- Department of Neurosurgery, National Hospital Organization Kumamoto Medical Center, Kumamoto, Japan.
Correspondence Address:
Airi Miyazaki, Department of Neurosurgery, National Hospital Organization Kumamoto Medical Center, Kumamoto, Japan.
DOI:10.25259/SNI_388_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Airi Miyazaki, Takashi Nakagawa, Jin Matsuura, Yoshihiro Takesue, Tadahiro Otsuka. Surgical safety criteria for burr hole surgery with urokinase in patients with acute subdural hematoma: Retrospective comparison between burr hole surgery and craniotomy. 23-Nov-2021;12:574
How to cite this URL: Airi Miyazaki, Takashi Nakagawa, Jin Matsuura, Yoshihiro Takesue, Tadahiro Otsuka. Surgical safety criteria for burr hole surgery with urokinase in patients with acute subdural hematoma: Retrospective comparison between burr hole surgery and craniotomy. 23-Nov-2021;12:574. Available from: https://surgicalneurologyint.com/surgicalint-articles/11241/
Abstract
Background: Acute subdural hematoma (ASDH) is a common disease and craniotomy is the first choice for removing hematoma. However, patients for whom craniotomy or general anesthesia is contraindicated are increasing due to population aging. In our department, we perform burr hole surgery under local anesthesia with urokinase administration for such patients. We compared the patient background and outcomes between burr hole surgery and craniotomy to investigate the surgical safety criteria for burr hole surgery.
Methods: We reviewed 24 patients who underwent burr hole surgery and 33 patients who underwent craniotomy between January 2010 and April 2020 retrospectively.
Results: The median age of the burr hole surgery group was older (P = 0.01) and they had multiple pre-existing conditions. Compared with the craniotomy group, neurological deficits and CT findings were minor in the burr hole surgery group, whereas the maximum hematoma thickness was not significantly different. The hematoma was excreted after a total of 54,000 IU of urokinase was administered for a median of 3 days. The Glasgow Coma Scale score improved in all patients in the burr hole surgery group and there were no deaths. Age, especially over 65 y.o., (OR 1.16, 95% CI 1.04–1.30) and the absence of basal cistern disappearance (OR 0.04, 95% CI 0.004–0.39) were significant factors.
Conclusion: Burr hole surgery was performed safely in all patients based on the age, especially older than 65 y.o., and the absence of basal cistern disappearance. ASDH in the elderly is increasing and less invasive burr hole surgery with urokinase is suitable for the super-aging society.
Keywords: Acute subdural hematoma, Burr hole surgery, Urokinase
INTRODUCTION
Acute subdural hematoma (ASDH) is a common disease caused by traumatic brain injury (TBI). ASDH compresses the brain and causes secondary pathologies such as cerebral ischemia and swelling. As a result, patients have a poor prognosis. Craniotomy for the removal of hematoma is recommended as the treatment method in the following cases: (1) The width of hematoma is 1 cm or greater, or the midline shift is 5 mm or greater. (2) Patients exhibit neurological symptoms due to hematoma. (3) The Glasgow Coma Scale (GCS) score decreased by more than two points.[
MATERIALS AND METHODS
Patients
We reviewed patients with ASDH as the main disease between January 2010 and April 2020 retrospectively. The following parameters were collected: age, gender, history of trauma, medical history, such as bleeding tendency or anti-thrombotic drug use, preoperative GCS score, pupil abnormality, maximum hematoma thickness, midline shift, patency of basal cistern, and skull fracture on preoperative computed tomography (CT). Outcomes were the length of hospitalization and days until operation from onset, the number of patients with urokinase administration, administration days and total dose, reduction of subdural hemorrhage (SDH) volume, GCS score at discharge, improved GCS score, mortality, and hospitalization. SDH volume was calculated as length*width*depth/2 and reduction of SDH volume (%) was calculated as ([volume at preoperative SDH – SDH volume at drain removal]/volume at preoperative SDH*100). Reduction of SDH volume was rated as excellent (≥75%), good (≥50%), fair (≥25%), or poor (<25%).
