- Department of Neurological Surgery, University of California, Sacramento, United States
- Department of School of Medicine, University of California, Sacramento, United States
- Department of Neurological Surgery, Kaiser Permanente Sacramento Medical Center, Sacramento, United States.
Correspondence Address:
Nina Yu, University of California, Davis, United States.
DOI:10.25259/SNI_939_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Catherine Peterson1, Nina Yu2, Huy T. Duong3. Surgical treatment of a giant paraophthalmic aneurysm postfailed flow diversion through endoscopic endonasal approach: Technical nuances and review of the literature. 08-Mar-2024;15:75
How to cite this URL: Catherine Peterson1, Nina Yu2, Huy T. Duong3. Surgical treatment of a giant paraophthalmic aneurysm postfailed flow diversion through endoscopic endonasal approach: Technical nuances and review of the literature. 08-Mar-2024;15:75. Available from: https://surgicalneurologyint.com/surgicalint-articles/12791/
Abstract
Background: Giant internal carotid artery (ICA) aneurysms are usually treated through flow diversion, coiling, or a combination of both. However, certain cases that fail the endovascular treatment pose a technical challenge.
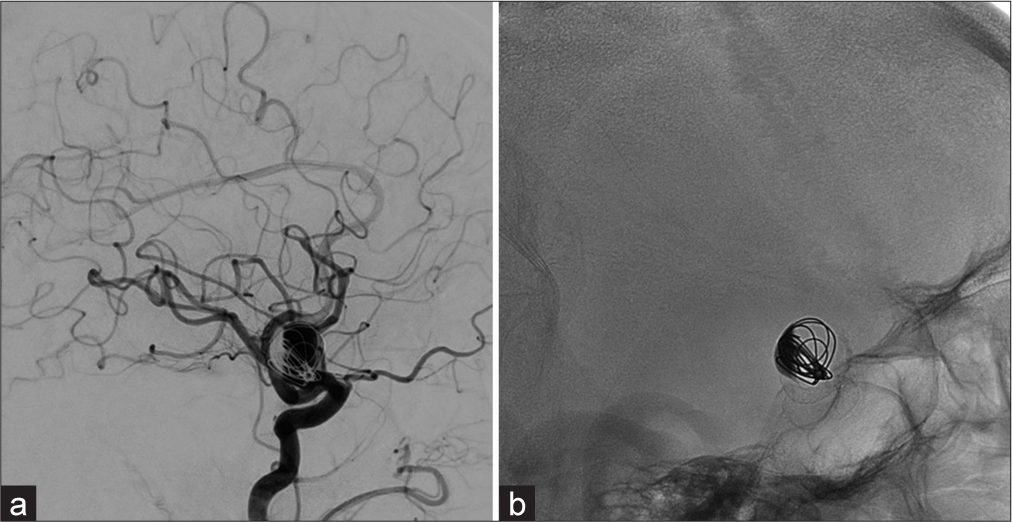
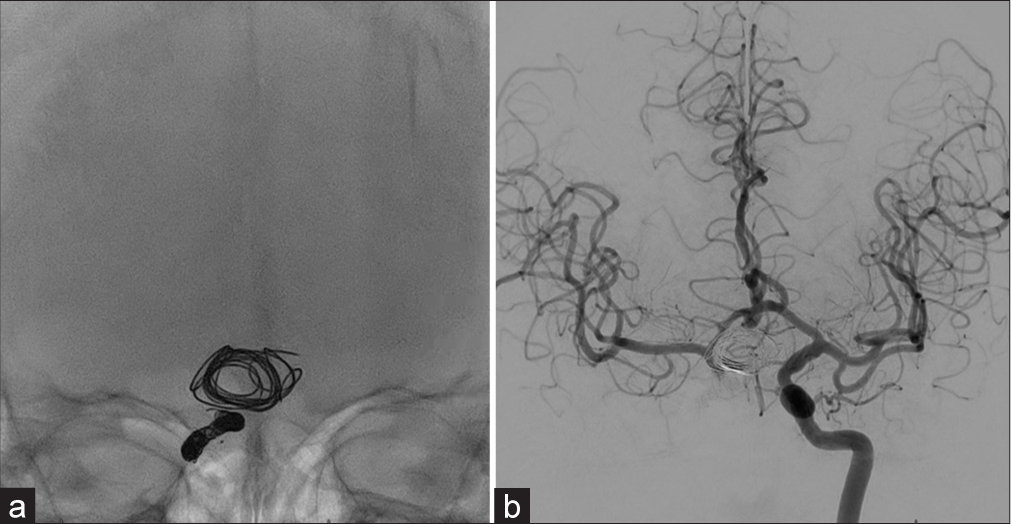
Case Description: A 68-year-old male presented with gradual visual changes affecting his right eye and was found to have a giant unruptured right paraophthalmic aneurysm. The aneurysm showed growth, and the patient’s symptoms worsened despite coiling and flow diversion. Due to the location of this aneurysm and persistent compression of the optic chiasm by the coil mass, his right ICA was sacrificed, and an expanded endoscopic endonasal approach was successfully used to clip the residual aneurysm, remove the coil mass, and thus, decompress the optic chiasm. The patient’s visual symptoms improved after that, and post clipping imaging demonstrated adequate occlusion of his right paraophthalmic aneurysm.
