- Department of Neurosurgery, Mohamed V Military Training Hospital, Mohammed V Faculty of Medicine and Pharmacy, Rabat, Morocco.
Correspondence Address:
Fresnel Lutèce Ontsi Obame, Department of Neurosurgery, Mohamed V Military Training Hospital, Mohammed V Faculty of Medicine and Pharmacy, Rabat, Morocco.
DOI:10.25259/SNI_667_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fresnel Lutèce Ontsi Obame, Yao Christian Hugues Dokponou, Salami Mohcine, Saad Moussa Elmi, Napoleao Imbunhe, Inas El Kacemi, Mohamed Mouhssani, Imad-Eddine Sahri, Housni Abderrahmane, Jawad Laaguili, Abad Chérif El Asri, Miloudi Gazzaz. Surgical outcome and prognostic factors for 39 recurrent spinal hydatid cysts. 29-Sep-2023;14:347
How to cite this URL: Fresnel Lutèce Ontsi Obame, Yao Christian Hugues Dokponou, Salami Mohcine, Saad Moussa Elmi, Napoleao Imbunhe, Inas El Kacemi, Mohamed Mouhssani, Imad-Eddine Sahri, Housni Abderrahmane, Jawad Laaguili, Abad Chérif El Asri, Miloudi Gazzaz. Surgical outcome and prognostic factors for 39 recurrent spinal hydatid cysts. 29-Sep-2023;14:347. Available from: https://surgicalneurologyint.com/surgicalint-articles/12574/
