- Division of Neurosurgery, P.O. Santa Maria Delle Grazie, Naples, Italy,
- Faculty of Medicine, University of Geneva, Geneva, Switzerland
- Department of Neurology, Neurosurgery, Acute Medicine, Intensive Care Unit, Division of Neuroradiology (MIV), and EEG and Epilepsy Unit (SV), Geneva University Hospitals, Geneva, Switzerland.
Correspondence Address:
Ciro Mastantuoni, Division of Neurosurgery, P.O. Santa Maria Delle Grazie, Naples, Italy.
DOI:10.25259/SNI_139_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ciro Mastantuoni1, Nour-Louise Martin2, Enrico Tessitore3. Symptomatic lumbar Tarlov cyst resolution after computed tomography-guided percutaneous trans-sacral fibrin glue intracystic injection: A case report and literature review. 19-Apr-2024;15:137
How to cite this URL: Ciro Mastantuoni1, Nour-Louise Martin2, Enrico Tessitore3. Symptomatic lumbar Tarlov cyst resolution after computed tomography-guided percutaneous trans-sacral fibrin glue intracystic injection: A case report and literature review. 19-Apr-2024;15:137. Available from: https://surgicalneurologyint.com/surgicalint-articles/12863/
Abstract
Background: Perineural Tarlov cysts are extrathecal cerebrospinal fluid-filled cavities in the perineural recesses around dorsal spinal nerve roots. They are mostly asymptomatic but may occasionally cause back pain, radiculopathy, neurological deficits, and idiopathic intracranial hypotension.
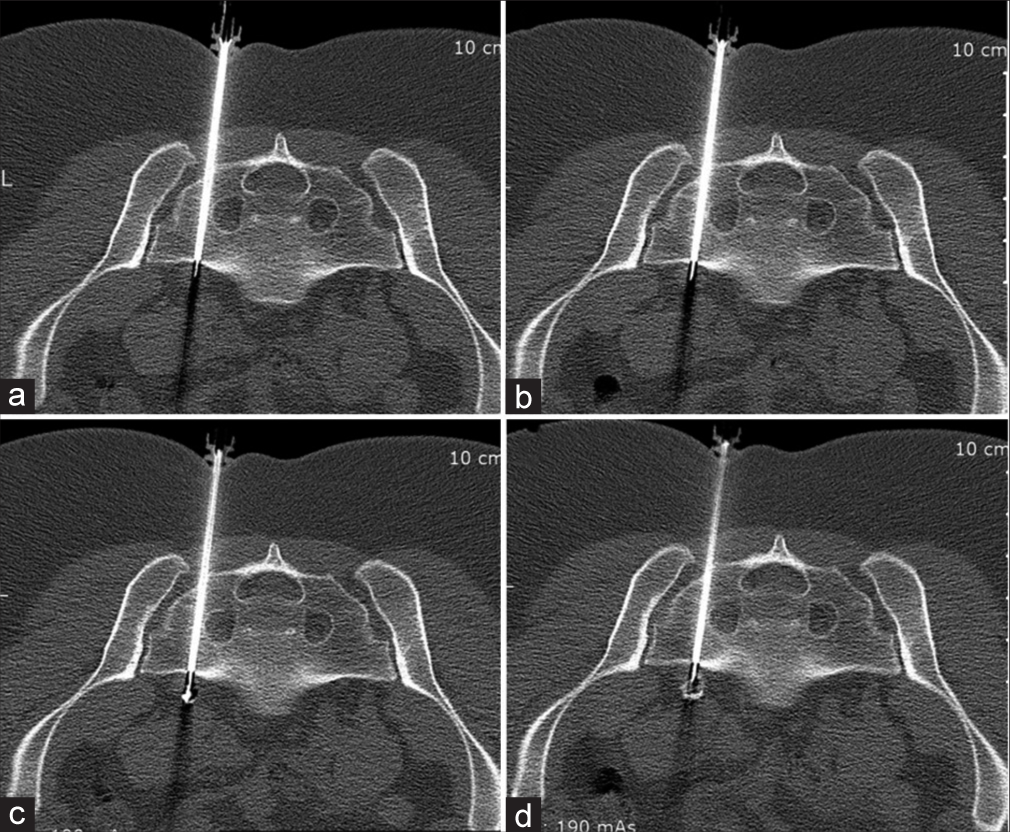
Case Description: A 40-year-old female presented with a partial left foot drop attributed to a symptomatic L5 Tarlov cyst with an extension anterior to the sacrum. Following a computed tomography (CT)-guided percutaneous trans-sacral fibrin glue intracystic injection, the cyst was markedly reduced in size, and the patient’s symptoms resolved.
