- Department of Neurosurgery, Santa Marcelina Hospital, São Paulo, Brazil.
DOI:10.25259/SNI_493_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anderson Batista Rodrigues, Daniella Brito Rodrigues, Joao Welberthon Matos Queiroz, Kaito Alves Carvalho Laube, Murillo Cunegatto Macullo Braga, William Seiti Kita, Allexsandro Aparecido Alvarenga Nascimento Faria De Luna, Rafael Wilson De Souza, Ricardo Henrique Doria Netto. Surgical treatment of spinal arachnoid web: Report of two cases and literature review. 28-Jun-2021;12:316
How to cite this URL: Anderson Batista Rodrigues, Daniella Brito Rodrigues, Joao Welberthon Matos Queiroz, Kaito Alves Carvalho Laube, Murillo Cunegatto Macullo Braga, William Seiti Kita, Allexsandro Aparecido Alvarenga Nascimento Faria De Luna, Rafael Wilson De Souza, Ricardo Henrique Doria Netto. Surgical treatment of spinal arachnoid web: Report of two cases and literature review. 28-Jun-2021;12:316. Available from: https://surgicalneurologyint.com/surgicalint-articles/10920/
Abstract
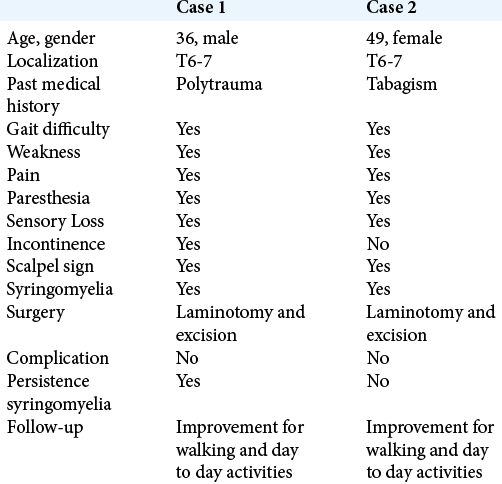
Background: Arachnoid webs (AWs) can cause cord compression and syringomyelia in the thoracic spine. Here, we describe two patients who underwent operative treatment for AW and reviewed the literature.
Case Description: Two patients underwent surgical treatment for thoracic AW. Both presented with spastic gait and numbness in the lower extremities. On MR, these lesions exhibited the “scalpel” sign (i.e. due to the accumulation of cerebrospinal fluid on the dorsal aspect of the spinal cord). Operative intervention, consisting of fenestration and web resection, resulted in symptom resolution.
Conclusion: Thoracic AWs are rare lesions that should be considered among the differential diagnosis of spinal compressive syndromes. Surgical fenestration and resection of the AW correct the flow dynamics allowing for full symptoms resolution.
Keywords: Arachnoid web, Scalpel sign, Surgical treatment, Syringomyelia, Thoracic spine
INTRODUCTION
“Spinal arachnoid web (AW)” is defined by a thickening of the arachnoid membrane occurring along the spinal cord under the pial surface. It is believed to originate from a malformed or ruptured arachnoid cyst. These AWs are rare and can cause compressive myelopathy particularly in the thoracic spine.[
On magnetic resonance (MR) T2-weighted sagittal sequences, these lesions produce the “scalpel sign,” due to AW’s resultant accumulation of cerebrospinal fluid (CSF) on the dorsal aspect of the spinal cord.[
CASE REPORT
Case 1
History and examination
A 36-year-old male presented with a progressive weakness of the left leg greater than the right leg (range of 4− to 4+/5), hyperactive lower extremity reflexes/Babinski responses, a bilateral L1 relatively sensory level, and sphincter dysfunction of 4 month’s duration.
