- Department of Neurosurgery, Dr. Hasan Sadikin Hospital, Padjadjaran University, Bandung, West Java, Indonesia
Correspondence Address:
Yulius Hermanto, Department of Neurosurgery, Dr. Hasan Sadikin Hospital, Padjadjaran University, Bandung, West Java, Indonesia.
DOI:10.25259/SNI_685_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Roland Sidabutar1, Yulius Hermanto1, Agung Budi Sutiono1, Guata Naibaho1, Ahmad Faried1. Surgical treatment of tuberculum sellae meningioma: A retrospective review of single institutional experience. 29-Nov-2024;15:440
How to cite this URL: Roland Sidabutar1, Yulius Hermanto1, Agung Budi Sutiono1, Guata Naibaho1, Ahmad Faried1. Surgical treatment of tuberculum sellae meningioma: A retrospective review of single institutional experience. 29-Nov-2024;15:440. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13258
Abstract
Background: Tuberculum sellae meningiomas (TSMs) represent a distinct entity among intracranial meningiomas. Both transcranial approaches (TCAs) and endoscopic endonasal approaches (EEAs) have provided neurosurgeons with options for managing these difficult tumors. Still, controversies persist regarding the selection criteria for the most optimal approach.
Methods: The authors retrospectively reviewed 45 patients treated surgically for TSM between 2018 and 2023. The clinical reports of all subjects were assessed pre-and post-operatively, encompassing demographic information, clinical symptoms, imaging results, ophthalmological evaluations, operative details, and any complications.
Results: A total of 45 patients were included in this study, with 21 patients undergoing EEAs and 24 TCAs. TSMs treated with EEA are smaller than TCA (P = 0.0014), less prevalent in optic canal invasion (P = 0.0291) and in arterial encasement (P = 0.0050), and have no lateral extension (P P = 0.0032). The mortality tends to be higher in the TCA group and is related to arterial encasement, although statistically insignificant.
Conclusion: Both traditional TCAs and EEAs offer options for the surgical management of TSM, each with its advantages and limitations. Based on our experiences, several factors (lateral extension and arterial encasement) may guide the suitable approach, and multidisciplinary considerations, with the overarching goals of achieving maximal tumor resection and minimizing postoperative complications.
Keywords: Endoscopic endonasal, Meningioma, Skull base, Trans sphenoidal, Tuberculum sellae
INTRODUCTION
Tuberculum sellae meningiomas (TSMs) represent a distinct clinical entity among intracranial meningiomas. TSMs arise near the sella turcica, a bony-saddle-shaped structure at the center of the skull base.[
The primary goal of TSM surgery is to achieve maximal tumor removal and improve visual function while preserving critical neurovascular structures.[
The emergence of both traditional transcranial approaches (TCAs) and endoscopic endonasal approaches (EEAs) in the surgical management of TSMs has provided neurosurgeons with valuable options for approaching these challenging tumors.[
This retrospective study aimed to describe our institutional experiences in surgically managing TSMs in 45 consecutive patients. The emphasis was placed on preoperative evaluation, particularly considering tumor characteristics and anatomical factors that play pivotal roles in determining the most suitable surgical approach and subsequent postoperative outcomes.
MATERIALS AND METHODS
Patients
This study received approval from the Institutional Review Board (IRB) at our institution. This retrospective study enrolled all patients of TSMs who experienced TCA or EEA surgery at Dr Hasan Sadikin Hospital between January 2018 and December 2023 (a total of 45 cases). All patients were pathologically confirmed as meningioma (93.3% of cases were WHO grade I). Meningiomas originating from the clinoid processes, olfactory groove, and planum sphenoidal were excluded from the study. The surgical indications included vision impairment, progressive headache, and intracranial hypertension. Traditional TCAs, such as pterional (16 patients), subfrontal interhemispheric (seven patients), and lateral supraorbital craniotomy (one patient), as well as extended EEA surgeries (21 patients), were performed to resect the tumor. All TCA procedures were conducted by experienced neurosurgeons within our department (A.B.S. and R.S.). For EEA, all surgeries were performed by a single surgeon (RS).