Conclusion: Rarely, patients may present with symptomatic lumbar Tarlov cysts located anterior to the sacrum. Here, we present a patient whose left-sided foot drop resolved following the percutaneous trans-sacral CT-guided L5 intracyst injection of fibrin glue.
Keywords: Computed tomography-guided (CT-guided), Percutaneous, Tarlov cyst, Radicular pain, Fibrin glue
INTRODUCTION
A 40-year-old female presented with a left L5 partial foot drop attributed to a L5 Tarlov cyst extending anterior to the sacrum. Following computed tomography (CT)-guided percutaneous trans-sacral fibrin glue intracystic injection, the cyst was markedly reduced in size, and the patient’s symptoms resolved.
CASE DESCRIPTION
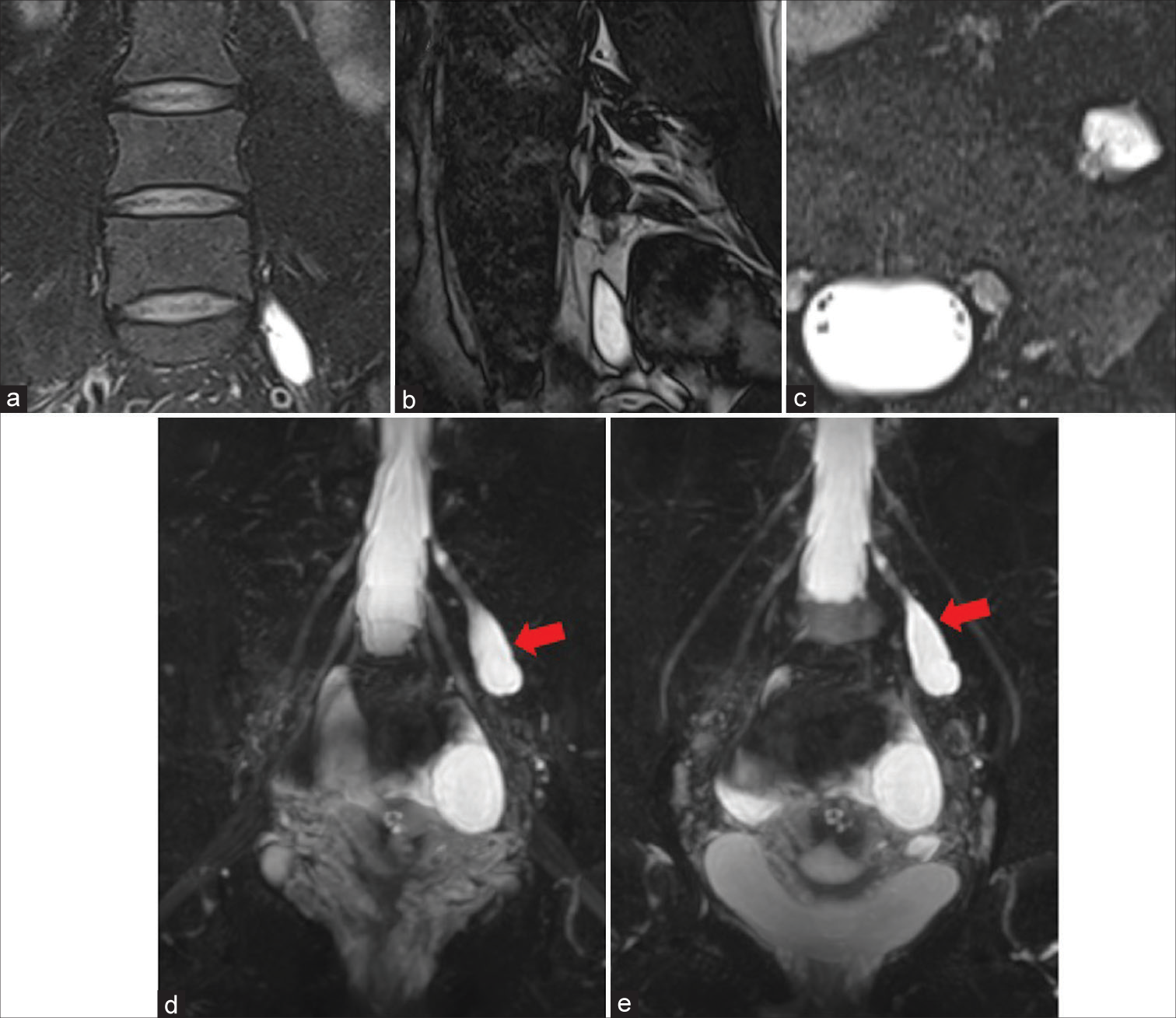
