- Department of Neurosurgery, University of Texas Health Science Center Houston, Houston, Texas, United States.
DOI:10.25259/SNI_209_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryan Michael McCormack, Amber Y. Chen, Lindsey M. Schwartz, Cole T. Lewis, Ryan S. Kitagawa. Surgical resection of a large posttraumatic middle meningeal artery pseudoaneurysm with associated epidural hematoma. 05-Jan-2021;12:1
How to cite this URL: Ryan Michael McCormack, Amber Y. Chen, Lindsey M. Schwartz, Cole T. Lewis, Ryan S. Kitagawa. Surgical resection of a large posttraumatic middle meningeal artery pseudoaneurysm with associated epidural hematoma. 05-Jan-2021;12:1. Available from: https://surgicalneurologyint.com/surgicalint-articles/10515/
Abstract
Background: Middle meningeal artery (MMA) pseudoaneurysms are rare but can occur secondary to trauma with an associated skull fracture and can present with a variety of hemorrhage patterns. Epidural, subdural, subarachnoid, and intraparenchymal hematomas have all been reported. Given the wide range of clinical presentations and radiographic findings, multiple treatment strategies have been employed, including surgical removal, endovascular intervention, and conservative treatment. MMA pseudoaneurysms typically range from 2 to 5 mm in size and have been shown to have unpredictable growth patterns.
Case Description: A 54-year-old male identifying as a Jehovah’s Witness presented after a fall and was found to have an epidural hematoma with an accompanying temporal bone fracture. Imaging demonstrated a traumatic pseudoaneurysm of the MMA. Given the patient’s religious preferences, the emphasis was made during surgical planning for the minimization of blood loss. The epidural hematoma was evacuated, and the MMA pseudoaneurysm was directly visualized and surgically excised after ligation of its tributaries. The patient tolerated the procedure well without significant blood loss and made a complete neurological recovery.
Conclusion: A well-circumscribed hypodensity on CT within a surrounding hyperintense collection should raise suspicion of MMA pseudoaneurysm in the setting of overlying temporal bone fracture as supported by previous imaging findings of large MMA pseudoaneurysms. The early detection of MMA pseudoaneurysm is imperative, as the presence may dictate more urgent intervention and changes in operative technique. Although not much is known about the nature and progression of these lesions, surgical excision has remained a safe, reliable method of treatment.
Keywords: Epidural hematoma, Jehovah’s Witness, Middle meningeal artery, Pseudoaneurysm, Surgical resection
INTRODUCTION
Middle meningeal artery (MMA) pseudoaneurysms typically occur secondary to trauma and are frequently associated with overlying skull fracture.[
Given the anatomical location, epidural hematomas and pseudoaneurysms may occur due to traumatic lacerations of the MMA.[
MMA pseudoaneurysms causing small epidural hematomas can be detected using conventional angiogram, with CT angiography (CTA) representing a safe and reliable alternative.[
CASE REPORT
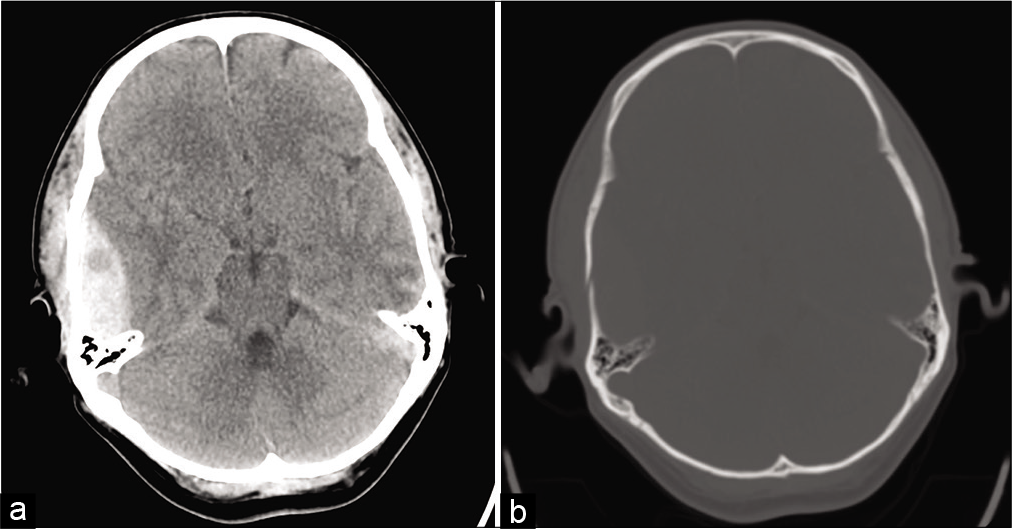