The clinical reports of all subjects were assessed pre-and postoperatively, encompassing demographic information, clinical symptoms, imaging results, ophthalmological evaluations, operative details, and any complications. Both computed tomography (CT) and magnetic resonance imaging (MRI) data were used for preoperative assessment, intraoperative guidance, and postoperative outcomes.
Radiological assessment
The tumor volume was determined using the formula: tumor volume (in cubic centimeters, cm3) = (anteroposterior × coronal × craniocaudal)/2. This calculation assumes the tumor’s shape resembles a rough sphere. The degree of tumor removal was assessed based on surgical records and postoperative MRI scans. Gross total resection (GTR) was defined as the absence of any residual tumor on the postoperative imaging. The presence of tumor remnants characterized subtotal resection.
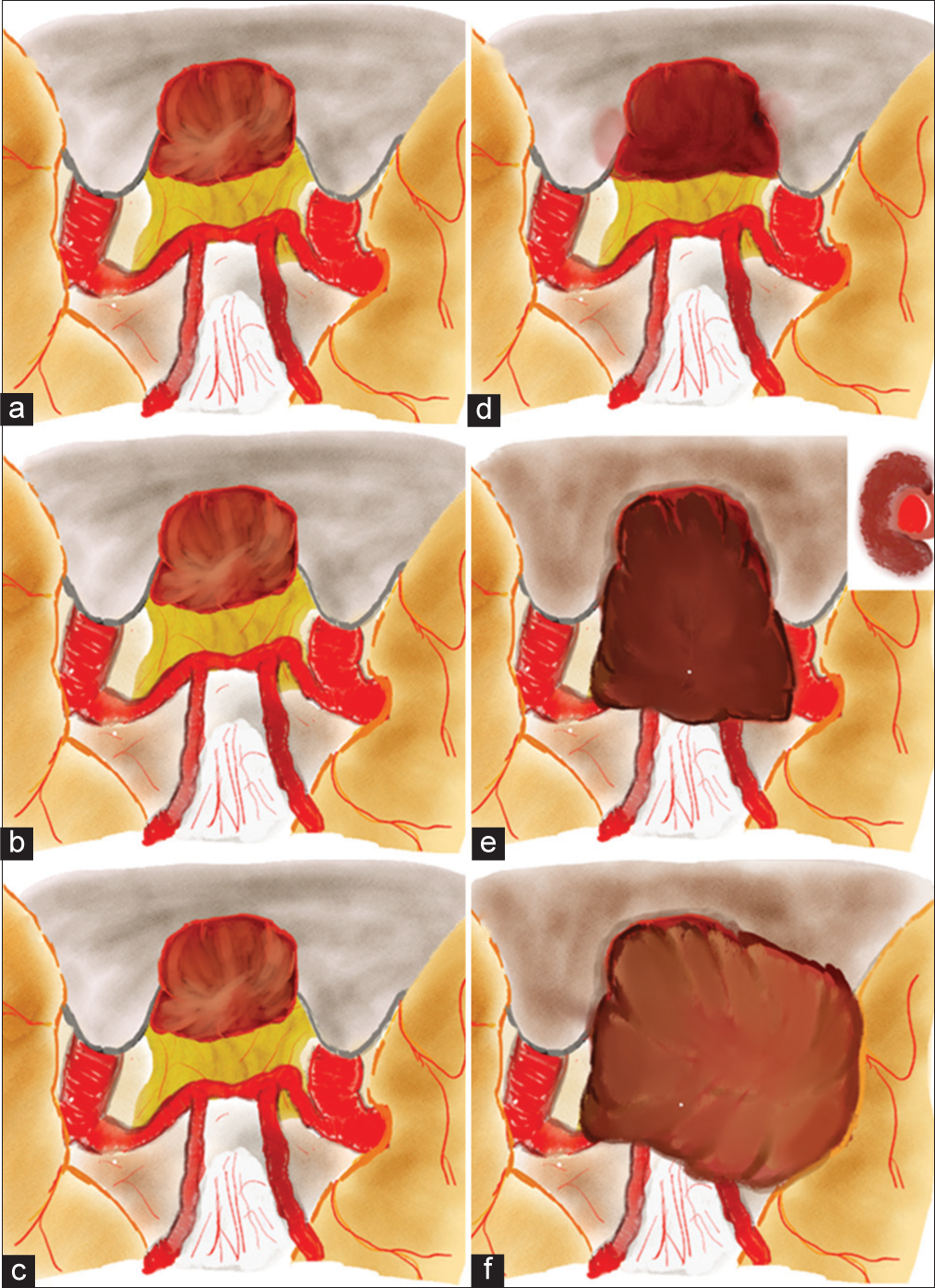
The refined Magill-McDermott (M-M) scale was used to classify optic canal invasion and arterial encasement [
Figure 1:
The illustration of classification in our study, adopted from the refined Magill-McDermott scale. (a,b,c) The drawings of tuberculum sellae meningioma without the involvement of optic canal, arterial encasement, and lateral extension. (d) Optic canal invasion. (e) Arterial encasement > 1800 of either internal carotid artery, middle cerebral artery, or anterior cerebral artery. (f) Lateral extension beyond the anterior clinoid process.
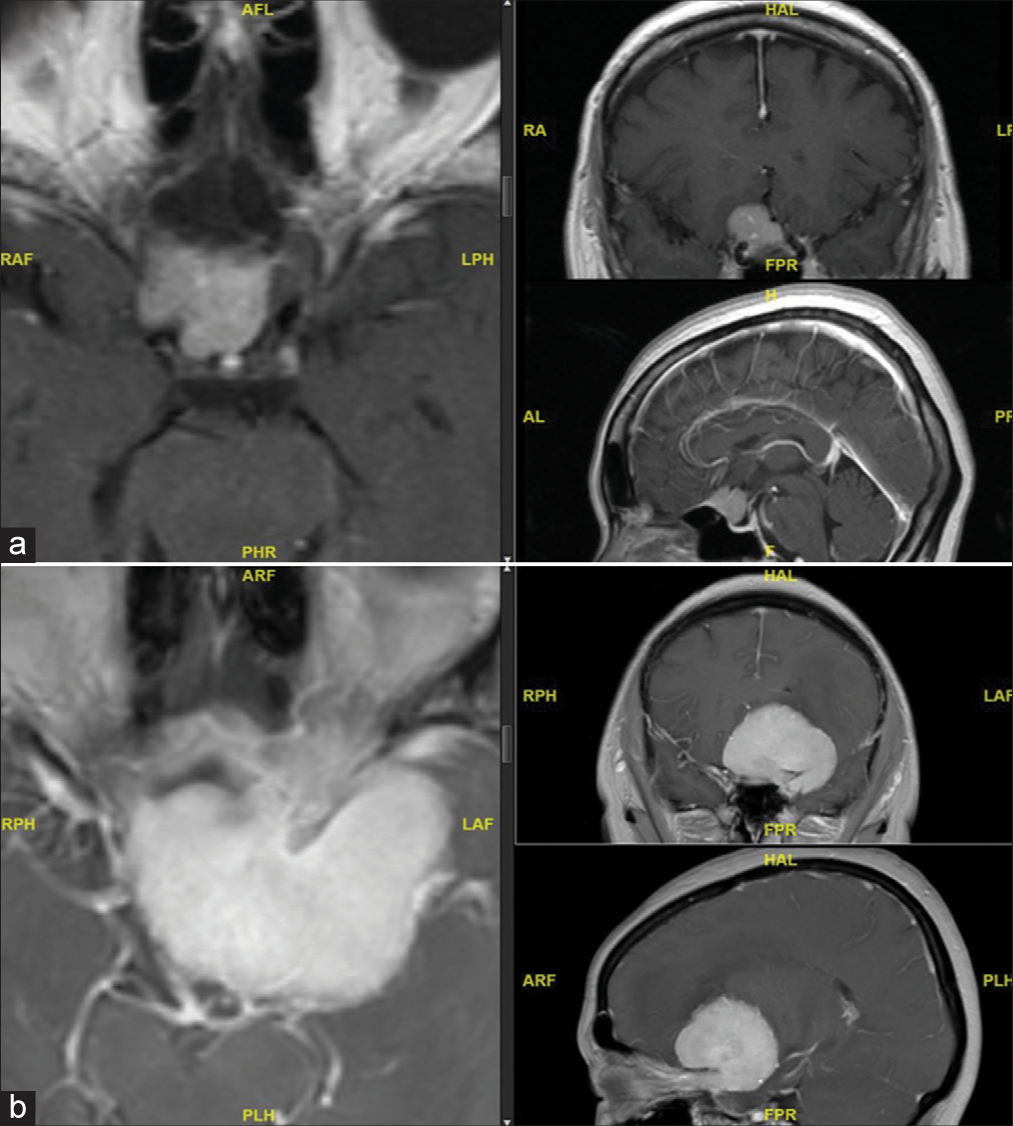
Figure 2:
Representative images from patients with tuberculum sellae meningioma. (a) The suitable candidate for an endoscopic endonasal approach – is a small tumor, with minimal arterial encasement and no lateral extension beyond the clinoid process. (b) The suitable candidate for transcranial approach – a large tumor, extensive arterial encasement, and lateral extension beyond the clinoid process.
Study bias
This study is constrained by selection and observer biases. In addition, observer bias is a limitation, as only data documented in the electronic medical records were available for analysis.
