- Department of Neurosurgery, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom.
- Department of Colorectal Surgery, Warrington and Halton Foundation Trust, Warrington, United Kingdom.
- Department of Data Science, National Health Service (NHS) Northern Care Alliance, Manchester, United Kingdom.
- Department of Data Science, College of Letters and Sciences, University of California, Berkeley, United Kingdom.
- Department of Neurosurgery, Manchester Centre for Clinical Neurosciences, Salford Royal Hospital, Salford, United Kingdom.
Correspondence Address:
Sayan Biswas, Department of Neurosurgery, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom.
DOI:10.25259/SNI_787_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ella Snowdon1, Sayan Biswas1, Zahra R. Almansoor1, Luqman Naim Bin Aizan2, Xin Tian Chai1, Sharan Manikanda Reghunathan1, Joshua MacArthur1, Callum James Tetlow3, Ved Sarkar4, K. Joshi George5. Temporal trends in neurosurgical volume and length of stay in a public healthcare system: A decade in review with a focus on the COVID-19 pandemic. 24-Nov-2023;14:407
How to cite this URL: Ella Snowdon1, Sayan Biswas1, Zahra R. Almansoor1, Luqman Naim Bin Aizan2, Xin Tian Chai1, Sharan Manikanda Reghunathan1, Joshua MacArthur1, Callum James Tetlow3, Ved Sarkar4, K. Joshi George5. Temporal trends in neurosurgical volume and length of stay in a public healthcare system: A decade in review with a focus on the COVID-19 pandemic. 24-Nov-2023;14:407. Available from: https://surgicalneurologyint.com/surgicalint-articles/temporal-trends-in-neurosurgical-volume-and-length-of-stay-in-a-public-healthcare-system-a-decade-in-review-with-a-focus-on-the-covid-19-pandemic/
Abstract
Background: Over the past decade, neurosurgical interventions have experienced changes in operative frequency and postoperative length of stay (LOS), with the recent COVID-19 pandemic significantly impacting these metrics. Evaluating these trends in a tertiary National Health Service center provides insights into the impact of surgical practices and health policy on LOS and is essential for optimizing healthcare management decisions.
Methods: This was a single tertiary center retrospective case series analysis of neurosurgical procedures from 2012 to 2022. Factors including procedure type, admission urgency, and LOS were extracted from a prospectively maintained database. Six subspecialties were analyzed: Spine, Neuro-oncology, Skull base (SB), Functional, Cerebrospinal fluid (CSF), and Peripheral nerve (PN). Mann-Kendall temporal trend test and exploratory data analysis were performed.
Results: 19,237 elective and day case operations were analyzed. Of the 6 sub-specialties, spine, neuro-oncology, SB, and CSF procedures all showed a significant trend toward decreasing frequency. A shift toward day case over elective procedures was evident, especially in spine (P SB (tau = 0.733, P = 0.0042), functional (tau = 0.156, P = 0.0016), and PN surgeries (P neuro-oncology (tau = −0.648, P = 0.0077), SB (tau = −0.382, P = 0.012), and functional operations, a trend which remained consistent during the COVID-19 pandemic (P = 0.01). Spine remained constant across the decade while PN demonstrated a trend toward increasing LOS.
Conclusion: Most subspecialties demonstrate a decreasing LOS coupled with a shift toward day case procedures, potentially attributable to improvements in surgical techniques, less invasive approaches, and increased pressure on beds. Setting up extra dedicated day case theaters could help deal with the backlog of procedures, particularly with regard to the impact of COVID-19.
Keywords: COVID-19, Length of stay, National Health Service, Neurosurgical operations, Temporal trend analysis
INTRODUCTION
There are huge pressures on healthcare systems to deliver high-quality and efficient patient care. The volume of surgical procedures and the length of time patients spend in hospital are of vital importance for hospital administrators and clinicians. It allows for the identification of areas of improvement and allows for more efficient resource allocation.[
Due to changing demographics and advances in treatment, there have been noticeable changes in the field of neurosurgery.[
Therefore, we aimed to analyze the frequency of the most common neurosurgical procedures and the associated LOS following these surgeries over a 10-year period at a tertiary neurosurgical center in the UK. Our study investigates current practice with respect to historic volumes and LOS and also examines whether the surgical volumes have reached pre-COVID levels.
MATERIALS AND METHODS
Data source and grouping
This study was a single-center retrospective analysis of all neurosurgical operations performed at a tertiary neurosurgical center, from December 2012 to November 2022. Data on all neurosurgical cases performed during this time were exported from the trust’s database and anonymized for analysis, and therefore, the institutional review board waived the necessity for individual patient consent. A total of 33,483 procedures were identified. Data on six routinely collected variables for each operation recorded: date and time of admission, age of the patient (continuous), LOS from the start of admission to discharge in hours (continuous), type of operation (day-case, elective or non-elective), OPCS4 code (operation identifier number), and description of the procedure (the operation that was performed). A total of 631 distinct operation types were observed across all subspecialties, which were condensed into the most common operations for each subspecialty. Further, subgroup analysis was then conducted for the most common umbrella operations in each subspecialty. Elective operations were classified as operations conducted during an inpatient admission for a patient, while non-elective operations were classified as any trauma or emergency operations. Day cases were elective procedures without an overnight stay.
Exclusion criteria
For subspecialty analysis, all epidural injection procedures (which are routinely done as day cases in our institution) were removed as the short LOS would skew the analysis. Second, with the aim of removing the outliers caused by those with a long LOS, as defined by Zhao et al., 2018, we removed those with an LOS >30 days.[
Statistical analysis
Statistical analysis was performed in the R coding language (R Foundation for Statistical Computing, Vienna, Austria). Mann-Kendall (MK) analysis was used to determine if there was a statistically significant increase or decrease in either the frequency or LOS over time. Despite our observation period of 10 years, frequency analysis of each operation subtype from the initial year 2012 was removed (on a subspecialty basis) due to sparse data. For LOS analysis, median LOS was analyzed as it is less likely to be affected by outliers than the mean. Analysis of the relationship between LOS and age was assessed using Pearson’s correlation to estimate the degree of linear association between the age of patients and LOS, alongside a one-way analysis of variance and post hoc Tukey’s test when the age was split into distinct groups (<30, 31–50, 51–70, 71+). The mean rate of change of procedure frequency was compared to the change seen during COVID-19 between 2019 and 2020, using an Independent samples t-test. For all statistical analyses, P < 0.05 was considered statistically significant.