Imaging studies
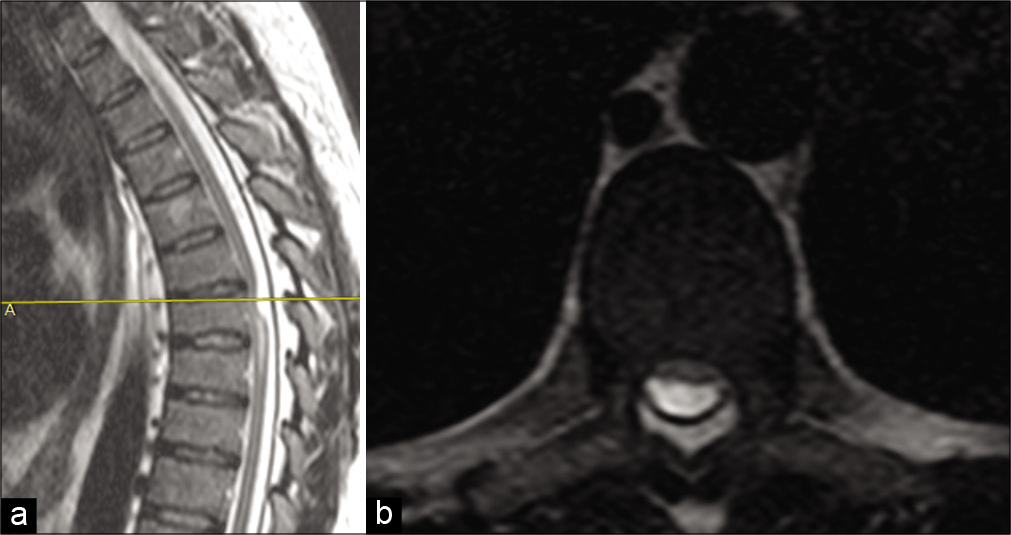
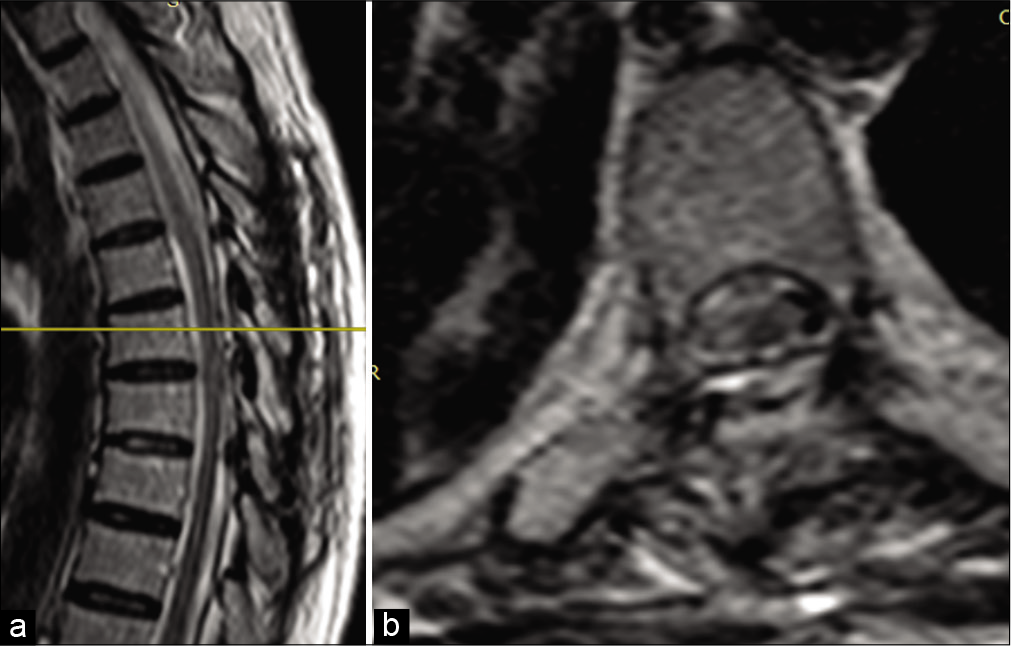
The magnetic resonance imaging (MRI) of the thoracic spine showed the spinal cord compression at the T7 level (enlargement of the spinal cord is the positive “scalpel sign:” focal dorsal indentation secondary to deformity of the cord at the level, because of the resemblance on sagittal MRI images to a scalpel with its blade pointing posteriorly) and inferior syringomyelia [
Figure 1:
(a) Sagittal T2-weighted magnetic resonance image (MRI) of the thoracic spine showing the spinal cord anteriorly displaced at the level of T7, with enlargement of the dorsal liquor space (“scalpel sign”) and narrowing of the spinal cord, associated with the inferior syringomyelia area. (b) Axial T2-weighted MRI of the thoracic spine showing the spinal cord anteriorly displaced by arachnoid web.