Statistical analysis
Statistical analysis was conducted using GraphPad Prism 8.0. Descriptive statistics, including patient demographics, were presented in tabular format. Continuous variables were reported as means with standard deviations, while categorical variables were expressed as percentages. Group comparisons were performed using the Student’s t-test for continuous variables and the Chi-square test for categorical variables. P < 0.05 was considered indicative of a statistically significant difference.
RESULTS
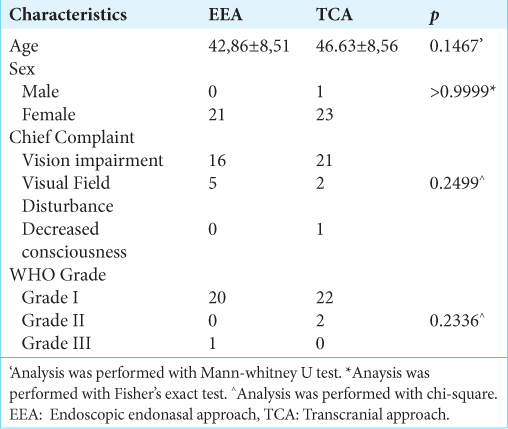
Clinical characteristics
A total of 45 patients were included in this study, with 21 patients undergoing EEA and 24 patients undergoing TCAs. There was no significant difference in age, sex, and presenting symptoms in both groups, with the majority of patients being middle-aged females. The chief complaint in our series was mostly related to vision impairment (n = 37/45), followed by visual field disturbance (7/45), and one patient had decreased consciousness due to intracranial hypertension. All patients were pathologically confirmed as meningioma, with the majority of cases (n = 42/45) being WHO grade I. The clinical data are presented in
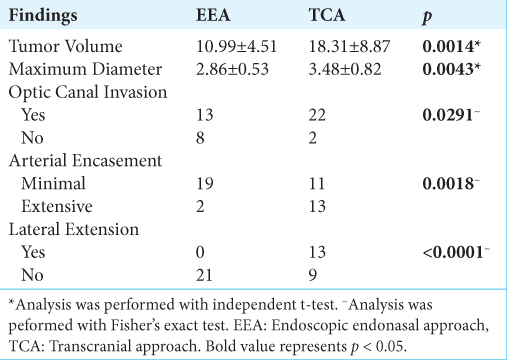
Radiological findings
In this series, the mean volume of the tumor was 10.99 ± 4.51 cm3 in the EEA group and 18.31 ± 8.87 cm3 (P = 0.0014) in the TCA group. Similarly, there was a significant difference in tumor diameter, with measurements of 2.86 ± 0.53 cm in the EEA group and 3.48 ± 0.82 cm in the TCA group (P = 0.0043). Moreover, the patients in the EEA group exhibited a significantly lower rate of optic canal invasion, with 13 out of 21 patients (13/21), compared to patients in the TCA group, where 22 out of 24 patients (22/24) had optic canal invasion (P = 0.0291). In addition, the EEA group had a lower rate of arterial encasement, with 19 out of 21 patients showing minimal encasement and two out of 21 patients displaying extensive encasement. On the contrary, the