- Department of Neurosurgery, Carle Illinois College of Medicine, University of Illinois Urbana-Champaign,
- Department of Neurosurgery, Carle Neuroscience Institute, Carle Foundation Hospital,
- Department of Electrical and Computer Engineering, University of Illinois Urbana-Champaign,
- Department of Neurosurgery, Carle Illinois College of Medicine, Urbana, Illinois, United States.
Correspondence Address:
Paul Arnold, Department of Neurosurgery, Carle Illinois College of Medicine, Urbana, Illinois, United States.
DOI:10.25259/SNI_88_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Darrion Bo-Yun Yang1, James Harms2, Ravishankar K. Iyer3, Paul Arnold4. Synovial cysts at the cervicothoracic junction: Illustrative series of three cases. 08-Jun-2023;14:196
How to cite this URL: Darrion Bo-Yun Yang1, James Harms2, Ravishankar K. Iyer3, Paul Arnold4. Synovial cysts at the cervicothoracic junction: Illustrative series of three cases. 08-Jun-2023;14:196. Available from: https://surgicalneurologyint.com/surgicalint-articles/12359/
Abstract
Background: Spinal synovial cysts are an uncommon pathology, estimated to affect 0.65–2.6% of the population. Cervical spinal synovial cysts are even rarer, accounting for only 2.6% of spinal synovial cysts. They are more commonly found in the lumbar spine. When they occur, they can compress the spinal cord or surrounding nerve roots resulting in neurological symptoms, particularly when they increase in size. Decompression and cyst resection are the most common treatment and typically result in resolution of symptoms.
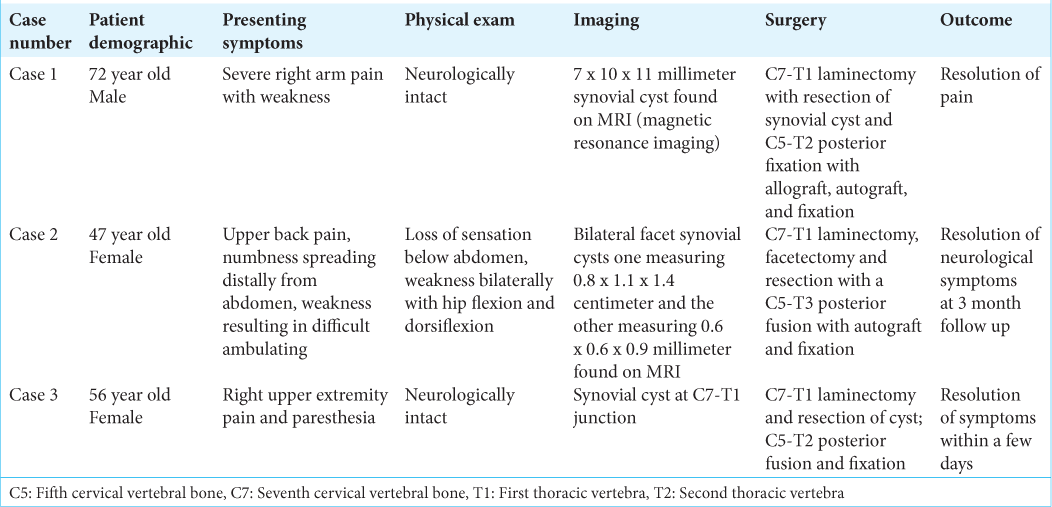
Methods: The authors present three cases of spinal synovial cysts occurring at the C7–T1 junction. They occurred in patients aged 47, 56, and 74, respectively, and presented with symptoms of pain and radiculopathy. Diagnosis was made with computed tomography (CT) scan and magnetic resonance imaging (MRI). The cysts were managed with laminectomy, resection, and fusion.
Results: All patients reported full resolution of symptoms. There were no intra or postoperative complications.
Conclusion: Cervical spinal synovial cysts are an uncommon cause of radiculopathy and pain in the upper extremities. They can be diagnosed through CT scans and MRI, and treatment with laminectomy, resection, and fusion results in excellent outcomes.