RESULTS
Total neurosurgery – including epidural injections
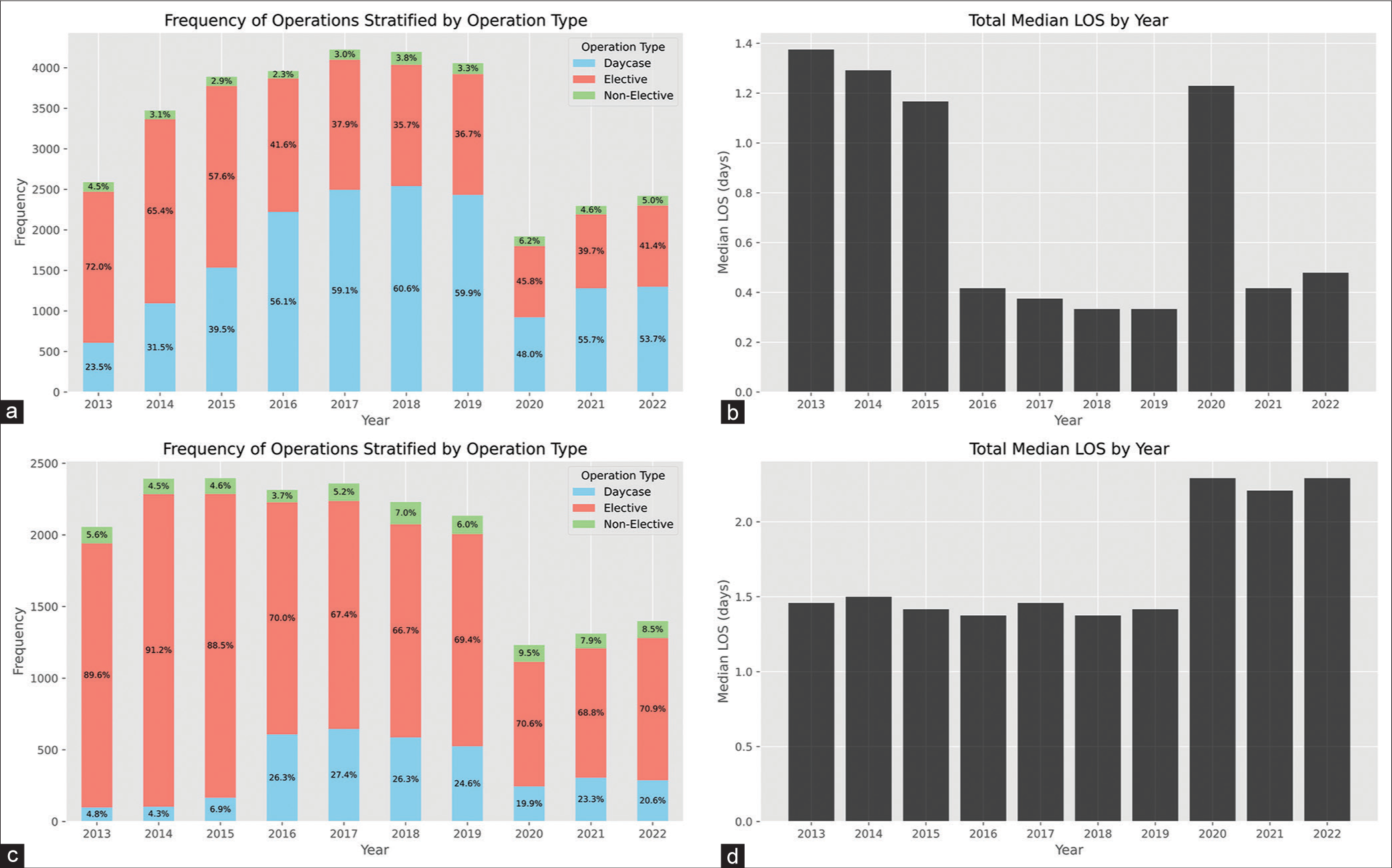
There were a total of 33,483 neurosurgical operations performed between 2012 and 2022. Of this, 16,355 were day case surgeries, 15,902 were elective, and 1226 were emergency/ non-elective. The mean patient age was 54.60 (±15.59), with a median of 55 (43–67) and a range of 18–100. Temporal distribution analysis demonstrated no overall statistically significant change in the frequency of operations performed annually (MK: tau = −0.06, P = 0.85) [
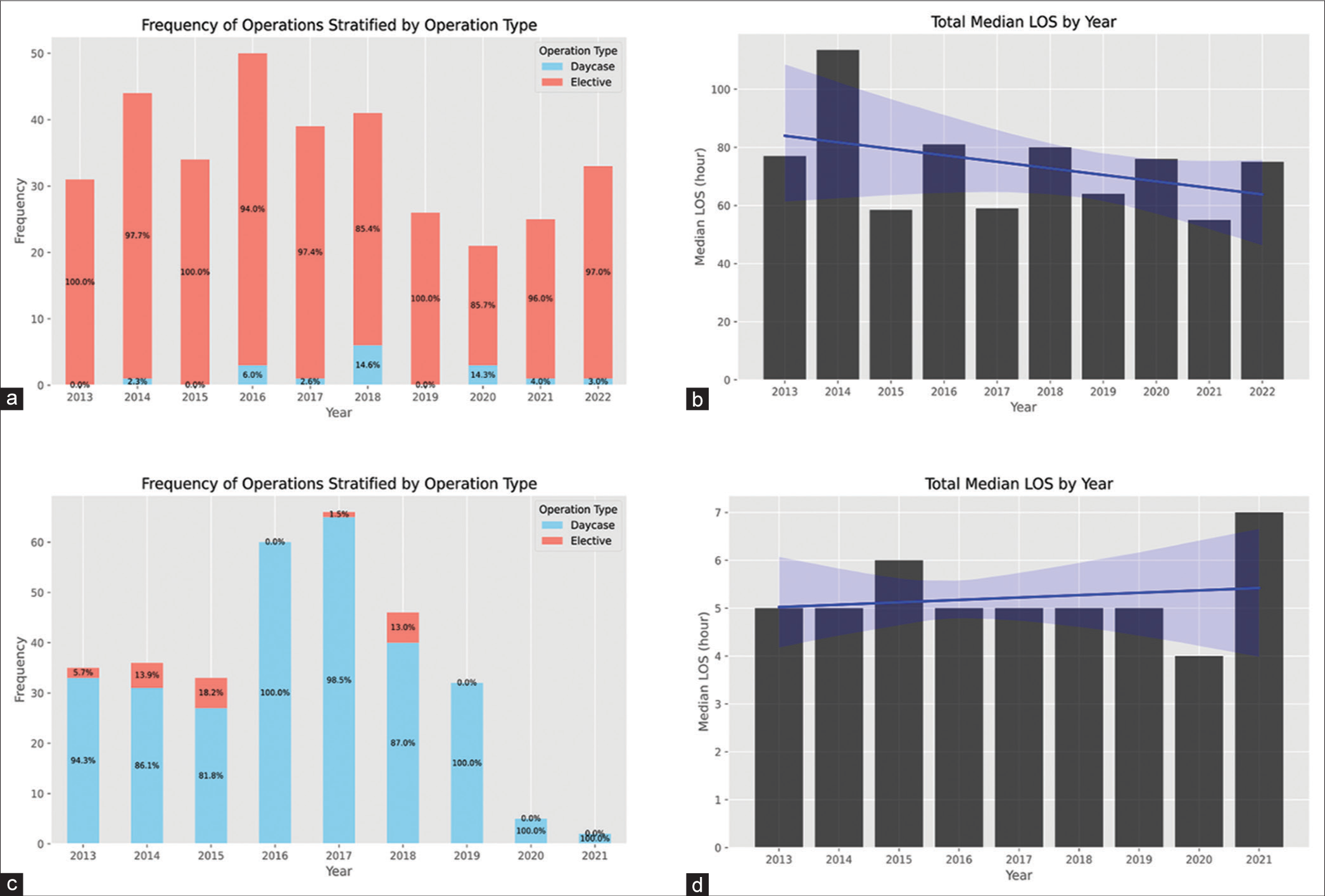
Figure 1:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022: (a) frequency of all neurosurgical operations, (b) median LOS for all neurosurgical operations, (c) frequency of all neurosurgical operations excluding spinal injections, and (d) median LOS for all neurosurgical operations excluding spinal injections.
Total neurosurgery – excluding epidural injections
Within the total procedures performed, the largest subset of procedures was day-case spinal injections (13,409 cases, accounting for nearly 40% of all cases), which included epidural injections, nerve root blocks, and facet joint injections. Exclusion of these cases revealed significant changes in the distribution of operation types with 15,802 elective cases, 3435-day case procedures, and 837 emergency/non-elective cases. Temporal distribution analysis demonstrated an overall statistically significant decrease in the frequency of operations performed annually (MK: tau = −0.51, P = 0.04) [
After removing all non-elective cases, a total of 19,237 operations were identified. Trends in operative frequency and postoperative median LOS for each neurosurgical sub-specialty and the associated common procedure types were subsequently analyzed.
Spinal surgery
Cohort demographics
A total of 11,046 spinal neurosurgery operations were performed between 2012 and 2022, with 8986 elective and 2060-day case procedures. The mean patient age was 52 (±15.08) years, with a median of 52 (41–64) and a range of 18–99. Of the 21 distinct spinal operations, only the four most common umbrella spinal operations underwent further subgroup analysis: “Excision of lumbar intervertebral disc,” “decompression of lumbar spine,” “anterior cervical discectomy and fusion,” and “lumbar fusion.”
Frequency analysis
The most frequent operation type undertaken was “excision of lumbar intervertebral disc” at 3750, followed by “decompression of lumbar spine” at 3668.