Abstract
Background: Cystic bone echinococcosis accounts for 0.5–4% of all reported cases, and 45% occur in the spine. Our aim was to review the clinical and radiological features, surgery, and outcomes for 39 patients with recurrent spinal hydatidosis.
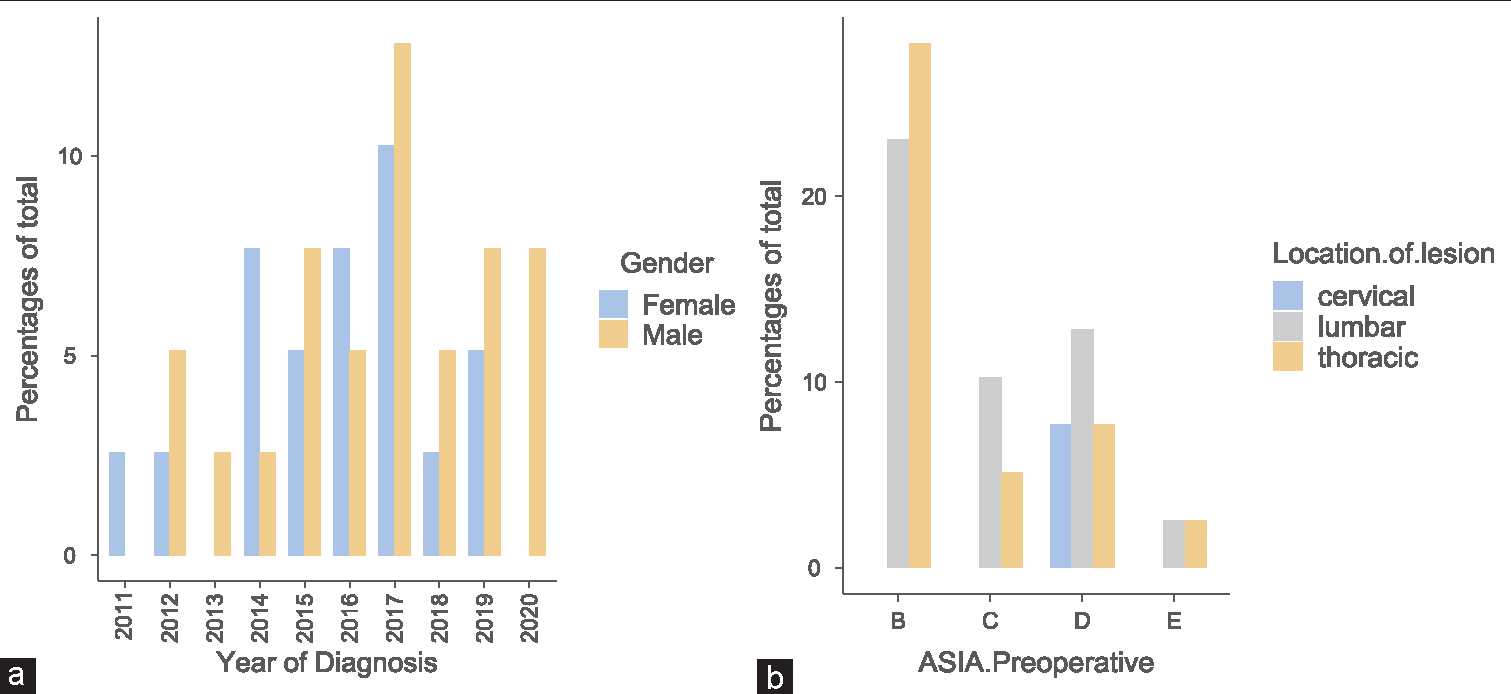
Methods: Thirty-nine reports of patients with recurrent spinal hydatidosis (2011–2020) were followed for an average of 9.28 ± 5.60 months.
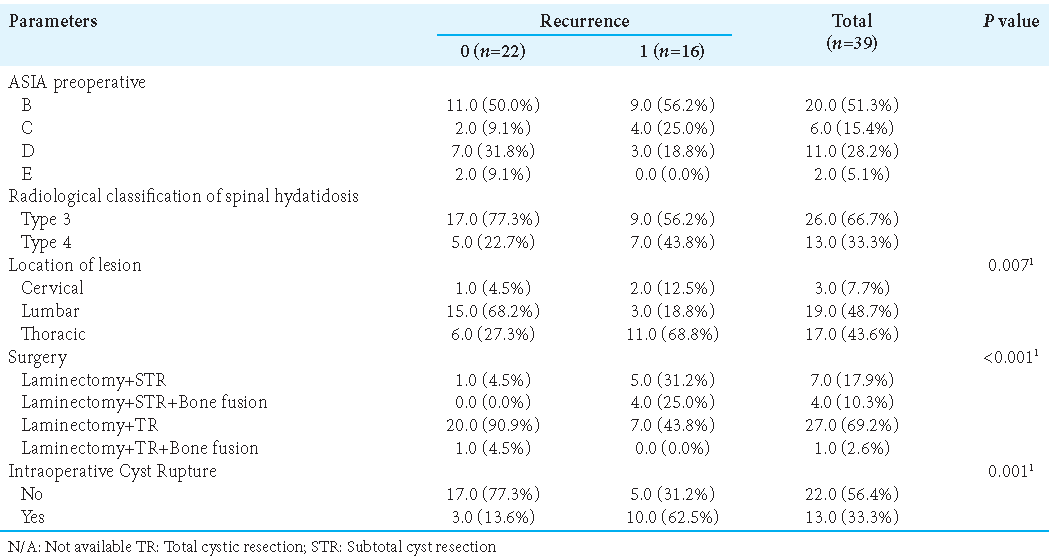
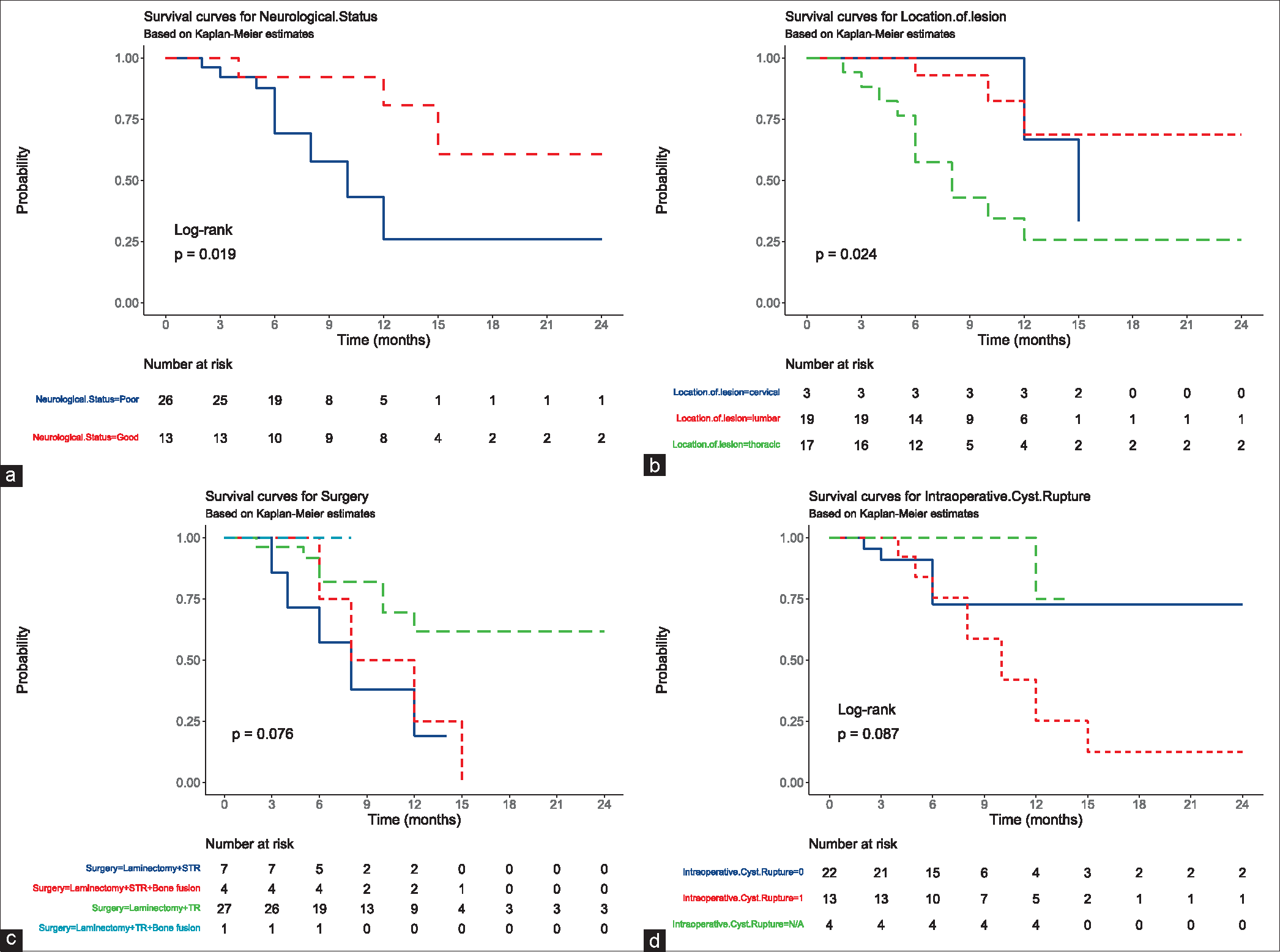
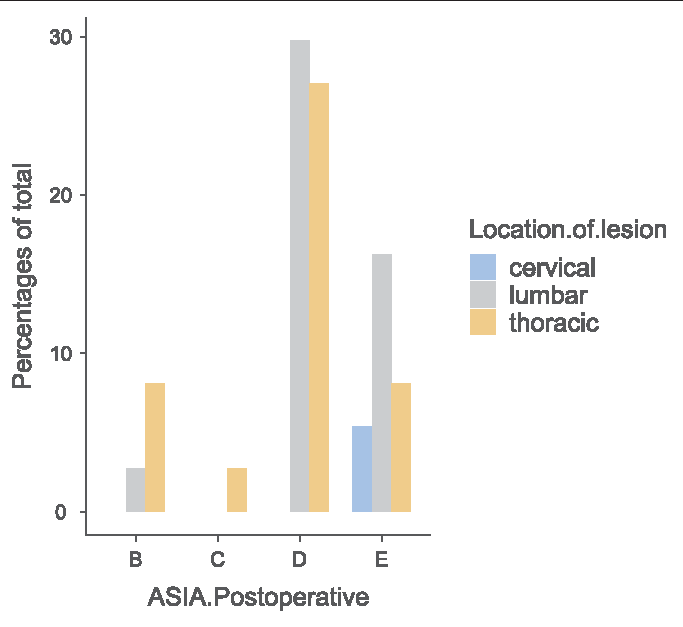
Results: Lesions occurred in descending order in the; lumbar (48.7%), thoracic (43.6%), and cervical spine (7.7%). Total cyst resection was achieved in 28 of 39 patients (71.8%). Intraoperative cyst rupture occurred in 13 patients (33.3%). The postoperative American Spinal Injury Association (ASIA) score was “good” in 82% of patients. Those with “poor” postoperative ASIA scores had a 41% incidence of recurrent thoracic hydatid cysts; further, they demonstrated significantly higher recurrence rates if cysts had ruptured intraoperatively (P = 0.001). In addition, laminectomy, subtotal original cyst resection (P P
Conclusion: The majority of patients demonstrated improvement following surgery for cervical hydatid cysts. Notably, those with poor outcomes typically experienced intraoperative ruptures of their thoracic hydatid cysts, contributing to high cyst recurrence rates.
Keywords: Outcome, Prognostic factors, Recurrence, Spinal hydatidosis
INTRODUCTION
Cystic echinococcosis (hydatidosis) is a parasitic disease caused by Echinococcus granulosus. Cystic bone echinococcosis accounts for 0.5–4% of all reported cases and 45% occur in the spine.[
MATERIALS AND METHODS
Ethics approval
This retrospective study involved anonymous data collection, and consent was not required.
Study population
We retrospectively reviewed the hospital records (clinical, radiological, and surgical) of 39 patients with spinal hydatidosis over a 10-year period (2011–2020). The study only included patients undergoing surgery for spinal hydatidosis along with reporting all patients with symptomatic recurrences warranting reoperations.
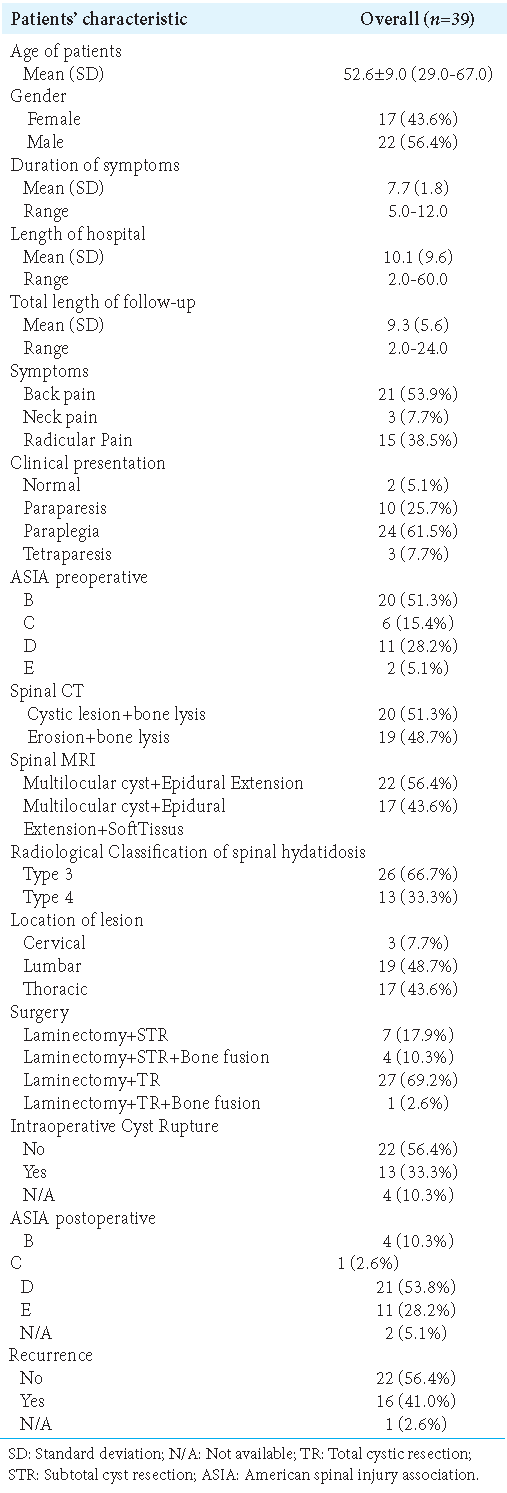
Patients’ preoperative clinical characteristics including ASIA scores
Over 10 years, 39 patients with spinal hydatidosis had surgery [
Utilization of MR/CT studies
Preoperative MR/CT studies
Patients underwent cervical, thoracic, or lumbar MR/CT studies to document the location and extent of their spinal hydatidosis. Most lesions involved the lumbar (48.7%), followed by the thoracic (43.6%) and cervical spine (7.7%). Typically, on MR, lesions consisted of multiloculated cysts extending into epidural soft tissues, while on CT scans, they presented with vertebral lysis and/or erosive bony defects. Cyst locations were most frequently type 3 (i.e., intraspinal extradural hydatid cyst in 66.7% of cases) [
Postoperative MR studies
