
A 16-year-old female presented with severe neck pain for 1-month, low grade fever, and 2 weeks of progressive spastic quadriparesis (motor 4/5) with sensory loss to pin from C2 to C4 (ASIA D). The cervical X-rays and computed tomography (CT) scan showed an osteolytic C2 lesion (i.e., involving the C2 body and pedicle) with kyphosis and Atlano-Axial instability. The MRI showed an extradural mass anterior to C1/2 compressing the cord spinal cord; it extended into the retropharyngeal space [
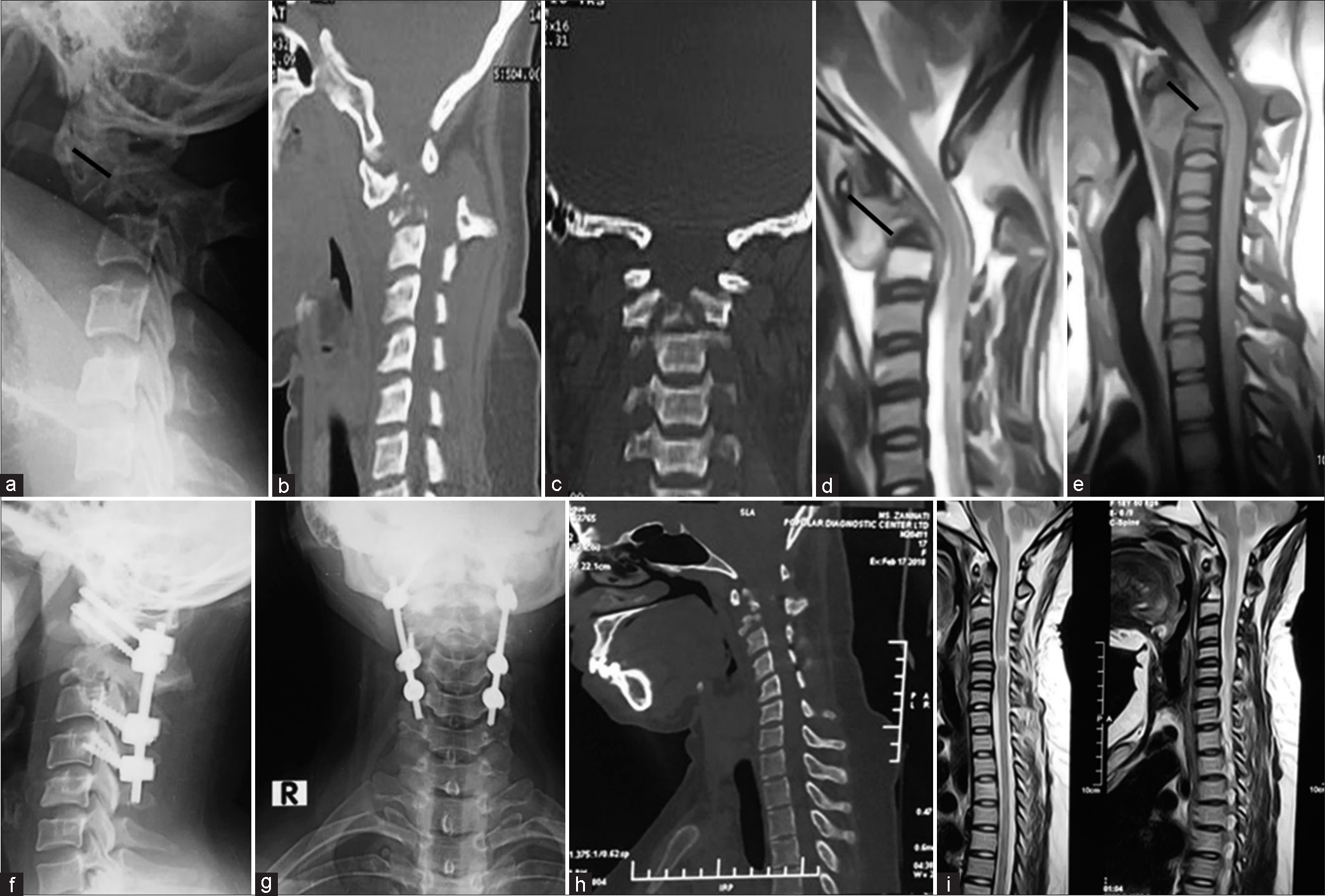
Figure 2:
(a) X-ray cervical spine lateral view showing increased atlanto dental interval (16 mm) with radio dense shadow in between, (b and c) computed tomography (CT) cervical spine lateral (b), coronal (c) view showing osteolytic lesion at C2 body. (d and e) Magnetic resonance imaging (MRI) cervical spine in sagittal T2-weighted image (T2WI) (d) and T1-weighted image (e) showing prevertebral retrooropharyngeal abscess. (f and g) Postoperative cervical X-ray after 15 days, (h) CT cervical spine sagittal after 1 month, and (i) MRI of the cervical spine in sagittal T2WI after 3 months showed complete resolution of abscess, correction of kyphotic deformity.