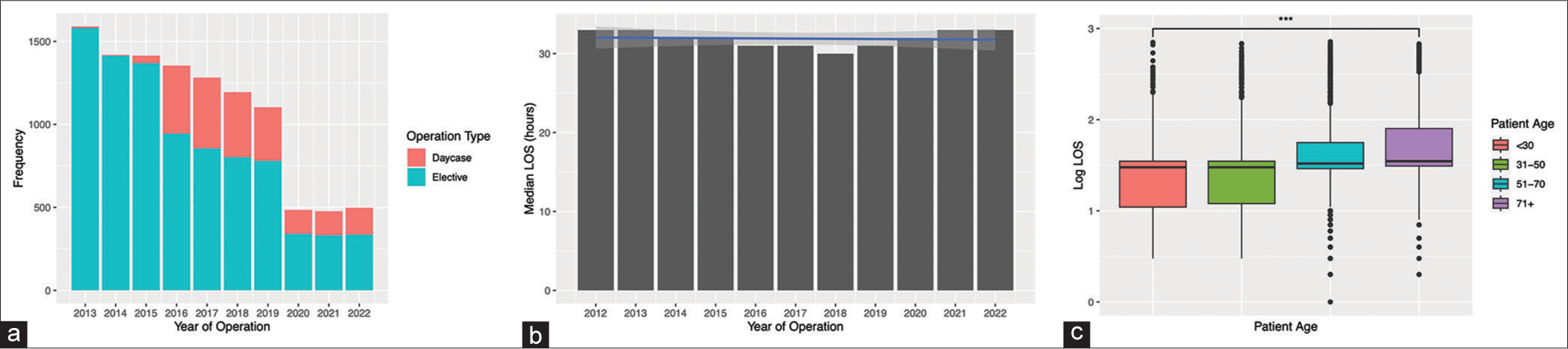
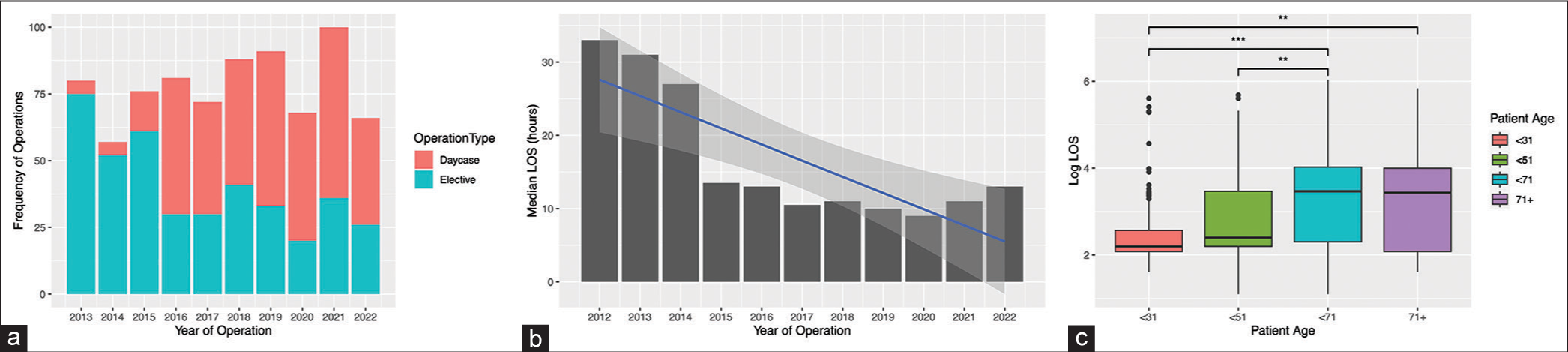
Figure 2:
Plots representing the temporal trends in operative frequency and post-operative length of stay (LOS) from 2012-2022 for all spinal operations: a) Frequency of all spinal operations split by elective and day case, b) Median LOS for all spinal operations, c) Comparing LOS and age, *** = P <0.001.
LOS analysis
Overall, the analysis showed a fairly constant LOS over time between 2012 and 2022, with no significant change in the median LOS (MK: tau = −0.103, P = 0.74), as shown in
Analysis of the most common umbrella operation types revealed that there was a statistically significant reduction in the frequency of “excision of lumbar intervertebral disc,” “decompression of lumbar spine,” and “anterior cervical discectomy and fusion.” (P < 0.05), a phenomenon further exacerbated by COVID-19. “Lumbar fusion,” however, showed no reliable trend in frequency due to drastic alterations in frequency in some years. In terms of LOS, both “lumbar decompression” and “anterior cervical discectomy and fusion” maintained a relatively static median LOS (though the latter was noted to have a slightly increasing trend), while “excision of lumbar intervertebral disc” and “lumbar fusion” demonstrated a decreasing median LOS, with the former showing a drastic drop between the years 2015 and 2016 which was accompanied by a shift to performing >50% of these as day case surgeries [Supplementary
Neuro-oncology
Cohort demographics
A total of 4088 neuro-oncology operations were performed between 2012 and 2022, with 3911 elective and 177-day case procedures. The mean patient age was 53 (±15.63), with a median of 55 (42–65) and a range of 18–89 years. Of the 19 distinct neuro-oncology operations, only the three most common umbrella neuro-oncology operations underwent further subgroup analysis: “Excision of lesion of tissue of brain,” “excision of lesion of meninges of brain,” and “biopsy of lesion of nervous system.”
Frequency analysis
The most frequent operation type undertaken was “excision of lesion of tissue of brain” in 1927, followed by “excision of lesion of meninges of brain” in 464.
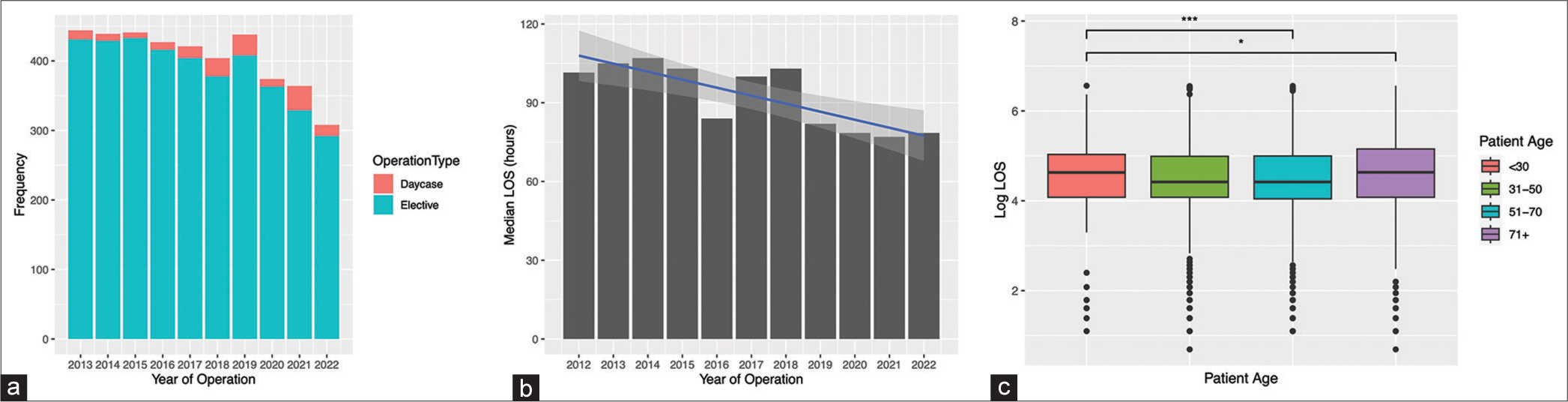
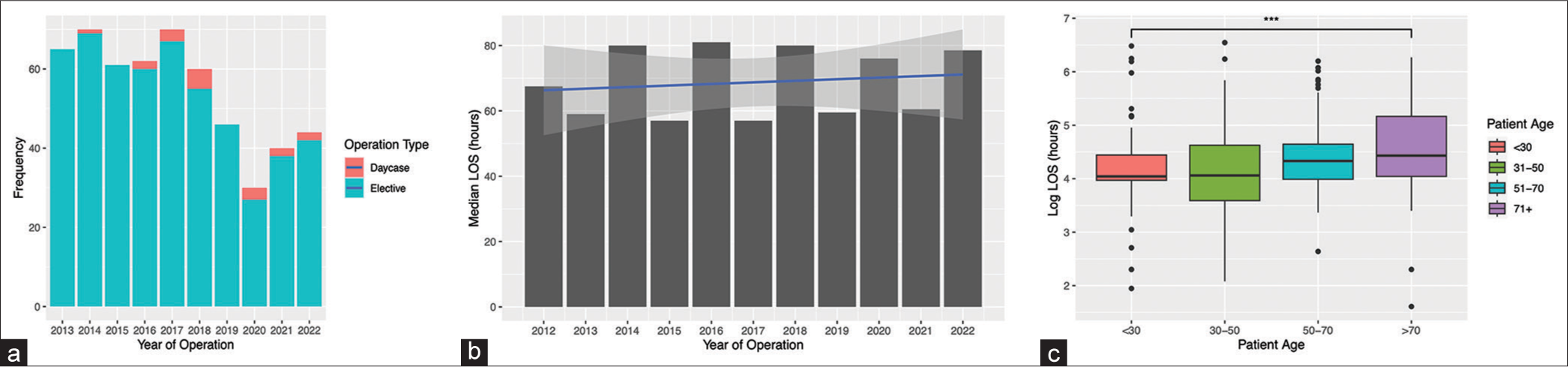
Figure 3:
Plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2012 to 2022 for all neuro-oncological (NO) operations: (a) frequency of all NO operations split by elective and day case, (b) median LOS for all NO operations, and (c) comparing LOS and age, ***P < 0.001, *P < 0.05.
LOS analysis
Overall, the analysis revealed a decrease in the median LOS over time between 2012 and 2022 (MK: tau = −0.648, P = 0.0077), as shown in
Analysis of the most common umbrella operation types revealed that there was a decreasing yet non-significant trend in operative frequency across the study period for all three classifications. In terms of the effect of the pandemic, the analysis revealed no reliable change in frequency in “biopsy of lesion of nervous system” or “excision of lesion of meninges of brain” due to high year-to-year variation in the years prior. “Excision of lesion of tissue of brain” operations, however, demonstrated an increasing trend up until the 2020 COVID-19 pandemic, where the frequency decreased and has remained lower than the pre-pandemic 2019 levels. Similar to operative frequency, “excision of lesion of meninges of brain” and “excision of lesion of tissue of brain” demonstrated a decreasing trend in postoperative LOS across the study period, the latter of which decreased only in the past four years. “Biopsy of lesion of nervous system” demonstrated a stable median LOS over the decade [Supplementary
Skull base (SB)
Cohort demographics
A total of 2029 SB procedures were performed between 2012 and 2022, with 1870 elective and 59-day case procedures. The mean patient age was 53 (±16.18) years, with a median of 54 (41–65) and a range of 18–92. Of the 14 distinct SB operations, only the four most common umbrella SB operations underwent further subgroup analysis: “Excision of lesion of pituitary gland,” “excision of lesion of cranial nerve,” “excision of lesion of meninges of SB,” and “microvascular decompression of cranial nerve.”
Frequency analysis
The most frequent operation type undertaken was “excision of lesion of pituitary gland” at 392, followed by “excision of lesion of cranial nerve” at 339.
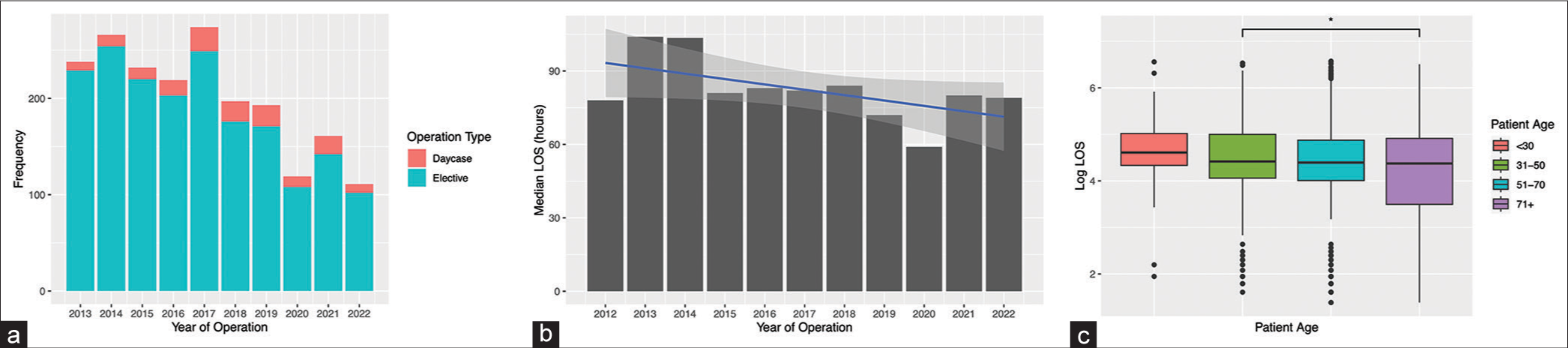
Figure 4:
Plots representing the temporal trends in operative frequency and post-operative length of stay (LOS) from 2012-2022 for all skull base (SB) operations: a) Frequency of all SB operations split by elective and day case, b) Median LOS for all SB operations, c) Comparing LOS and age, * = P <0.05.