Postoperatively, patients underwent immediate and 1-month postoperative enhanced MR scans to confirm total resection (TR) or subtotal cyst resection (STR). Patients were additionally followed with contrast MR studies on a yearly basis for early detection of recurrent lesions.
Surgery
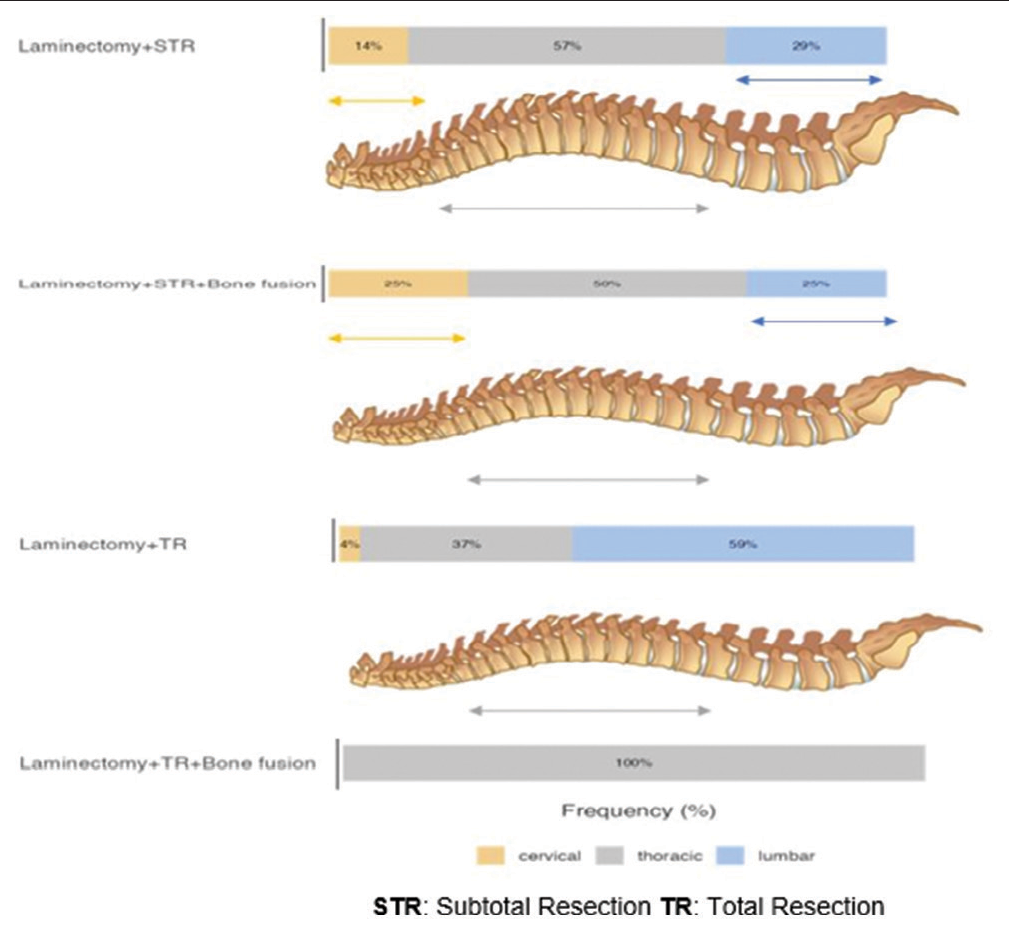
Patients all underwent decompressive laminectomies, supplemented selectively with instrumentation (i.e., where at least two levels were involved or with evidence of vertebral body damage and/or instability).
Neurological follow-up
Neurological assessments were routinely performed preoperatively and postoperatively (i.e., last day of hospitalization, and 3, 6, 12, and 24 months postoperatively). The times between the first surgery and the first recurrence were also recorded.
Statistical analysis
Clinical and radiographic parameters were additionally analyzed using univariate analysis of preoperative and postoperative ASIA scores. Chi-square tests or Fisher’s exact tests were used to analyze