Operative technique for burr hole surgery
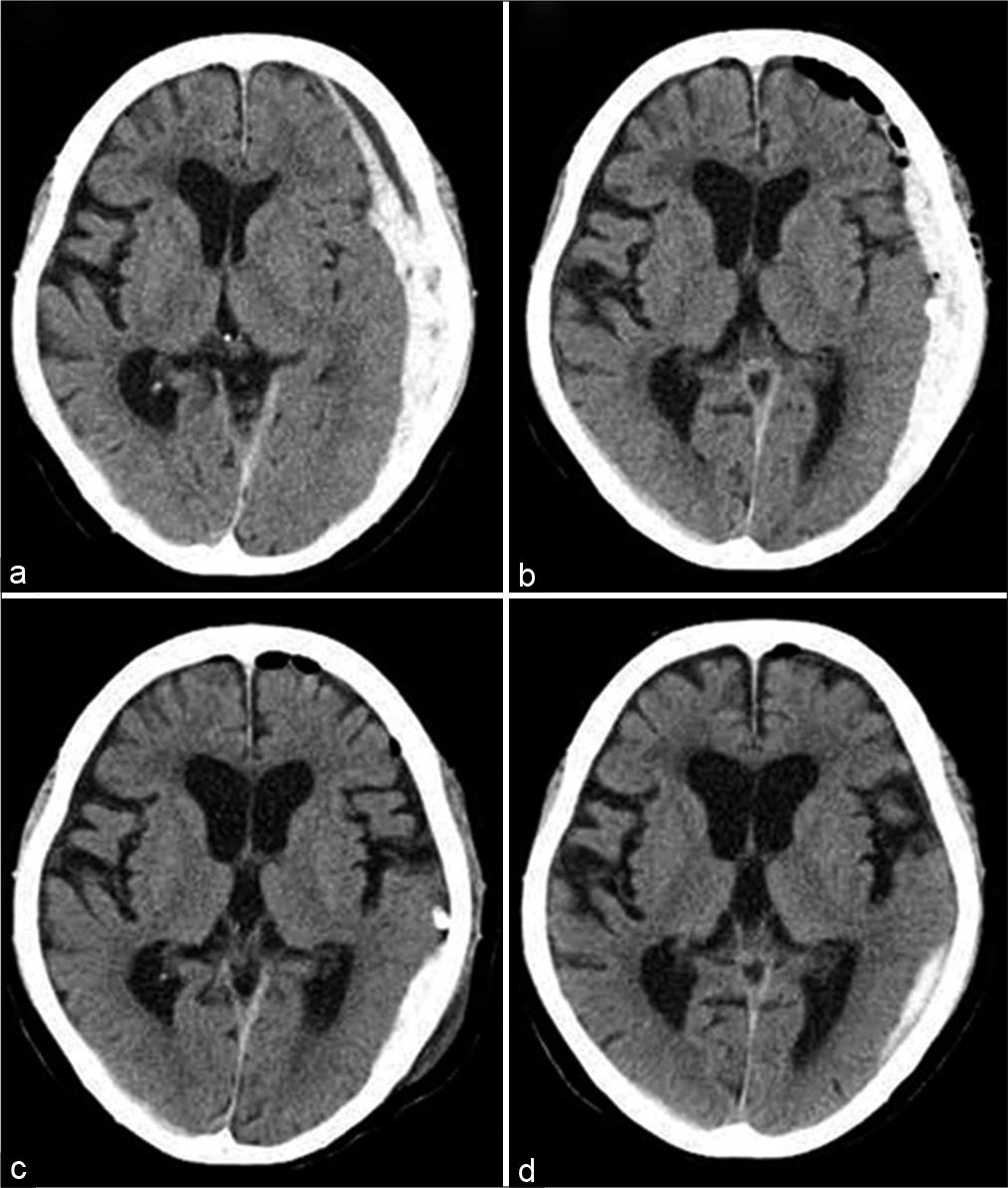
The incision was performed with local anesthesia under sedation. The hematoma was aspirated as much as possible and a drainage tube was inserted into the subdural space. If the hematoma did not decrease on CT the following day, urokinase (diluted to 60,000 units in 10 ml of saline, using 18,000–36,000 units/day) was injected. After clamping for 2 h, the hematoma drain was opened. These steps were repeated until the effects of hematoma were reduced [
Statistical analysis
We used the χ2 test and Mann-Whitney U test in univariate analysis, and logistic regression analysis in multivariate analysis. In our analyses, differences were considered significant at a value of P < 0.05. The statistical analyses were performed using IBM SPSS Statistics 27 (SPSS Inc., Chicago, IL, USA).