LOS analysis
Overall, analysis showed a decrease in the median LOS between 2012 and 2022. (MK: tau = −0.382, P = 0.012), as shown in
Analysis of the most common umbrella operation types revealed that “excision of lesion of cranial nerve” and “microvascular decompression of cranial nerve” procedures demonstrated a decreasing trend in annual operative frequency, while “excision of lesion of pituitary gland” demonstrated an overall increasing trend in operative frequency. No reliable trend could be observed in the “excision of lesion of meninges of SB” group. “Excision of lesion of pituitary gland” and “microvascular decompression of cranial nerve” demonstrated a drop in procedure frequency due to COVID-19, with the former being the most pronounced. All four classifications demonstrated a trend toward decreasing LOS, with two of these being significant (P < 0.02). These were “excision of lesion of pituitary gland” and “excision of lesion of cranial nerve” [Supplementary
Functional neurosurgery
Cohort demographics
A total of 786 functional neurosurgery procedures were performed between 2012 and 2022, with 410 elective and 376 day case procedures. The mean patient age was 48.7 (±14.89) years, with a median of 50 (37–63) and a range of 18–87 years. Of the seven distinct functional operations, only the two most common umbrella classifications underwent further subgroup analysis: “Deep brain stimulation” and “vagus nerve stimulation.”
Frequency analysis
The most frequent operation type undertaken was “implantation/insertion of neurostimulator” at 393, followed by “maintenance of neurostimulator” at 332.
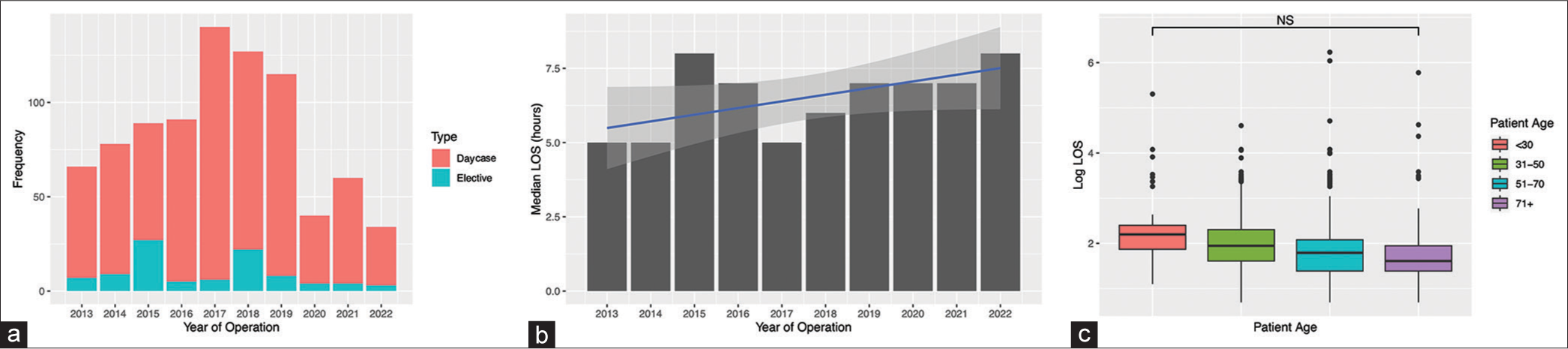
Figure 5:
Plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2012 to 2022 for all functional operations: (a) frequency of all functional operations split by elective and day case, (b) median LOS for all functional operations, and (c) comparing LOS and age, **P < 0.01, ***P < 0.001.
LOS analysis
Overall, analysis of the LOS showed a significant decreasing trend in the median LOS over the last decade (MK: tau = −0.648, P = 0.0077), as shown in
When classified by the most common procedure types, “deep brain stimulation” and “vagus nerve stimulation,” neither showed a trend toward increasing or decreasing frequency, with great intra-year variation being observed instead. “Vagus nerve stimulation” was, however, noted to have a sudden decline in frequency between the years 2015 and 2016, with a steady rise again in the years that followed. There was no observed difference in procedure frequency as a result of the pandemic. With regard to LOS, both “deep brain stimulation” and “vagus nerve stimulation” showed a decrease. “Deep brain stimulation” was observed to have a relatively stable LOS until the COVID-19 pandemic, where a rapid decline was seen, whereas “vagus nerve stimulation” had a markedly higher LOS in 2013 with the remainder of the decade maintaining a stable lower median LOS [Supplementary
Cerebrospinal fluid (CSF)
Cohort demographics
A total of 548 CSF operations were performed between 2012 and 2022, with 530 elective and 18-day case procedures. The mean patient age was 52.79 (±19.04), with a median of 53 years (36–71) and a range of 18–86 years. Of the six distinct CSF operations, only the most common umbrella CSF operation, “creation of shunt,” underwent further subgroup analysis.
Frequency analysis
The most frequent operation type undertaken was “creation of shunt” at 185, followed by “monitoring of tissue pressure in the brain” at 112.
Figure 6:
Plots representing the temporal trends in operative frequency and post-operative length of stay (LOS) from 2012-2022 for all cerebrospinal fluid (CSF) operations: a) Frequency of all CSF operations split by elective and day case, b) Median LOS for all CSF operations, c) Comparing LOS and age, *** = P <0.001.