Keywords: Laminectomy, Spinal synovial cysts, Spine surgery
INTRODUCTION
Synovial cysts are extradural soft-tissue masses that arise from extrusion of the synovium through a defect in the joint capsule.[
We present three cases of synovial cervical spinal cysts emerging from the C7–T1 facet joint treated with surgical resection, laminectomy, and fusion. Two are unilateral, while one was bilateral. All patients were followed for a minimum of 1 year after surgery [
MATERIALS AND METHODS
A 47-year-old woman presenting to the emergency room with a 4-day history of upper back pain and 1 day with numbness spreading distally from the abdomen and weakness resulting in some difficulty ambulating.
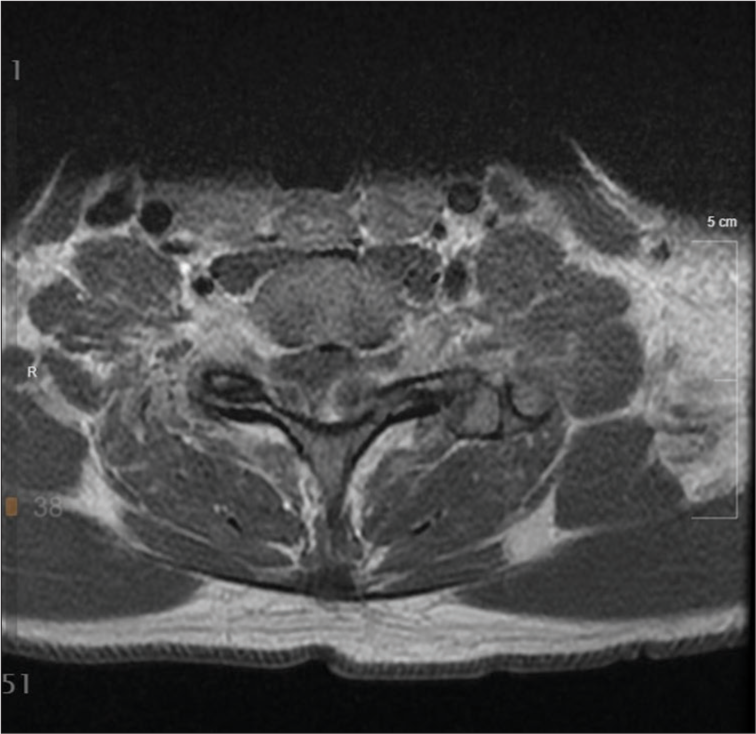
Her physical examination showed loss of sensation below her abdomen and weakness bilaterally in hip flexion and dorsiflexion bilaterally. On magnetic resonance imaging (MRI), bilateral synovial cysts at the C7–T1 junction were found [
The cyst was treated surgically with a C7–T1 laminectomy, facetectomy, and resection with a C5–T3 posterior fusion with autograft and fixation. The large synovial cyst was encountered in the left facet joint and opened. As much as possible was resected through the foramen in the C7–T1 area. Further bone was removed to allow room for the nerve root and to allow dissection of the smaller cyst.