Ethical statement
Informed consent was received from all patients and this study protocol was approved by the ethics review committee of our institution (July 2020, IRB No. 844).
RESULTS
Twenty-four patients who underwent burr hole surgery and 33 who underwent craniotomy were available for analysis among a total of 604 ASDH patients. Those who underwent mini-craniotomy had chronic subdural hematoma, or underwent surgery more than 5 days after onset were excluded.
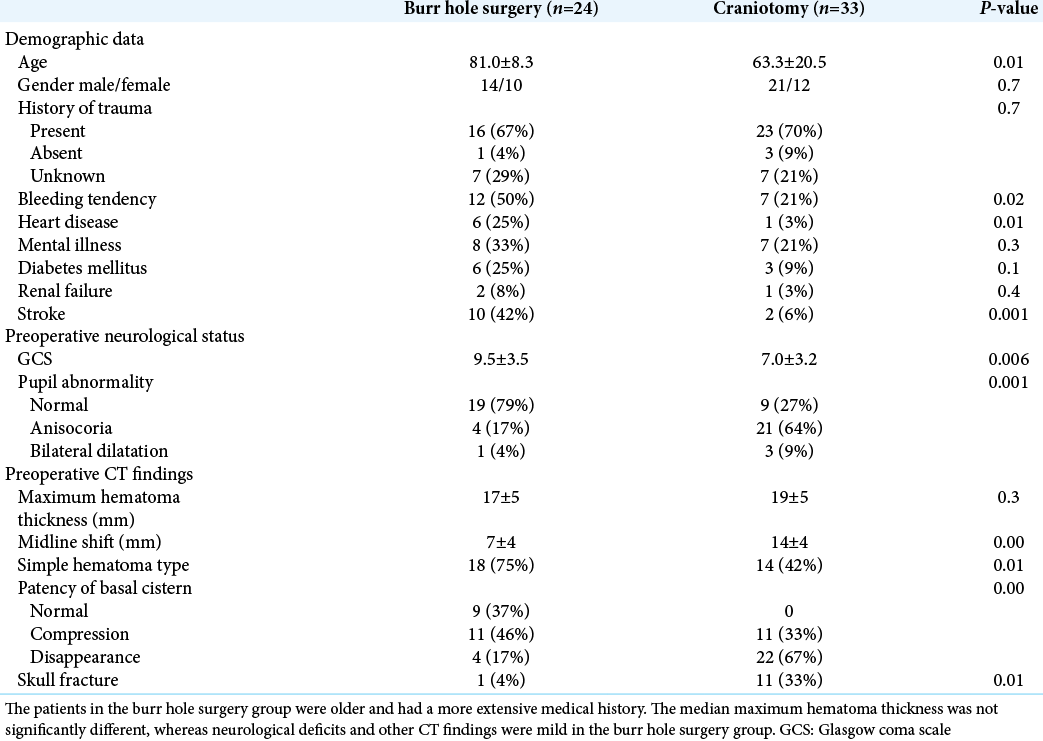
Patient characteristics are compared in
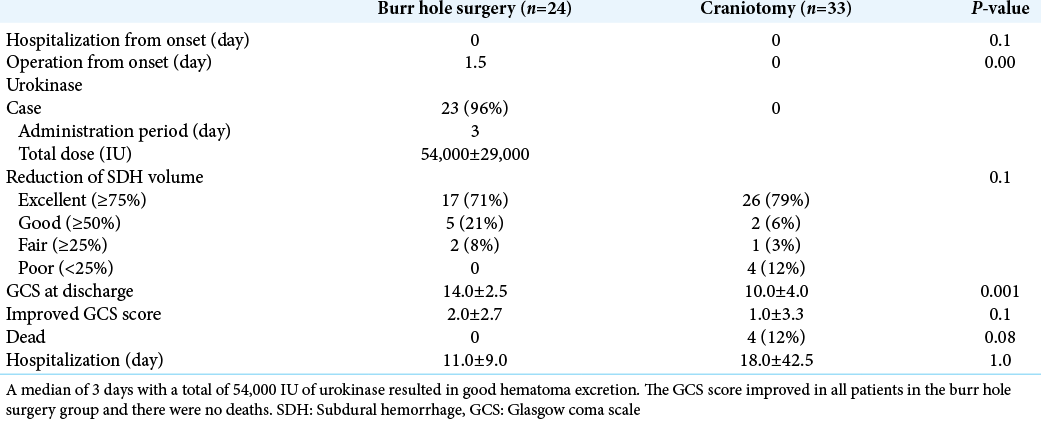
Craniotomy was performed on the day of admission, whereas burr hole surgery was often performed the day after confirming hemostasis on CT or when neurological findings worsened [
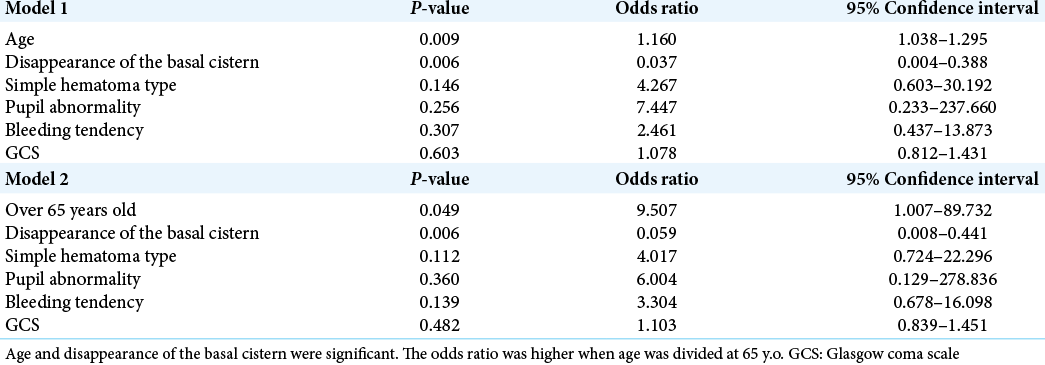
We selected 6 variables (age, bleeding tendency, GCS, simple hematoma type, pupil abnormality, and patency of the basal cistern) that were significantly related to the selection of burr hole surgery. Their predictive values were analyzed through multivariate logistic regression [
DISCUSSION
Burr hole surgery was selected to avoid the risks of general anesthesia and craniotomy such as bleeding or postoperative pneumonia.[
The safety criteria for burr hole surgery in this study were age, especially over 65 y.o., and the absence of basal cistern disappearance. These two points may lead to safe burr hole surgery. As the brain volume decreases in the elderly, the volume of subdural space increases and buffers compression of the brain by the hematoma.[