categorical variables, along with the t-test (i.e., for evaluation of continuous and ordinal variables). Survival was analyzed used the Kaplan– Meier method (i.e., to identify potential risk factors for recurrence).
RESULTS
Surgery
Following decompressive laminectomies, TR was achieved in 28 cyst cases (71.8%) and STR in 11 cases (28.2%) [
Intraoperative cyst rupture: A major risk factor for cyst recurrence
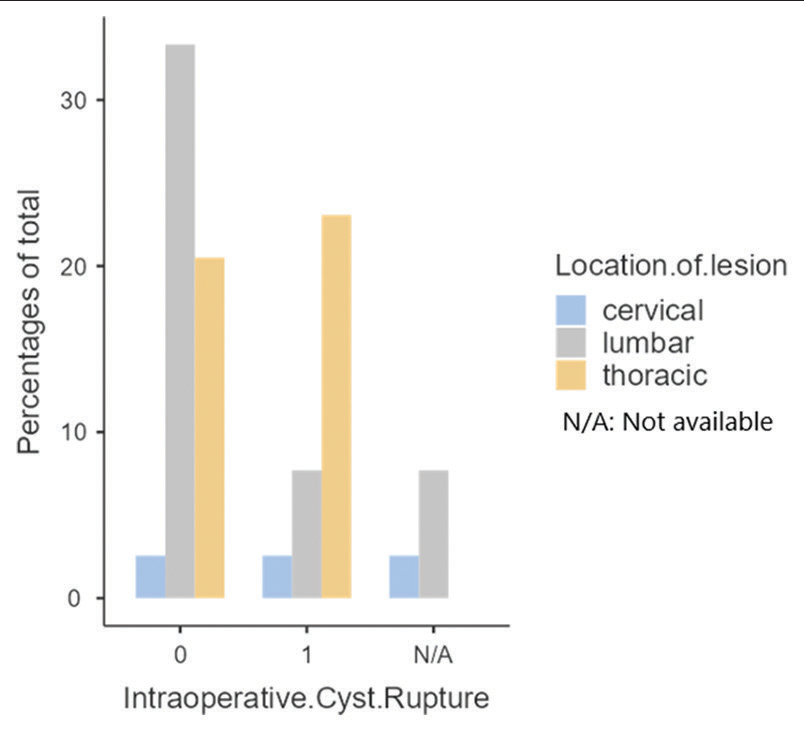
Nine occurred in the thoracic spine [
After a mean interval of 12.8 postoperative months (range: 6–24 months), 16 patients (41%) experienced cyst recurrences. In 76.9% (10/13 cases) of cases, there had been an accidental intraoperative cyst rupture during the index procedure (i.e., swabs soaked in hypertonic saline were utilized to minimize leakage in these 13 cases), while 22.7% occurred without a history of a ruptured cyst (5/22 cases) [
No recurrent postoperative cerebrospinal fluid (CSF) leaks
No patients exhibited persistent postoperative Cerebrospinal fluid (CSF) leaks.