TCA group had 11 out of 24 patients with minimal encasement and 13 out of 24 patients with extensive encasement (P = 0.0018). All patients in the EEA group showed no lateral extension beyond the clinoid process. Conversely, in the TCA group, 13 out of 24 had lateral extension (P < 0.0001). The radiological assessment is presented in
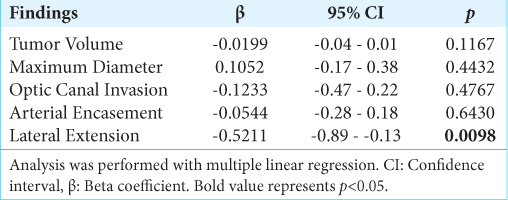
Then, we conducted a multivariate analysis to ascertain which radiological factors are crucial in determining the appropriate surgical approach for patients with TSMs. Our analysis confirmed that lateral extension beyond the clinoid process precludes the utilization of the EEA for treating TSMs in our series [P = 0.0098,
Postoperative outcomes
In this series, the rate of achieving gross total resection (GTR) was higher in the EEA group (17/21) than in the TCA group (9/24) (P = 0.0032). Among the 44 patients with vision impairment, vision restoration or stabilization was reported in 36 (81.82%) patients, including 14 (58.33%) in the TCA group and 17 (80.95%) in the EEA group. There was no statistically significant difference (P > 0.05) between TCA and EEA groups in vision restoration or stabilization rates.
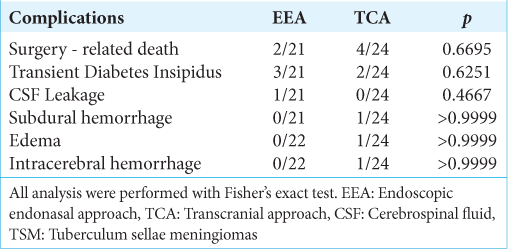
In our study, there was 1 patient (4.76%) experienced postoperative cerebrospinal fluid leakage in the EEA group and required secondary surgery to repair the dural leakage. Whereas none of the 24 patients in the TCA group experienced cerebrospinal fluid leakage. Transient diabetes insipidus occurred in three out of 21 patients with EEA and two out of 24 patients with TCA (P = 0.6521). There was a lower rate of surgery-related death in the EEA group (2/21) compared to the TCA group (4/24), all of them related to injury to the major arteries. In addition, we also observed other complications, including subdural hemorrhage (one in TCA), edema (one in TCA), and intracerebral hemorrhage (one in TCA). However, there was no significant difference in postoperative complications rate between the EEA and TCA (P > 0.05). The data are presented in