RESULTS
Immediately after surgery, the patient reported improvement in function. Three-month postoperatively, the patient reported resolution of neurological symptoms. Her weakness resolved and she was able to ambulate normally. Anteroposterior and lateral X-rays 1 year after surgery show fusion and stable hardware placement [
All three patients recovered fully, with no evidence of cyst recurrence at 1 year after surgery [
DISCUSSION
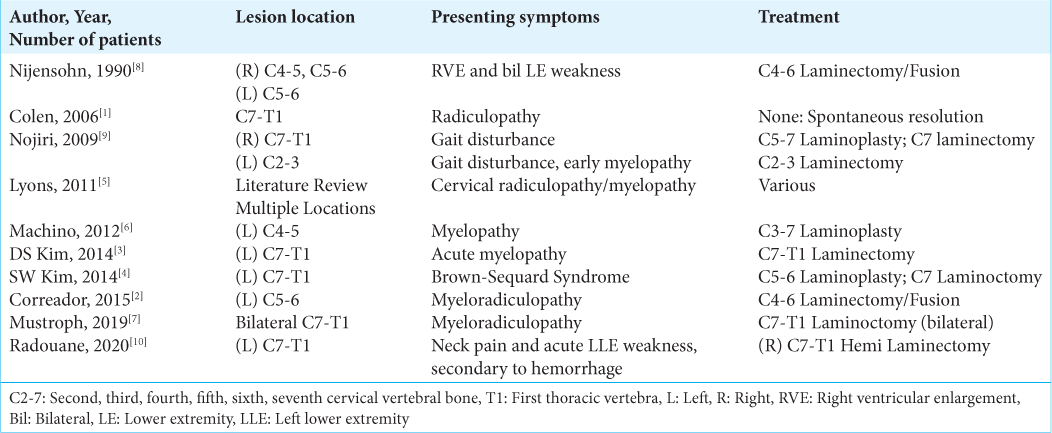
Cervical synovial cysts in the C7–T1 junction are rare, making up an estimated 2.6% of all synovial cysts found in the spine. Machino et al. found that only 51 cases reported in the past 20 years.[
The etiology of cervical spinal cysts is uncertain, but they are often associated with trauma, spinal surgery, hypermobility, or inflammatory disorders such as rheumatoid arthritis.[
Patients with spinal synovial cysts also present with variable complaints. Because synovial cysts are slow growing, symptoms often do not appear until the cyst grows large enough to compress the spinal cord or the surrounding nerve roots. However, the cysts may undergo sudden changes, especially if they are exposed to stress. Synovial cysts have been known to spontaneously resolve,[
Surgery has been shown to be an effective treatment for synovial cysts causing symptomatic compression of the spinal cord or associated nerves. Decompressive laminectomy is most performed, with excision and removal of the synovial cyst.[
CONCLUSION
We present three cases of cervical spinal synovial cysts at the C7–T1 junction. It is an uncommon pathology, and little is known about the etiology. All three were treated with decompressive laminectomy and fixation leading to resolution of symptoms.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Colen CB, Rengachary S. Spontaneous resolution of a cervical synovial cyst. Case illustration. J Neurosurg Spine. 2006. 4: 186
2. Corredor JA, Quan G. Cervical synovial cyst causing cervical radiculomyelopathy: Case report and review of the literature. Global Spine J. 2015. 5: e34-8
3. Kim DS, Yang JS, Cho YJ, Kang SH. Acute myelopathy caused by a cervical synovial cyst. J Korean Neurosurg Soc. 2014. 56: 55-7
4. Kim SW, Ju CI, Kim HS, Kim YS. Brown-séquard syndrome caused by a cervical synovial cyst. J Korean Neurosurg Soc. 2014. 55: 215-7
5. Lyons MK, Birch BD, Krauss WE, Patel NP, Nottmeier EW, Boucher OK. Subaxial cervical synovial cysts: Report of 35 histologically confirmed surgically treated cases and review of the literature. Spine (Phila Pa 1976). 2011. 36: E1285-9
6. Machino M, Yukawa Y, Ito K, Kato F. Cervical degenerative intraspinal cyst: A case report and literature review involving 132 cases. BMJ Case Rep. 2012. 2012: bcr2012007126
7. Mustroph ML, Cerecedo-Lopez CD, Groff M, Zaidi HA. Bilateral synovial cysts as a rare cause of myelopathy in a 38-year-old woman. Cureus. 2019. 11: e5377
8. Nijensohn E, Russell EJ, Milan M, Brown T. Calcified synovial cyst of the cervical spine: CT and MR evaluation. J Comput Assist Tomogr. 1990. 14: 473-6
9. Nojiri H, Sakuma Y, Uta S. Degenerative intraspinal cyst of the cervical spine. Orthop Rev (Pavia). 2009. 1: e17
10. Radhouane K, Dridi H, Mansouri N, Yedeas MD, Harbaoui A, Chkili R. Hemorrhagic synovial cyst: An unexpected cause of acute cervical spinal cord compression. Case report. Int J Surg Case Rep. 2020. 77: 527-30