LOS analysis
Overall, the analysis showed a fairly constant LOS over time, with no significant change in the median LOS over the period of 10 years (MK: tau = 0.147, P = 0.59), as shown in
Analysis of the most common operation type, “creation of shunt,” showed no clear trends in frequency, though it was noted that the frequency in the COVID-19 years 2020 and 2021 was significantly lower than observed previously, with an unprecedented rapid decline between 2019 and 2020. The median LOS in this procedure group also remained stable, though there was a minor increasing trend. This was largely a result of the year 2021, and as there was such a relatively small sample size in the pandemic years, it is hard to comment on the effect of COVID-19 on LOS for the “creation of shunts” [Supplementary
Peripheral nerve (PN)
Cohort demographics
A total of 840 PN operations were performed between 2012 and 2022, with 95 elective and 745-day case procedures. The mean patient age was 53 (±16.00) years, with a median of 54 (42–64) and a range of 18–91. Of the seven distinct PN operations, only the most common umbrella PN operation, “carpal tunnel release,” underwent further subgroup analysis.
Frequency analysis
The most frequent operation type undertaken was “carpal tunnel release” at 307, followed by “maintenance of neurostimulator in PN” at 144.
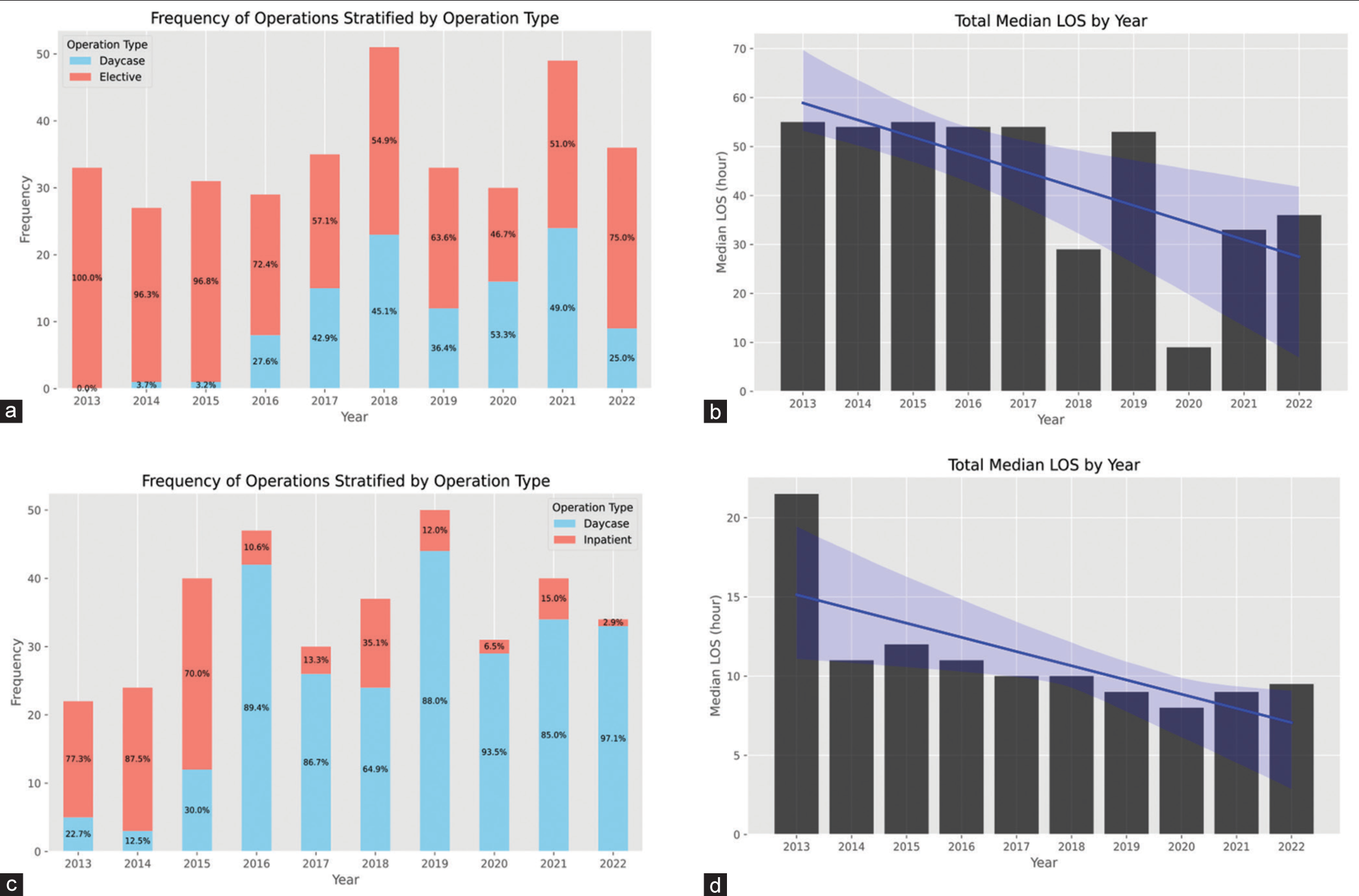
Figure 7:
Plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022 for all peripheral nerve (PN) operations: (a) frequency of all PN operations split by elective and day case, (b) median LOS for all PN operations, and (c) comparing LOS and age, NS: Not significant.