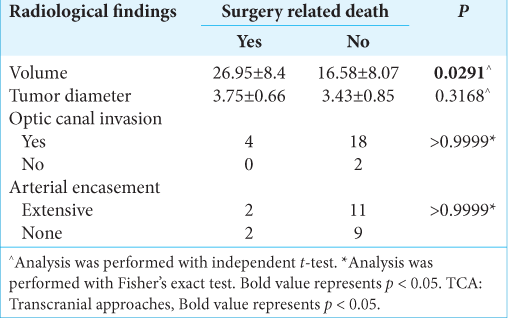
We subsequently performed an analysis to identify the factors associated with surgery-related death in the EEA group. In the EEA group, extensive arterial encasement was associated with surgery-related death [
DISCUSSION
TSM is a prevalent benign tumor located in the sellae region.[
Typically, TSM exhibits slow growth and may not manifest any clinical symptoms in its early stages. In our series, almost all patients presented with visual disturbances, reflecting meningioma’s growth pattern and proximity to the optic apparatus. Impaired visual acuity and visual field deficits are often reported as the clinical manifestations of TSM due to its proximity to the optic apparatus. As the tumor compresses the optic nerve or chiasm, patients may experience visual disturbances ranging from blurry vision to partial or complete vision loss or visual field disturbance.[
Surgical intervention is the optimal treatment strategy for TSM, aiming not only to remove the tumor but also to alleviate compression on critical structures and restore vision. In our series, we avoid performing EEA in TCMs with lateral extension. In the context of EEA, lateral extension beyond the clinoid process presents a challenge. This extension can involve critical structures such as the cavernous sinus, optic nerve, and ICA, making complete resection through an endonasal route difficult or impossible without risking damage to these structures. Therefore, in cases where lateral extension beyond the clinoid process is present, EEA surgery for TSM is not advisable due to the increased risk of complications and inadequate tumor resection. Instead, traditional TCAs may be preferred for accessing and resecting tumors with lateral extension beyond the clinoid process.[
In our series, the mortality is relatively lower in the EEA group. Our subsequent analysis revealed that arterial encasement is the factor associated with surgery-related death in EEA surgery. Due to the intricate anatomy and limited working space within the narrow corridor of the sphenoid sinus, adequately accessing and safely dissecting tumors that encase major arteries can be difficult through an endonasal route.[