Surgery
Surgery was performed in two stages. The first was transoral decompression; the second was posterior stabilization [
CASE 3
History and presentation
A 68-year-old male presented with severe neck pain for 1 month, respiratory distress, quadriplegia/sphincter dysfunction, a C2 complete sensory level, and bladder-bowel dysfunction (ASIA A). After immediate placement in skeletal (tong) traction, his motor exam improved to the 2/5 level. Cervical X-rays of the CVJ confirmed atlanto-axial instability. The MRI revealed destructive changes involving the C2 and C3 intervertebral discs/vertebral bodies along with an extradural anterior C1–C3 retropharyngeal collection that markedly compressed the cord. The CT confirmed the destruction of dens [
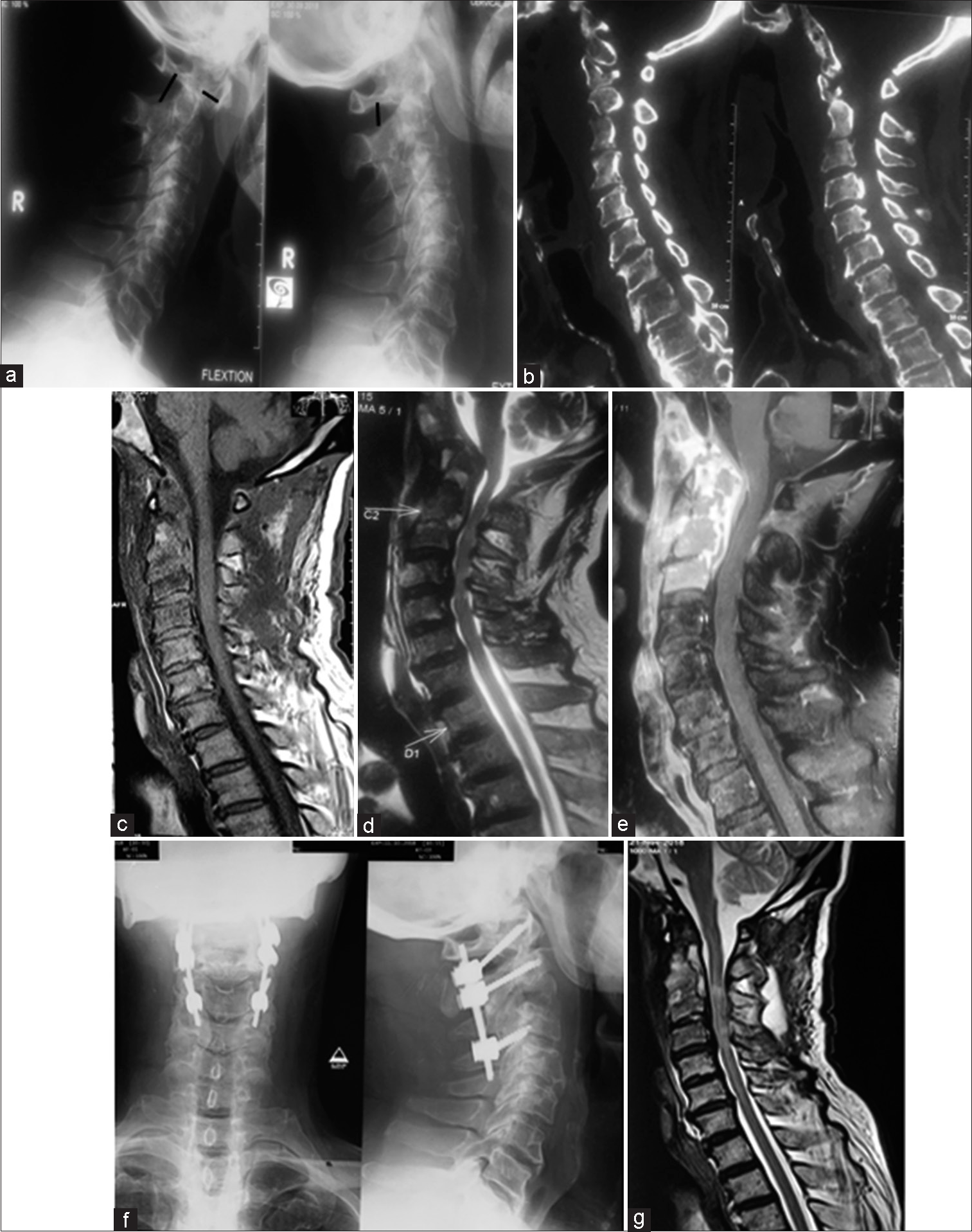
Figure 3:
X-ray cervical spine dynamic view showing C1/2 instability, (b) Computed tomography (CT) cervical spine in sagittal view, showing partial erosion of C1 lateral mass and C2 body, (c, d, e) Magnetic resonance imaging (MRI) of the cervical spine, contrast enhancing extradural mass at C1–3 levels causing obliteration of the anterior CSF column and prevertebral collection of abscesses. (f) Postoperative X-ray of the cervical spine at 1 month, showing spinal fixation between C1 lateral mass, C2 pedicle, and C3 lateral mass with screws and rods, (g) MRI of the cervical spine at 6-month complete resolution of abscess and significant decompression of cord.
Surgery
After 2 days of skeletal (tong) traction, through a midline posterior occiput-C2 incision, the C1/2 lateral joint space was identified and pus was spilling out from it anteriorly. Granulation tissue was debrided lateral to the C2, and C3 lateral masses. The screw was placed from C1 to C3. Postoperatively, the treatment with a collar for 3 months, the antibiotic regimen, the diagnostic studies, and the postoperative lab studies were all similar than the prior cases [
Histopathology and antibiotic treatment
Histopathology showed granulomatous inflammation suggestive of TB. The GeneXpert (A cartridge based nucleic acid amplification test rapid diagnostic test for TB detection as well as Rifampicin resistance in direct smear negative cases) was positive for TB. The patient was given 18 months of anti-tubercular therapy; 3 months of 4 drugs followed by 15 months of 2 drugs. He was also given, pyridoxine tablets for 18 months.