Outcomes
Postoperatively, the majority of patients were neurologically improved; the ASIA scores were “good” in 82% and “poor” in 12.9% [
DISCUSSION
Surgical management of spinal hydatid cysts
In our series of 39 patients, all underwent debridement and laminectomy to resect spinal hydatid cysts, while just five warranted additional fusions.[
Recurrence rates for spinal hydatid cysts
Despite surgical advances and the use of chemotherapy, high recurrence rates remain one of the greatest challenges in treating spinal hydatid cysts.[
Outcomes
We found no mortalities or serious postoperative adverse events in our series. Further, we observed “good outcomes” with ASIA D-E scores in 82% of cases. Ursini et al. reported similar postoperative improvement in their study.[
CONCLUSION
The three main factors contributing to high recurrence rates for spinal hydatidosis cysts and poor neurological outcomes included; (1) a thoracic location of the cyst, (2) subtotal rather than TR, and (3) a history of intraoperative cyst rupture during the index surgery (ASIA A-B-C).
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akhaddar A, Boucetta M. A new surgical technique for the removal of extensive spinal epidural hydatid cyst. Surg Neurol Int. 2018. 9: 96
2. Fiori R, Coco I, Nezzo M, Kabunda G, Umana GE, Fraioli MF. Spinal hydatidosis relapse: A case report. Case Rep Orthop. 2014. 2014: 207643
3. Manenti G, Censi M, Pizzicannella G, Pucci N, Pitocchi F, Calcagni A. Vertebral hydatid cyst infection. A case report. Radiol Case Rep. 2020. 15: 523-7
4. Mansfield BS, Pieton K, Pather S. Spinal cystic echinococcosis. Am J Trop Med Hyg. 2019. 100: 9-10
5. Neumayr A, Tamarozzi F, Goblirsch S, Blum J, Brunetti E. Spinal cystic echinococcosis-a systematic analysis and review of the literature: Part 1. Epidemiology and anatomy. PLoS Negl Trop Dis. 2013. 7: e2450
6. Schnepper GD, Johnson WD. Recurrent spinal hydatidosis in North America. Case report and review of the literature. Neurosurg Focus. 2004. 17: E8
7. Trifa A, Maamri K. Aggressive behavior and recurrent spinal hydatid cyst. Pan Afr Med J. 2021. 40: 202
8. Ursini T, Rodari P, Badona Monteiro G, Barresi V, Cicciò C, Moscolo F. Large multicystic spinal lesion in a young African migrant: A problem of differential diagnosis. BMJ Case Rep. 2021. 14: e242690
9. Velasco-Tirado V, Romero-Alegría Á, Belhassen-García M, Alonso-Sardón M, Esteban-Velasco C, López-Bernús A. Recurrence of cystic echinococcosis in an endemic area: A retrospective study. BMC Infect Dis. 2017. 17: 455
10. Zhang T, Ma LH, Liu H, Li SK. Incurable and refractory spinal cystic echinococcosis: A case report. World J Clin Cases. 2021. 9: 10337-44