These findings were consistent with the diagnosis of an AW or anterior spinal cord herniation.
Surgical report
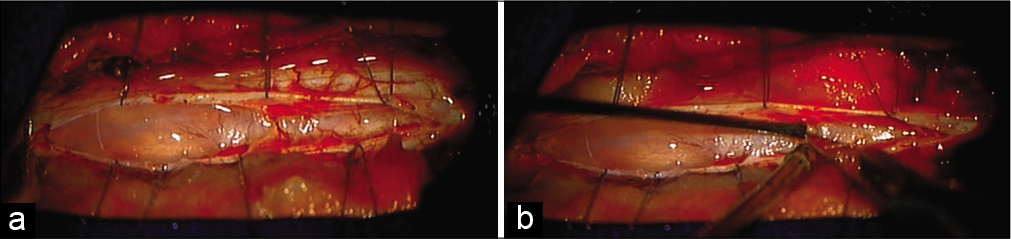
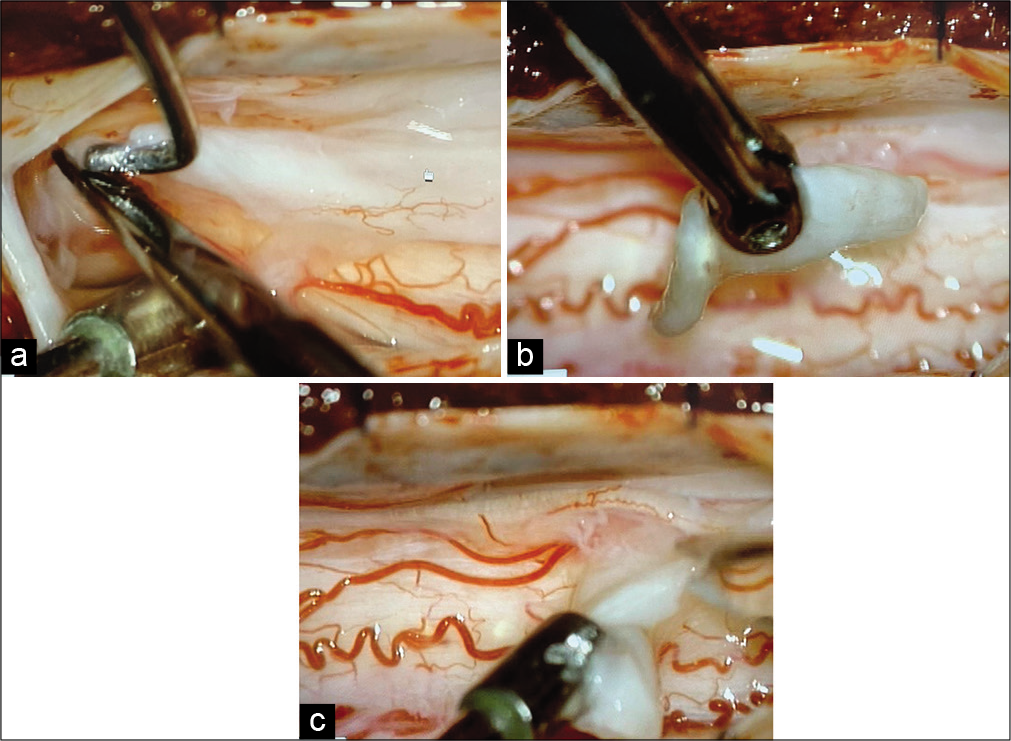
The patient underwent a T6–T7 laminotomy. A midline durotomy was then performed. After the opening the arachnoid, exposing the dorsal cord, there were multiple septate membranes between the dura and the spinal cord that thick fibrotic tissue appeared to strange the cord (i.e. adhesions to the ventral dura, contributed to cord compression) [
Follow-up
There were no postoperative complications, and the patient was discharged days later. The 3 months postoperative MR showed resolution of spinal compression and but residual syringomyelia [
Case 2
History and examination
A 49-year-old female also presented with paraparesis/ myelopathy but intact sphincter function. The thoracic MRI of again showed the spinal cord displaced at the T7 level, with a central syrinx [
Figure 4:
Preoperative magnetic resonance images (MRI) obtained in the patient in Case 2. Sagittal T2-weighted MRI of the thoracic spine showing the spinal cord anteriorly displaced at the level of T7, with enlargement of the spinal cord liquor (“scalpel sign”) and narrowing of the spinal cord. Hypersignal indicating segmental myelopathy.
Figure 6:
(a) Postoperative magnetic resonance images (MRI) obtained in the patient in Case 2. Sagittal T2-weighted MRI of the thoracic spine showing resolution of the arachnoid web at the T7 level. (b) Axial T2-weighted MRI of the thoracic spine at the T7 level showing improvement of spinal cord displacement.
DISCUSSION
Definition and etiology
AWs are rare pathology. They are defined as intradural transverse extramedullary bands of arachnoid tissue connecting the dorsal surface of the spinal cord to the dura. A total of 43 cases have been documented.[
Epidemiology