The disadvantages of burr hole surgery are the inability of hemostasis and excretion of solid hematoma. Regarding hemostasis, burr hole surgery was performed on a wait-and-see basis from the day after admission or at the time of worsening of neurological findings, during which natural hemostasis may have been achieved. In this study, as mentioned earlier, patients in the burr hole surgery group had mild neurological deficits and CT findings, which may have made it possible to perform a standby operation. In addition, the hematoma that was removed intraoperatively was in a solid state, with only a small amount just below the burr hole, and no intraoperative rebleeding occurred unless the hematoma was touched at the bleeding point. As for the remaining solid hematoma, excretion was good after the use of urokinase and there were no complications such as rebleeding. There is no prospective randomized study on subdural irrigation using alteplase. According to CLEAR III, alteplase irrigation via an extraventricular drain did not improve functional outcomes compared with saline irrigation. However, protocol-based use of alteplase was suggested to be safe.[
In this study, half of the patients in the burr hole surgery group had a history of bleeding tendency. However, this was not related to the choice of operation. The number of patients with pre-existing medical conditions is increasing as the population ages and 30% of patients with severe TBI aged over 65 y.o. are taking antithrombotic drugs in Japan.[
LIMITATIONS
This was a single-center, retrospective study with a small sample size. The patients exhibited severe neurological deficits, and immediate craniotomy and decompression were required based on CT. Therefore, there may have been a selection bias. As there is no consensus on burr hole surgery with urokinase in patients with ASDH, further studies with a larger sample size and prospective randomized trials are required.