Conclusion: Recognizing the option of an endoscopic endonasal approach for clipping giant internal carotid aneurysms is of great importance. This approach can be safe and technically successful for the treatment of paraophthalmic aneurysms that fail the typical endovascular treatment.
Keywords: Aneurysm, Clipping, Endonasal, Endoscopic, Paraophthalmic
INTRODUCTION
Paraophthalmic aneurysms characteristically arise from the internal carotid artery (ICA) and clinically present with various visual deficits ranging in severity. These include aneurysm rupture with subarachnoid hemorrhage, and nonspecific symptoms such as headache, tinnitus, vertigo, transient ischemic attacks, or otherwise are incidentally discovered. In addition, these aneurysms pose technical challenges due to their proximity to critical intracranial structures.[
The current treatment options include coil embolization, flow diversion, surgical clipping, or a combination of these treatment modalities. The majority are commonly treated through an endovascular approach that typically involves the placement of a flow diverter stent. However, endovascular treatment with flow diversion is not without risk and may not completely occlude giant aneurysms presenting with cranial neuropathies such as ophthalmologic symptoms. In these cases, surgical clipping remains an option.[
In this operative report, we present a case of a 68-year-old male with a giant unruptured right paraophthalmic artery aneurysm presenting with visual symptoms. After initial coiling and flow diversion, the aneurysm showed growth, and the patient’s visual symptoms worsened. An expanded endoscopic endonasal transsphenoidal approach was successfully used to clip the residual aneurysm and decompress the coil mass and the optic chiasm, improving the patient’s symptoms and preventing further visual loss.
CASE REPORT
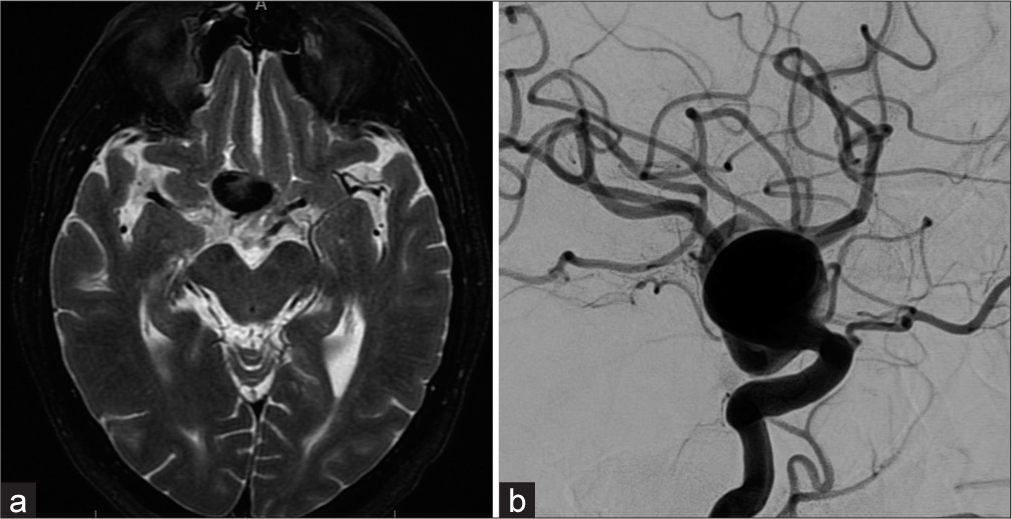
A 68-year-old male with a history of hypertension presented with a 1-year history of gradually decreasing right eye visual acuity with occasional headaches. His examination was nonfocal except for decreased visual acuity in the right eye without papilledema. Magnetic resonance imaging was initially ordered and demonstrated a giant right paraophthalmic aneurysm [
Operative technique
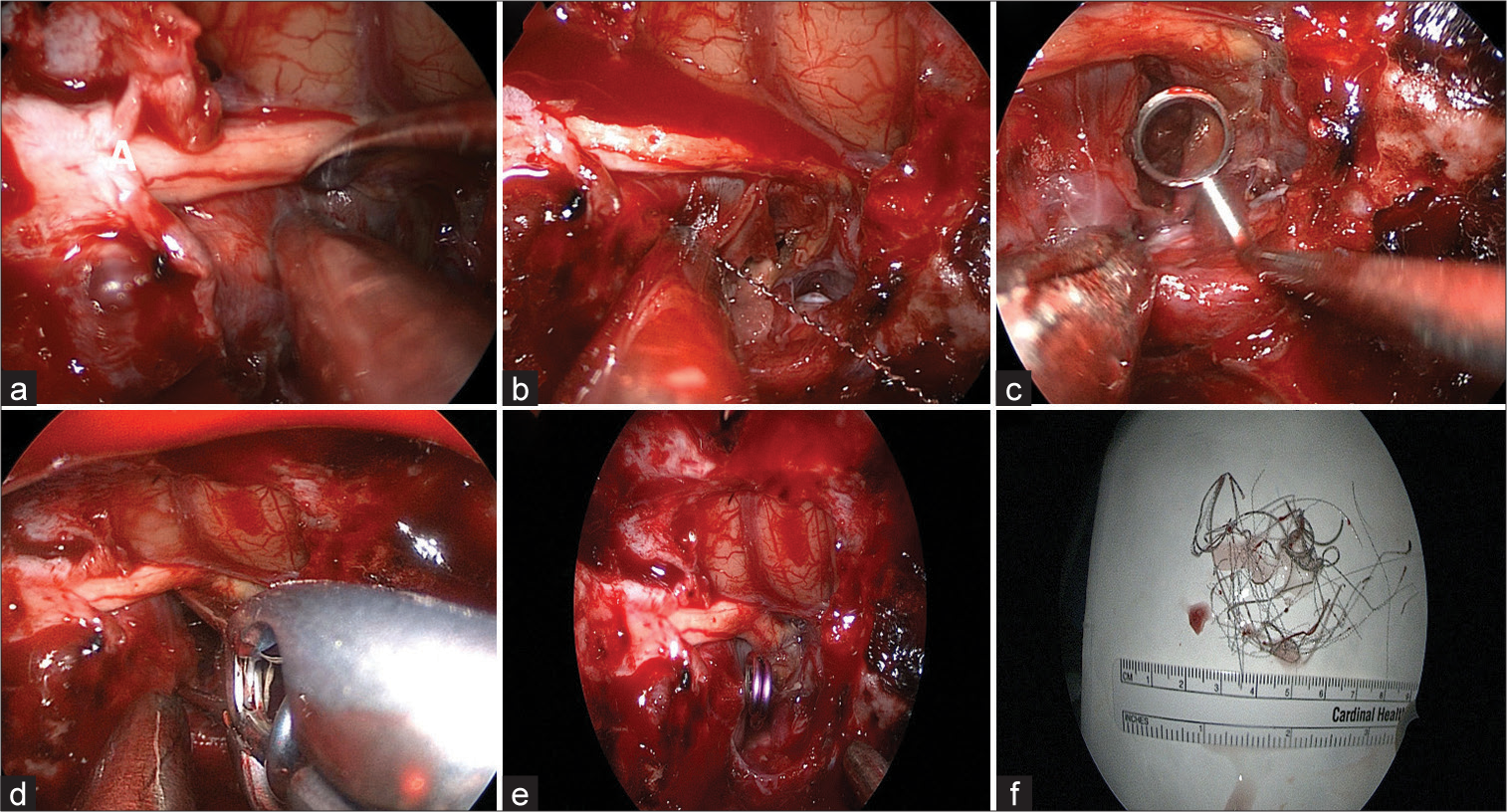
After his right ICA sacrifice, there was no residual filling of the aneurysm or the right ICA beyond the communicating segment from the contralateral side through the anterior communicating artery complex. The patient underwent an expanded endoscopic endonasal approach for clipping and resection of his right paraophthalmic aneurysm [
Figure 4:
Intraoperative photographs of (a) compression of the right optic nerve and chiasm by a giant aneurysm, (b) evacuation of its coils, (c) further evacuation of its contents with a ring curette, (d) clipping of the aneurysm, (e) final position of the straight clip and resultant decompression of the optic apparatus, and (f) evacuated coils and clot from the previously coiled aneurysm mass.