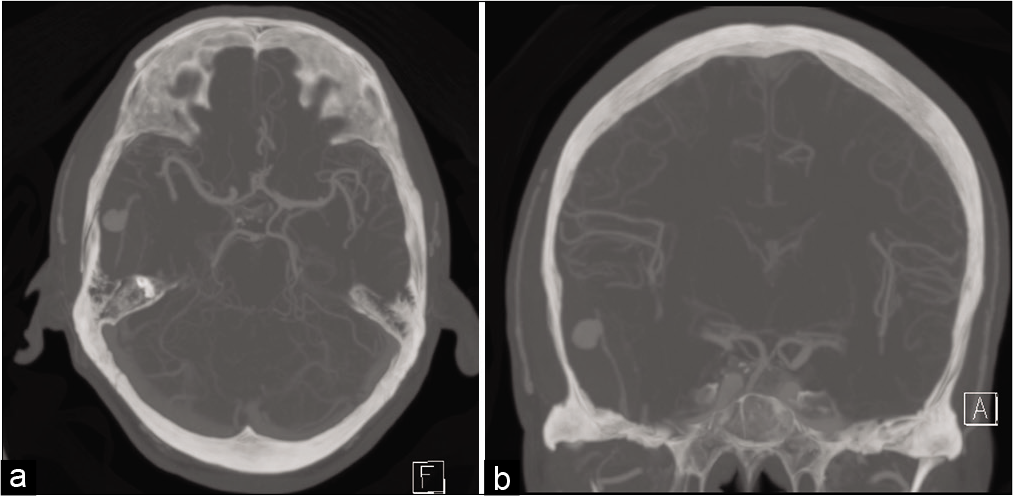
A 54-year-old male who identifies as a Jehovah’s Witness presented to our hospital with an epidural hematoma after a fall from standing. The patient had persistent headache, nausea, vomiting, somnolence, and altered mental status. CT without contrast demonstrated an 18 mm thick right-sided epidural hematoma, minimal midline shift, accompanying right-sided temporal bone fracture, subarachnoid hemorrhage, and a contralateral temporal lobe hemorrhagic contusion [
The patient did not exhibit any motor dysfunction; however, he reported severe headache. The patient had no focal deficit, and his epidural was moderate, but the discovery of the MMA pseudoaneurysm prompted more aggressive management of his lesion. Due to the patient’s symptoms, high mortality associated with rupture (up to 20%), and large size of his MMA pseudoaneurysm a right-sided craniotomy with aneurysm resection was performed.[
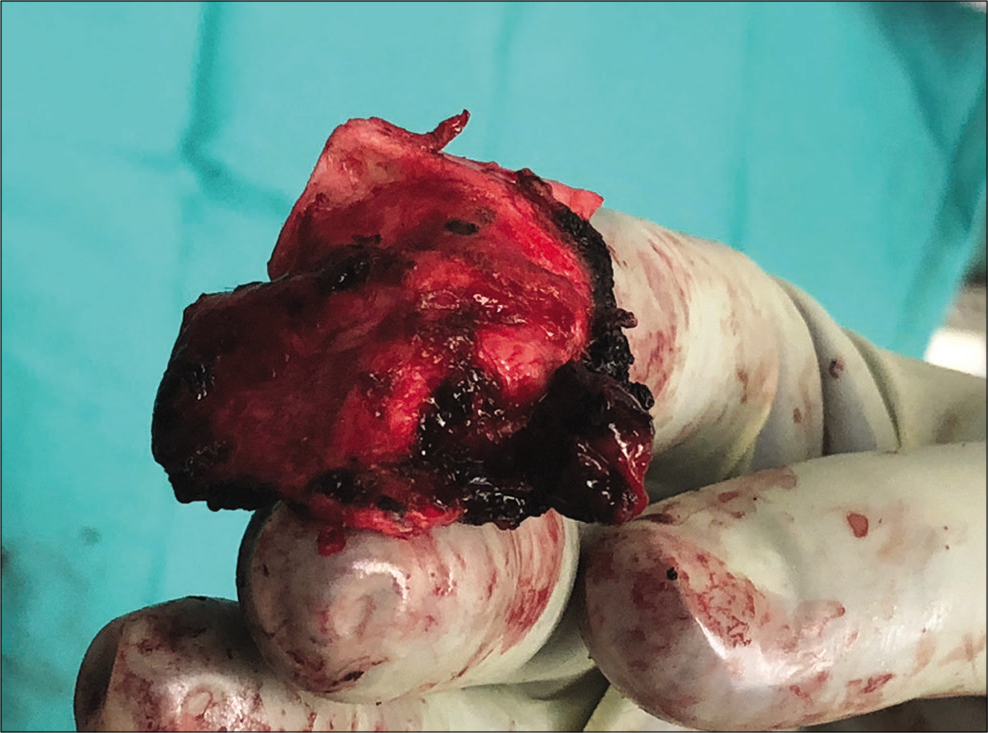
Given the patient’s denial of blood products, the minimization of blood loss was imperative. After temporal craniotomy, care was taken to preserve the epidural clot around the aneurysm to minimize re-rupture. The MMA was subsequently ligated with cautery proximal to the pseudoaneurysm. The pseudoaneurysm was visualized and resected along with a portion of the dura, and the epidural hematoma was evacuated [
DISCUSSION
Posttraumatic pseudoaneurysms of the MMA are rare, with 56 cases reported from 1957 to the present.[
Diagnostic testing with CTA has been recommended in the case of a temporal rim fracture with accompanying hemorrhage as this appears to be correlated with MMA pseudoaneurysm.[
The pseudoaneurysm reported here was large, measuring 10 mm. The patient was awake and nonfocal on examination, but the presence of the MMA pseudoaneurysm greatly increased the risk associated with conservative management of the patient’s epidural hematoma. Given the risk of fatal re-rupture, the decision was to urgently treat this lesion. The patient’s status as a Jehovah’s Witness added additional importance to minimize intraoperative blood loss. Jehovah’s Witnesses do not accept whole blood transfusions, packed red blood cells, plasma, or platelets due to their beliefs.[
Endovascular intervention of the MMA pseudoaneurysm was considered; however, we decided to pursue open intervention as this allowed treatment of the MMA pseudoaneurysm as well as the removal of the epidural hematoma for symptom relief. Preservation of the epidural clot around the MMA pseudoaneurysm minimized the risk of aneurysm re-rupture. We then ligated the MMA proximal to the aneurysm with cautery by incising the dura. The entirety of the aneurysm was then resected with a cuff of dura [
CONCLUSION
At this time, there are no established treatment guidelines, so the management of MMA pseudoaneurysms is primarily guided by patient status and clinical judgment. Endovascular treatments have been favored recently, but surgical resection or conservative treatments are options. In our case, surgical excision was elected due to the high risk of progression, the necessity of symptomatic epidural hematoma evacuation, and the unique challenge of the patient’s refusal of blood products. Surgical resection continues to be a safe treatment option for large MMA pseudoaneurysms.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Nakshabandi NA. The swirl sign. Radiology. 2001. 218: 433-3