CONCLUSION
Burr hole surgery was performed safely in all patients for whom craniotomy and general anesthesia were unfavorable. Burr hole surgery was selected based on age, especially in those over 65 y.o., and the absence of basal cistern disappearance. ASDH in the elderly due to minor head injury is increasing due to the aging population and increased use of antithrombotic drugs. Accordingly, burr hole surgery with urokinase avoids the risks of craniotomy and general anesthesia and is suitable for the super-aging society.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cho SW, Choi SW, Lim J, Kwon HJ, Kim SH, Koh HS. Burr hole drainage with urokinase irrigation for the treatment of acute subdural hematoma: A case report. Korean J Neurotrauma. 2018. 14: 142-5
2. Gaberel T, Magheru C, Parienti JJ, Huttner HB, Vivien D, Emery E. Intraventricular fibrinolysis versus external ventricular drainage alone in intraventricular hemorrhage: A meta-analysis. Stroke. 2011. 42: 2776-81
3. Gardner RC, Dams-O’Connor K, Morrissey MR, Manley GT. Geriatric traumatic brain injury: Epidemiology, outcomes, knowledge gaps, and future directions. J Neurotrauma. 2018. 35: 889-906
4. Hanley DF, Lane K, McBee N, Ziai W, Tuhrim S, Lees KR. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: Results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet. 2017. 389: 603-11
5. Huang AP, Tu YK, Tsai YH, Chen YS, Hong WC, Yang CC. Decompressive craniectomy as the primary surgical intervention for hemorrhagic contusion. J Neurotrauma. 2008. 25: 1347-54
6. Huang PK, Sun YZ, Xie XL, Kang DZ, Zheng SF, Yao PS. Twist drill craniostomy for traumatic acute subdural hematoma in the elderly: Case series and literature review. Chin Neurosurg J. 2019. 5: 10
7. Kannus P, Palvanen M, Niemi S, Parkkari J, Natri A, Vuori I. Increasing number and incidence of fall-induced severe head injuries in older adults: Nationwide statistics in Finland in 1970-1995 and prediction for the future. Am J Epidemiol. 1999. 149: 143-50
8. Karibe H, Hayashi T, Hirano T, Kameyama M, Nakagawa A, Tominaga T. Surgical management of traumatic acute subdural hematoma in adults: A review. Neurol Med Chir (Tokyo). 2014. 54: 887-94
9. Karibe H, Hayashi T, Narisawa A, Kameyama M, Nakagawa A, Tominaga T. Clinical characteristics and outcome in elderly patients with traumatic brain injury: For establishment of management strategy. Neurol Med Chir (Tokyo). 2017. 57: 418-25
10. Lucke-Wold BP, Turner RC, Josiah D, Knotts C, Bhatia S. Do age and anticoagulants affect the natural history of acute subdural hematomas?. Arch Emerg Med Crit Care. 2016. 1: 1010
11. Sato J, Karibe H, Nimura T, Hirano T, Takada S. The effect of trepanation surgery to the cases with difficulties in craniotomy for acute subdural hematoma. J Jpn Congr Neurol Emerg. 2009. 21: 39-43
12. Suehiro E, Fujiyama Y, Kiyohira M, Haji K, Ishihara H, Nomura S. Japan neurotrauma data bank committee. Risk of deterioration of geriatric traumatic brain injury in patients treated with antithrombotic drugs. World Neurosurg. 2019. 127: e1221-7
13. Uccella L, Zoia C, Bongetta D, Gaetani P, Martig F, Candrian C. Are antiplatelet and anticoagulants drugs a risk factor for bleeding in mild traumatic brain injury?. World Neurosurg. 2018. 110: e339-45
14. Volbers B, Niesen WD, Amiri-Soltani S, Staykov D, Shah MJ, Lang S. Bedside catheter hematoma evacuation in vitamin k antagonist-related intracerebral hemorrhage: A safe and feasible approach. Front Neurol. 2020. 11: 807
15. Wang GQ, Li SQ, Huang YH, Zhang WW, Ruan WW, Qin JZ. Can minimally invasive puncture and drainage for hypertensive spontaneous basal ganglia intracerebral hemorrhage improve patient outcome: A prospective non-randomized comparative study. Mil Med Res. 2014. 1: 10
16. Wilberger JE, Harris M, Diamond DL. Acute subdural hematoma: Morbidity, mortality, and operative timing. J Neurosurg. 1991. 74: 212-8
17. Zhang D, Zhuo H, Yang G, Huang H, Li C, Wang X. Postoperative pneumonia after craniotomy: Incidence, risk factors and prediction with a nomogram. J Hosp Infect. 2020. 105: 167-75