Neurodiagnostic follow-up
X-rays were done on postoperative days 1, 7, and 15 and every month thereafter looking for progressive infection/deformity, and/or pseudarthrosis [
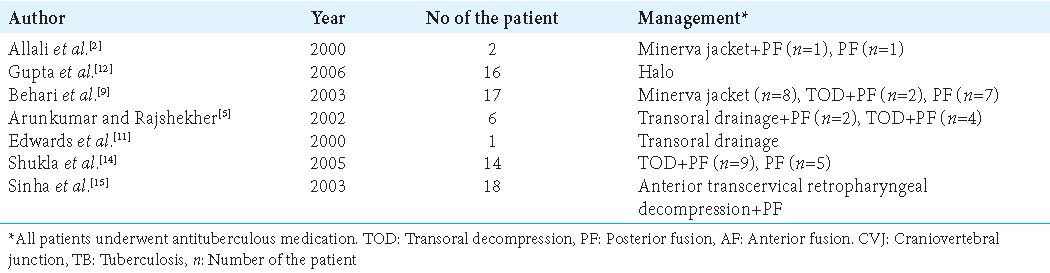
DISCUSSION
Spinal TB rarely involves the cervical spine (i.e., 3–5%) and even more infrequently occurs at the CVJ.[
CONCLUSION
In three patients with TB at the CVJ patients underwent early diagnosis (X-rays, MR, and CT) and surgical decompressions/ fusions to prevent further neurological deterioration and offer the potential for neurological recovery.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akhaddar A, Chakir N, El Hassani MY, El Quessar A, Jiddane M, Boukhrissi N. Sub-occipital Pott’s disease. Diagnostic imaging in 2 cases. J Neuroradiol. 2000. 27: 144-9
2. Allali N, El-Quessar A, Melhaoui A, El-Hassani MR, Chakir N, Jiddane M. Sub occipital Pott’s disease: Report of 8 cases. J Neuroradiol. 2004. 31: 72-3
3. Allali F, Benomar A, El Yahyaoui M, Chkili T, Hajjaj-Hassouni N. Atlantoaxial tuberculosis: Three cases. Joint Bone Spine. 2000. 67: 481-4
4. Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK. The results of nonoperative treatment of craniovertebral junction tuberculosis: A review of twenty-six cases. J Bone Joint Surg Am. 2011. 93: 540-7
5. Arunkumar MJ, Rajshekhar V. Outcome in neurologically impaired patients with craniovertebral junction tuberculosis: Results of combined anteroposterior surgery. J Neurosurg. 2002. 97: 166-71
6. Augier A, Zrig H, Roqueplan F, Brauner M, Dumas JL. MR and CT features of craniocervical junction tuberculosis: A report of 5 cases. J Radiol. 2008. 89: 585-9
7. Bapat MR, Lahiri VJ, Harshavardhan NS, Metkar US, Chaudhary KC. Role of transarticular screw fixation in tuberculous atlanto-axial instability. Eur Spine J. 2007. 16: 187-97
8. Belanger E, Levi AD. Tuberculosis of the axis in a patient with systemic sarcoidosis: Technique of posterior open biopsy of the dens: Case report. Neurosurgery. 2000. 47: 969-72
9. Behari S, Nayak SR, Bhargava V, Banerji D, Chhabra DK, Jain VK. Craniocervical tuberculosis: Protocol of surgical management. Neurosurgery. 2003. 53: 1010
10. Dhaon BK, Jaiswal A, Nigam V, Jain V. Atlantoaxial rotatory fixation secondary to tuberculosis of occiput: A case report. Spine (Phila Pa 1976). 2003. 28: E203-5
11. Edwards RJ, David KM, Crockard HA. Management of tuberculomas of the craniovertebral junction. Br J Neurosurg. 2000. 14: 19-22
12. Gupta SK, Mohindra S, Sharma BS, Gupta R, Chhabra R, Mukherjee KK. Tuberculosis of the craniovertebral junction: Is surgery necessary?. Neurosurgery. 2006. 58: 1144-50
13. Mohindra S, Gupta SK, Mohindra S, Gupta R. Unusual presentations of craniovertebral junction tuberculosis: A report of 2 cases and literature review. Surg Neurol. 2006. 66: 94-9
14. Shukla D, Mongia S, Devi BI, Chandramouli BA, Das BS. Management of craniovertebral junction tuberculosis. Surg Neurol. 2005. 63: 101-6
15. Sinha S, Singh AK, Gupta V, Singh D, Takayasu M, Yoshida J. Surgical management and outcome of tuberculous atlantoaxial dislocation: A 15-year experience. Neurosurgery. 2003. 52: 331-8