A 40-year-old female presented with a left partial foot drop for a 2-year duration. The contrast-enhanced magnetic resonance imaging (MRI) showed a small left L5 peri-radicular cyst that extended into the extraforaminal space and presacral region [
Figure 1:
Coronal (a), sagittal (b), and axial (c) views showing the perineural cyst and its relationship with the neighboring structures; (d and e) magnetic resonance imaging with fiber-tracking sequences displaying a small left L5 peri-radicular cyst at filled with cerebrospinal fluid and thus in communication with the subarachnoid space (red arrows). This finding confirms the diagnosis of the Tarlov cyst.
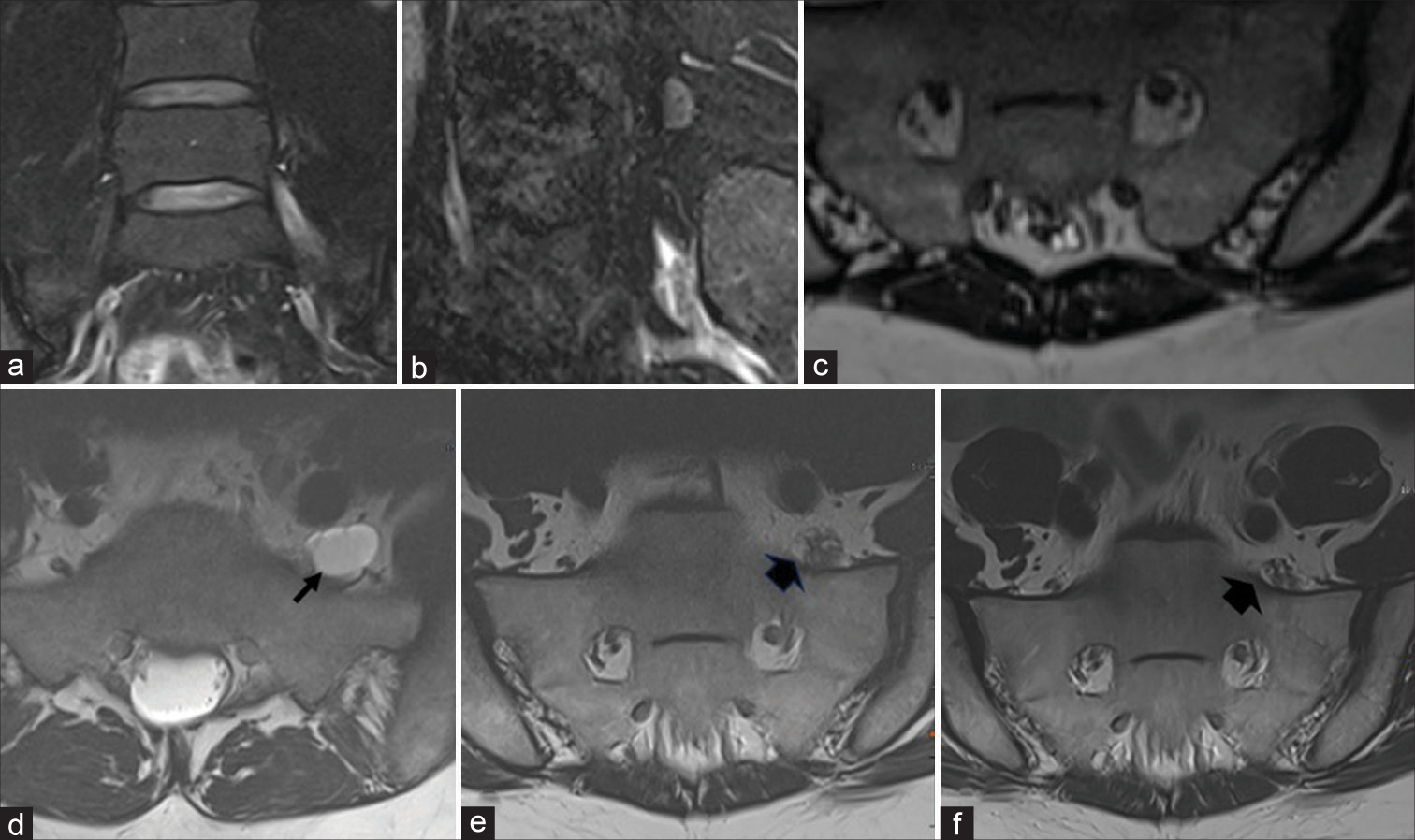
Figure 3:
(a-c) A 2-month post-procedure magnetic resonance imaging (MRI) displaying a complete resolution of the pre-sacral component of the cyst and a size reduction of the nerve root and the cyst passing from 18 to 12 mm. Coronal (a) and sagittal (b) and axial (c) views; (d-f) comparison between T2-weighted MRI, axial sequences, (d) before the procedure, (e) at two months follow-up and (f) at nine months follow-up. (d) The L5 peri-radicular cyst extending from the preforaminal recessal level to the presacral region is shown before the procedure (black arrow); (e) MRI at two months follows, showing the complete resolution of the pre-sacral component of the cyst and a size reduction of the nerve root (black arrowhead); (f) 9 months follow-up: the MRI showed the complete disappearance of Tarlov’s cyst with L5 G root remaining thickened without edematous suffering (black arrowhead).