DISCUSSION
The majority of giant paraophthalmic aneurysms are commonly treated through coil embolization with or without stenting or flow diversion. Complications of flow diverters may include stent migration and ophthalmic complications such as optic perineuritis. The other limitation of the endovascular approach to these aneurysms is that the stent/coil approach may result in incomplete occlusion of the aneurysm and the subsequent need for retreatment. Another treatment modality for giant paraophthalmic and ophthalmic aneurysms is surgical clipping. However, this approach may result in mixed outcomes with visual acuity recovery on a wide spectrum. The variability in outcomes may be attributed to the degree of aneurysm calcification, size, thrombosis, and other patient-specific demographics and co-morbidities.
Here, we reported a case of a giant unruptured right paraophthalmic artery aneurysm that failed endovascular treatment and was successfully clipped with optic chiasm decompression through an expanded endoscopic endonasal approach. The endoscopic endonasal approach is routinely implemented to excise pituitary neoplasms but also serves as an uncommon surgical option for clipping aneurysms coming off ICA and its paraclinoid branches. From conducting a literature review, we found only a few reports describing the use of this technique.[
CONCLUSION
Giant paraophthalmic artery aneurysms typically present with various ophthalmologic disturbances. Management consists of endovascular embolization through flow diversion and/or coiling, as well as less common surgical clipping. The endoscopic endonasal transsphenoidal approach for clipping such aneurysms has been minimally reported in the literature but remains a feasible option. Through the illustrative case presented here, we have demonstrated the technical nuances of surgical clipping of a giant paraophthalmic aneurysm through an endoscopic endonasal approach after endovascular treatment has failed.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akiyama R, Ishii A, Kikuchi T, Okawa M, Yamao Y, Abekura Y. Onset-to-treatment time and aneurysmal regression predict improvement of cranial neuropathy after flow diversion treatment in patients with symptomatic internal carotid artery aneurysms. J Neurointerv Surg. 2023. 15: 886-91
2. Bao YY, Yang YQ, Zhou L, Xie SH, Wu X, Ding H. Endoscopic endonasal supraoptic and infraoptic approaches for complex “parasuprasellar” lesions: Surgical anatomy, technique nuances, and case series. Front Oncol. 2022. 12: 847250
3. Boulouis G, Soize S, Maus V, Fischer S, Lobsien D, Klisch J. Flow diversion for internal carotid artery aneurysms with compressive neuro-ophthalmologic symptoms: Clinical and anatomical results in an international multicenter study. J Neurointerv Surg. 2022. 14: 1090-5
4. Brown BL, Lopes D, Miller DA, Tawk RG, Brasiliense LB, Ringer A. The fate of cranial neuropathy after flow diversion for carotid aneurysms. J Neurosurg. 2016. 124: 1107-13
5. Falk Delgado A, Andersson T, Falk Delgado A. Ruptured carotid-ophthalmic aneurysm treatment: A non-inferiority meta-analysis comparing endovascular coiling and surgical clipping. Br J Neurosurg. 2017. 31: 345-9
6. Froelich S, Cebula H, Debry C, Boyer P. Anterior communicating artery aneurysm clipped via an endoscopic endonasal approach: Technical note. Neurosurgery. 2011. 68: 310-6 discussion 315-6
7. Gardner PA, Vaz-Guimaraes F, Jankowitz B, Koutourousiou M, Fernandez-Miranda JC, Wang EW. Endoscopic endonasal clipping of intracranial aneurysms: Surgical technique and results. World Neurosurg. 2015. 84: 1380-93
8. Gu Y, Zhong X, Gao Y, He L. Endoscopic endonasal approach for simultaneously treating a pituitary adenoma coexisting with a paraclinoid aneurysm: Illustrative case. J Neurosurg Case Lessons. 2022. 3: CASE22130
9. Kitano M, Taneda M. Extended transsphenoidal approach to anterior communicating artery aneurysm: Aneurysm incidentally identified during macroadenoma resection: Technical case report. Neurosurgery. 2007. 61: E299-300 discussion E300
10. Silva MA, See AP, Dasenbrock HH, Patel NJ, Aziz-Sultan MA. Vision outcomes in patients with paraclinoid aneurysms treated with clipping, coiling, or flow diversion: A systematic review and meta-analysis. Neurosurg Focus. 2017. 42: E15