In our series, surgery-related deaths in TCAs were associated with large tumor sizes. A large tumor (>25 cm3) often distorts the normal architecture of the surrounding structures, which poses a significant challenge for TCA surgery in treating TSMs. The distorted anatomy complicates the surgical approach and increases the risk of damaging critical structures such as blood vessels and nerves.[
Studies have shown that early surgical intervention in TSMs can result in significant improvement or stabilization of visual deficits in a considerable number of patients.[
Recent International TSM study has reported that optic canal invasion and arterial encasement are associated with difficulty in achieving GTR either with EEA or TCAs.[
The strength of our study is the first report from a single institution with the experience of performing >20 cases for both EEA and TCA in the surgical treatment of TSM. In our study, we confirm that among all factors in the M-M scale, the arterial encasement is an important guidance for the approach. Overall, surgery may improve visual outcomes in many cases of TSM; it is important to consider individual patient factors and tailor treatment strategies based on surgical expertise, radiological assessment, and postoperative care. Several radiological parameters (lateral extension and arterial encasement) were associated as guidance for neurosurgeons in awareness of potential challenges during the surgery. Patient and surgical approach selection is crucial to minimize complications while achieving the treatment goal.
Limitation
This study is limited by observation bias and a single center. The surgeon preference bias is well reflected in our series, as all cases with lateral extension were performed transcranially. However, this situation is a common precaution for the EEA approach. In addition, the limited duration of follow-up makes it difficult to obtain the recurrence rate.