DISCUSSION
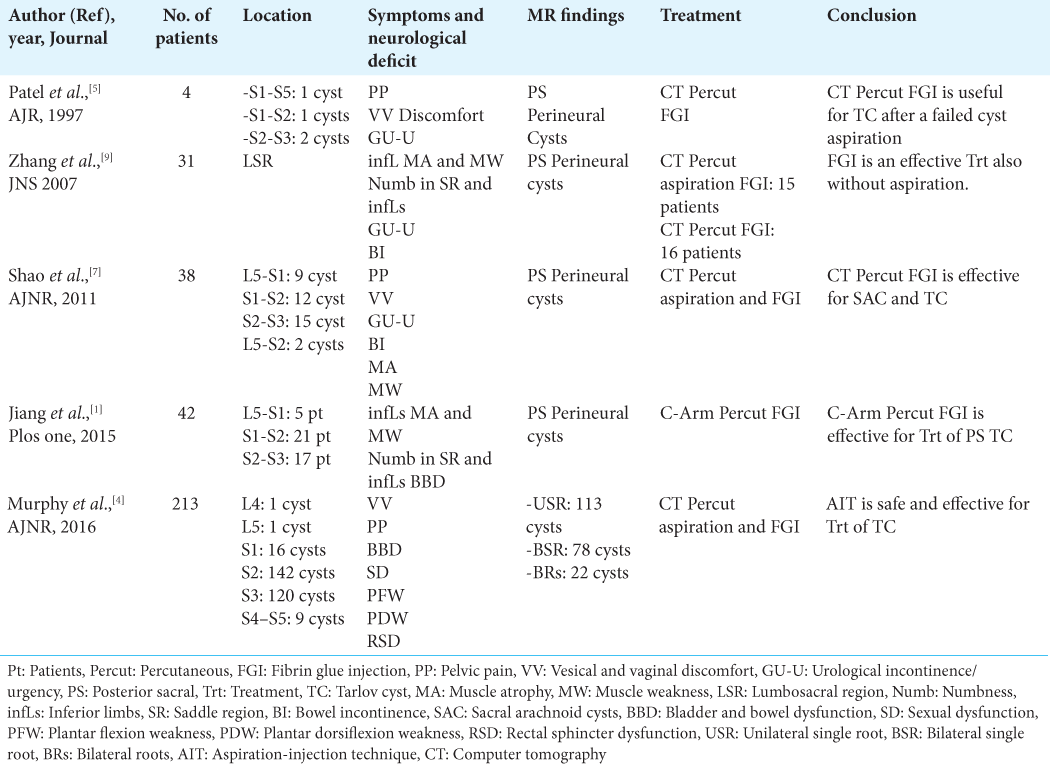
Minimally invasive percutaneous techniques utilized to treat TC may include cyst aspiration or two-needle-aspiration and fibrin glue injection under CT guidance.[
CONCLUSION
A 40-year-old female presented with the 2-year onset of a partial left foot drop attributed to an MR-documented L5 Tarlov cyst extending anterior to the sacrum. Following a CT-guided percutaneous trans-sacral fibrin glue intracystic injection, the cyst largely resolved, and the patient became asymptomatic.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Jiang W, Qiu Q, Hao J, Zhang X, Shui W, Hu Z. Percutaneous fibrin gel injection under C-arm fluoroscopy guidance: A new minimally invasive choice for symptomatic sacral perineural cysts. PLoS One. 2015. 10: e0118254
2. Klepinowski T, Orbik W, Sagan L. Global incidence of spinal perineural Tarlov’s cysts and their morphological characteristics: A meta-analysis of 13,266 subjects. Surg Radiol Anat. 2021. 43: 855-63
3. Murphy K, Nasralla M, Pron G, Almohaimede K, Schievink W. Management of Tarlov cysts: An uncommon but potentially serious spinal column disease-review of the literature and experience with over 1000 referrals. Neuroradiology. 2024. 66: 1-30
4. Murphy K, Oaklander AL, Elias G, Kathuria S, Long DM. Treatment of 213 patients with symptomatic Tarlov cysts by Ct-guided percutaneous injection of fibrin sealant. AJNR Am J Neuroradiol. 2016. 37: 373-9
5. Patel MR, Louie W, Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am J Roentgenol. 1997. 168: 367-70
6. Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol. 1994. 15: 293-7 discussion 98-9
7. Shao Z, Wang B, Wu Y, Zhang Z, Wu Q, Yang S. CT-guided percutaneous injection of fibrin glue for the therapy of symptomatic arachnoid cysts. AJNR Am J Neuroradiol. 2011. 32: 1469-73
8. Tracz J, Judy BF, Jiang KJ, Caraway CA, Yang W, Sobreira NL. Interventional approaches to symptomatic Tarlov cysts: A 15-year institutional experience. J Neurointerv Surg. 2023. p. ahead of print
9. Zhang T, Li Z, Gong W, Sun B, Liu S, Zhang K. Percutaneous fibrin glue therapy for meningeal cysts of the sacral spine with or without aspiration of the cerebrospinal fluid. J Neurosurg Spine. 2007. 7: 145-50