2. Bruneau M, Gustin T, Zekhnini K, Gilliard C. Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage: Case report and literature review. Surg Neurol. 2002. 57: 174-8
3. de Virgilio C, Frank PN, Grigorian A.editors. Surgery: A Case Based Clinical Review. Berlin: Springer; 2015. p.
4. Gohel MS, Bulbulia RA, Slim FJ, Poskitt KR, Whyman MR. How to approach major surgery where patients refuse blood transfusion (including Jehovah’s Witnesses). Ann R Coll Surg Engl. 2005. 87: 3-14
5. Guo C, Liu L, Wang B, Wang Z. Swirl sign in traumatic acute epidural hematoma: Prognostic value and surgical management. Neurol Sci. 2017. 38: 2111-6
6. Jussen D, Wiener E, Vajkoczy P, Horn P. Traumatic middle meningeal artery pseudoaneurysms: Diagnosis and endovascular treatment of two cases and review of the literature. Neuroradiology. 2012. 54: 1133-6
7. Kimura T, Sako K, Satoh M, Nakai H, Yonemasu Y, Takeuchi E. Posttraumatic pseudoaneurysm of the middle meningeal artery: A case report. No Shinkei Geka. 1995. 23: 1021-5
8. Lee JY, Lee CY, Kim HW. Angiographically progressive change of traumatic pseudoaneurysm arising from the middle meningeal artery. J Korean Neurosurg Soc. 2014. 56: 423-7
9. Lim DH, Kim TS, Joo SP, Kim SH. Intracerebral hematoma caused by ruptured traumatic pseudoaneurysm of the middle meningeal artery : A case report. J Korean Neurosurg Soc. 2007. 42: 416-8
10. Marvin E, Laws LH, Coppens JR. Ruptured pseudoaneurysm of the middle meningeal artery presenting with a temporal lobe hematoma and a contralateral subdural hematoma. Surg Neurol Int. 2016. 7: S23-7
11. Montanari E, Polonara G, Montalti R, Vivarelli M, Ricciuti RA, Giorgetti R. Delayed intracerebral hemorrhage after pseudoaneurysm of middle meningeal artery rupture: Case report, literature review, and forensic issues. World Neurosurg. 2018. 117: 394-410
12. Paiva WS, Andrade AF, Amorim RL, Bor-Seng-Shu E, Gattas G, Neville IS. Computed tomography angiography for detection of middle meningeal artery lesions associated with acute epidural hematomas. Biomed Res Int. 2014. 2014: 413916
13. Park JW, Lee JY. Traumatic intracerebral and subarachnoid hemorrhage due to a ruptured pseudoaneurysm of middle meningeal artery accompanied by a medial sphenoid wing dural arteriovenous fistula. Korean J Neurotrauma. 2017. 13: 162-6
14. Shah Q, Friedman J, Mamourian A. Spontaneous resolution of traumatic pseudoaneurysm of the middle meningeal artery. Am J Neuroradiol. 2005. 26: 2530-2
15. Srinivasan A, Lesiuk H, Goyal M. Spontaneous resolution of posttraumatic middle meningeal artery pseudoaneurysm. Am J Neuroradiol. 2006. 27: 882-3
16. Wang CH, Lee HC, Cho DY. Traumatic pseudoaneurysm of the middle meningeal artery: Possible indicators for early diagnosis in the computed tomography era. Surg Neurol. 2007. 68: 676-81