CONCLUSION
Both traditional TCAs and EEAs offer valuable options for the surgical management of TSM, each with its advantages and limitations. Based on our experiences, lateral extension and arterial encasement may guide the suitable approach, in addition to surgeon expertise and multidisciplinary considerations, with the overarching goals of achieving maximal tumor resection, preserving neurological function, and minimizing postoperative complications.
Authors’ contributions
RS, YH: Conceptualization, data curation, formal analysis, methodology, and writing; ABS, GN: Review and editing; AF: Final approval of the manuscript.
Ethical approval
The research/study was approved by the IRB at Dr. Hasan Sadikin Hospital Ethical Committee, number DP.04.03/D. XIV.2.2.1/1221/2023, dated December 20, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Carlson AP, Stippler M, Myers O. Predictive factors for vision recovery after optic nerve decompression for chronic compressive neuropathy: Systematic review and meta-analysis. J Neurol Surg B Skull Base. 2013. 74: 20-38
2. Chokyu I, Goto T, Ishibashi K, Nagata T, Ohata K. Bilateral subfrontal approach for tuberculum sellae meningiomas in long-term postoperative visual outcome. J Neurosurg. 2011. 115: 802-10
3. Duan C, Song D, Wang F, Wang Y, Wei M, Fang J. Factors influencing postoperative visual improvement in 208 patients with tuberculum sellae meningiomas. Acta Neurochir (Wien). 2024. 166: 140
4. Fukushima T, Maroon JC. Repair of carotid artery perforations during transsphenoidal surgery. Surg Neurol. 1998. 50: 174-7
5. Ganna A, Dehdashti AR, Karabatsou K, Gentili F. Fronto-basal interhemispheric approach for tuberculum sellae meningiomas; long-term visual outcome. Br J Neurosurg. 2009. 23: 422-30
6. Gardner PA, Kassam AB, Thomas A, Snyderman CH, Carrau RL, Mintz AH. Endoscopic endonasal approach for anterior cranial base and suprasellar lesions: Indications and limitations. Neurosurgery. 2009. 64: 677-89
7. Giammattei L, Starnoni D, Cossu G, Bruneau M, Cavallo LM, Cappabianca P. Surgical management of tuberculum sellae meningiomas: Myths, facts, and controversies. Acta Neurochir (Wien). 2020. 162: 631-40
8. Goel A, Muzumdar D, Desai KI. Tuberculum sellae meningioma: A report on management on the basis of a surgical experience with 70 patients. Neurosurgery. 2002. 51: 1358-63
9. Henderson F, Youngerman BE, Niogi SN, Alexander T, Tabaee A, Kacker A. Endonasal transsphenoidal surgery for planum sphenoidale versus tuberculum sellae meningiomas. J Neurosurg. 2022. 138: 1338-46
10. Karsy M, Raheja A, Eli I, Guan J, Couldwell WT. Clinical outcomes with transcranial resection of the tuberculum sellae meningioma. World Neurosurg. 2017. 108: 748-55
11. Kenawy K, Kasim AK, Almamoun MM. Tuberculum sellae meningiomas: Transcranial approaches results and complications. Open J Mod Neurosurg. 2022. 12: 67-76
12. Kozák J, Bízik I, Novotný M, Klener J. How I do it: Optic canal unroofing in surgery for tuberculum sellae meningiomas with compression of the optic nerve. Acta Neurochir (Wien). 2022. 164: 1397-400
13. Leclerc A, Gaberel T, Laville MA, Derrey S, Quintyn JC, Emery E. Predictive factors of favorable visual outcomes after surgery of tuberculum sellae meningiomas: A multicenter retrospective cohort study. World Neurosurg. 2022. 164: e557-67