The majority of patients present with thoracic AW; they are typically male, middle aged, and present with paraparesis/ myelopathy.[
Diagnosis
MRI is the most accurate test for diagnosing AW.[
Treatment and outcome
Surgical treatment should include fenestration and resection of the web.[
CONCLUSION
AWs are rare typically thoracic lesions responsible for a compressive myelopathy that is readily relieved with operative decompression.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chang HS, Nagai A, Oya S, Matsui T. Dorsal spinal arachnoid web diagnosed with the 12 quantitative measurement of cerebrospinal fluid flow on magnetic resonance 13 imaging. J Neurosurg Spine. 2014. 20: 227-33
2. Hirai T, Taniyama T, Yoshii T, Mizuno K, Okamoto M, Inose H. Clinical outcomes of surgical treatment for arachnoid web: A case series. Spine Surg Relat Res. 2019. 3: 43-8
3. Hubbard ME, Hunt MA, Jones KE, Polly DW. Thoracic spinal cord impingement by an arachnoid web at the level of a hemivertebra: Case report. J Neurosurg Spine. 2017. 27: 638-42
4. Nisson BS, Hussain I, Härtl R, Kim S, Baaj AA. Arachnoid web of the spine: A systematic literature review. J Neurosurg Spine. 2019. 31: 175-84
5. Reardon MA, Raghavan P, Carpenter-Bailey K, Mukherjee S, Smith JS, Matsumoto JA. Dorsal thoracic arachnoid web and the “scalpel sign”: A distinct clinical-radiologic. Am J Neurorradiol. 2013. 34: 1104-10
6. Viswanathan VK, Manoharan SR, Do H, Minnema A, Shaddy SM, Elder JB. Clinical and radiologic outcomes after fenestration and partial wall excision of idiopathic intradural spinal arachnoid cysts presenting with myelopathy. World Neurosurg. 2017. 105: 213-22
7. Zhang D, Papavassiliou E. Spinal intradural arachnoid webs causing spinal cord compression with inconclusive preoperative imaging: A report of 3 cases and a review of the literature. World Neurosurg. 2017. 99: 251-8