14. Liu JK, Christiano LD, Patel SK, Tubbs RS, Eloy JA. Surgical nuances for removal of tuberculum sellae meningiomas with optic canal involvement using the endoscopic endonasal extended transsphenoidal transplanum transtuberculum approach. Neurosurg Focus. 2011. 30: E2
15. Magill ST, Morshed RA, Lucas CG, Aghi MK, Theodosopoulos PV, Berger MS. Tuberculum sellae meningiomas: Grading scale to assess surgical outcomes using the transcranial versus transsphenoidal approach. Neurosurg Focus. 2018. 44: E9
16. Magill ST, Schwartz TH, Couldwell WT, Gardner PA, Heilman CB, Sen C. International tuberculum sellae meningioma study: Preoperative grading scale to predict outcomes and propensity-matched outcomes by endonasal versus transcranial approach. Neurosurgery. 2023. 93: 1271-84
17. Magill ST, Schwartz TH, Couldwell WT, Gardner PA, Heilman CB, Sen C. International tuberculum sellae meningioma study: Surgical outcomes and management trends. Neurosurgery. 2023. 93: 1259-70
18. Mahmoud M, Nader R, Al-Mefty O. Optic canal involvement in tuberculum sellae meningiomas: Influence on approach, recurrence, and visual recovery. Neurosurgery. 2010. 67: ons108-18 discussion ons118-9
19. Malueka RG, Hartanto RA, Setyawan NH, Fauzi DN, Damarjati KR, Rismawan A. Association of hormonal contraception with meningioma location in Indonesian patiens. Asian Pac J Cancer Prev. 2022. 23: 1047-51
20. Martinez-Perez R, Kortz MW, Florez-Perdomo W, Ung TH, Youssef AS. Endocrinological outcomes after transcranial resection of tuberculum sellae meningiomas: A systematic review and meta-analysis. Neurosurg Rev. 2022. 45: 1965-75
21. Nakamura M, Roser F, Struck M, Vorkapic P, Samii M. Tuberculum sellae meningiomas: Clinical outcome considering different surgical approaches. Neurosurgery. 2006. 59: 1019-29
22. Portet S, Banor T, Bousquet J, Simonneau A, Flores M, Ingrand P. New insights into expression of hormonal receptors by meningiomas. World Neurosurg. 2020. 140: e87-96
23. Qian K, Nie C, Zhu W, Zhao H, Zhang F, Wang H. Surgical management of tuberculum sellae meningioma: Transcranial approach or endoscopic endonasal approach?. Front Surg. 2022. 9: 979940
24. Sankhla SK, Jayashankar N, Khan MA, Khan GM. Surgical management of tuberculum sellae meningioma: Our experience and review of the literature. Neurol India. 2021. 69: 1592-600
25. Silveira-Bertazzo G, Manjila S, London NR, Prevedello DM. Techniques and challenges of the expanded endoscopic endonasal access to the ventrolateral skull base during the “farmedial” and “extreme medial” approaches. Acta Neurochir (Wien). 2020. 162: 597-603
26. Troude L, Boucekine M, Baucher G, Farah K, Boissonneau S, Fuentes S. Ipsilateral vs controlateral approach in tuberculum sellae meningiomas surgery: A retrospective comparative study. Neurosurg Rev. 2021. 44: 3581-91
27. Xu Y, Nunez MA, Mohyeldin A, Vigo V, Mao Y, Cohen-Gadol AA. Microsurgical anatomy of the dorsal clinoidal space: Implications for endoscopic endonasal parasellar surgery. J Neurosurg. 2022. 137: 1418-30
28. Yamaguchi R, Tosaka M, Miyagishima T, Osawa T, Horiguchi K, Honda F. Sagittal bending of the optic nerve at the entrance from the intracranial to the optic canal and ipsilateral visual acuity in patients with sellar and suprasellar lesions. J Neurosurg. 2019. 134: 180-8
29. Youngerman BE, Banu MA, Gerges MM, Odigie E, Tabaee A, Kacker A. Endoscopic endonasal approach for suprasellar meningiomas: Introduction of a new scoring system to predict extent of resection and assist in case selection with long-term outcome data. J Neurosurg. 2020. 135: 113-25