LOS analysis
Overall, the analysis showed a fairly constant LOS over time between 2013 and 2022, with no significant change in the median LOS (MK: tau = 0.479, P = 0.089), as shown in
Analysis of the most common procedure type, “carpal tunnel release,” revealed a slight trend toward decreasing frequency, though this was not significant. The frequency was at its lowest during the initial wave of the pandemic in 2020, with a slow increase observed in the years that followed. Similarly, there was a non-significant trend toward decreasing seen in the median LOS. For this procedure group, no effect on LOS as a result of COVID-19 was observed [Supplementary
DISCUSSION
Over the course of the last decade, the field of neurosurgery has undergone substantial evolution due to a culmination of factors that can have multi-faceted influences on the specialty. Positive intraoperative factors have included the acquisition of new surgical methods and the refinement of previous surgical techniques, with some subspecialties, such as spine and functional, exhibiting greater leaps in interventional improvement.[
Our results show that, overall, the majority of subspecialties had a decrease in the frequency of procedures over the 10-year period, with a sudden decline during COVID-19 and a slow recovery since. The subspecialties “Spinal,” “Neuro-oncology,” “CSF,” and “Skull-base” all had a significant decrease in the frequency of procedures over time. The “Peripheral nerve” subspecialty had a significant overall increase during this 10-year period, though a decrease was noted between 2018 and 2020. Our frequency analysis on spinal surgery demonstrated a reduction in procedures leading up to COVID-19, particularly in lumbar discectomies, contrasting with earlier findings that showed an increase between 2001 and 2011, attributed to an increased incidence of spine degeneration within an elderly population.[
Notably, “Functional,” “Neuro-oncology,” and “Skull base” subspecialties all had a rise in the frequency of day case procedures, with the “Spinal” subspecialty having a significant rise after 2015. This rise across these subspecialties is perhaps not unsurprising when considering how advancements have been made with regard to the use of more minimally invasive surgeries with improved anesthetic techniques, such as awake spinal surgery and a heavier focus on minimizing total time to recovery postoperatively. In our center, we have observed the appearance of dedicated day case theaters and staffing teams over the study period, correlating with the increased incidence demonstrated by our results. This, alongside fewer complications and an associated reduction in postoperative pain, inherently lends itself to a proportional increase in day-case procedures.[
The effect of increasing day case procedures has understandably had a large effect on postoperative LOS. Overall, “Neuro-oncology,” “CSF,” and “Functional” subspecialties had a statistically significant decrease in the median LOS over time, with “Skull Base” showing a trend toward decreasing though insignificant. No notable changes were noted in the “Spinal” subspecialty, while “Peripheral nerve” did show a trend toward an increasing LOS, though once again, this was not significant. The trends observed toward reducing LOS across most subspecialties could be attributed to a variety of factors outside the shift from elective to day cases. The understanding of how reducing inpatient stay enhances patient recovery has led to many campaigns to encourage faster discharges either at home or to alternate care facilities, with many studies attributing extended LOS to higher mortality rates.[
With regard to trends between LOS and differing age groups, “Spinal,” “Functional,” “CSF,” and “Neuro-oncology” subspecialties had a statistically significant increase in median LOS with age, while “Skull base” showed the opposite trend. Our results for “Neuro-oncology” contradict an earlier study showing a negative correlation between the age of patients presenting with a tumor and the hospital LOS.[
With respect to the impact of the pandemic on LOS, we reported a statistically significant reduction in median LOS within the subspecialties of “Neuro-oncology” and “Skull base.” This is not unexpected, as reducing hospital LOS was a strategy adopted in clinical practice in an attempt to deal with the increased pressures seen during the pandemic.[
Overall, when comparing the impact of the pandemic on the frequency of procedures, with the exception of “Skull base” and “Peripheral nerve” subspecialties, our results showed that COVID-19 led to a statistically significant decline in operation frequency above the normal trend in years prior. In the past three years, this impact has been the equivalent of not having done any surgery for more than a whole year. However, the impact of the pandemic in a private healthcare system such as the USA showed opposing results, whereby no significant change in procedure frequency was reported due to COVID-19.[
The consequence of numerous neurosurgical cancellations seen in the face of the pandemic is an expected rise in the number of referrals and an augmented post-pandemic waiting list.[
Interestingly, across many subspecialties, our post-pandemic findings from 2021 and 2022 generally do not reflect a substantial rise in the frequency of procedures as would be predicted, with no change or a decrease from pandemic levels being the predominant trend. Only the subspecialties of “Neuro-oncology” and “CSF” depicted a postpandemic rise. The hypothesized rise following the pandemic may have been hindered by a multitude of factors, including a shortage of hospital beds, stricter theater regulations, and self-isolation due to invalid swab results and COVID-related staff illness.[
At present, we do not know whether the reported trends seen at our tertiary center accurately depict trends that would be seen across other UK tertiary centers. This is especially pertinent when considering socioeconomic and ethnic differences that differ between tertiary centers serving different regions, which is in part demonstrated by our results correlating increased age with prolonged LOS. Thus, our data serve to provide a “glimpse” into neurosurgical trends within the UK that may be extrapolatable within other cohorts. Nevertheless, these results are unlikely to generalize to other private or hybrid healthcare systems due to different treatment incentives, both economic and operational, reduced financial constraints, and greater access to state-of-the-art novel technologies. Moreover, an element of uncertainty remains regarding future trends as it is difficult to pre-empt how advancing technologies, including radiomics and artificial intelligence, will alter the field of neurosurgery.[
Limitations
Despite these results, there are a few limitations in this study. First, the sample size varied throughout the course of the ten years, resulting in an imbalance dataset with some procedures having a markedly lower number of patients in some years than others. Despite our exclusion criteria largely mitigating the effects of this, it is still likely that these variations have somewhat skewed our results. Second, we were unable to determine the number of comorbidities for each individual patient, as this may have influenced LOS trends seen in this study. In addition, the impact of intraoperative and immediate postoperative complications on the LOS for patients after surgery was not explored, and the temporal trends in these factors can further elucidate/explain the changes observed. Finally, this being a single-center retrospective analysis poses questions of the generalizability and extrapolation of these results in geographically and financially distinct healthcare systems with clinically and demographically different patient populations and surgical preferences.
CONCLUSION
This study details the temporal trends observed in operative neurosurgery over a decade in a high-volume tertiary center in a public healthcare system. We observed a significant decline in postoperative LOS across most neurosurgical subspecialties, coupled with a shift toward day-case surgeries. These changes may be attributed to improved neurosurgical techniques, the pressure on inpatient beds, and perhaps the desire of patients to avoid staying in hospitals. However, the decline in overall surgical volume across subspecialties indicates the growing role of non-surgical treatments, evolving more complex (and hence longer) surgical practices, and stringent patient selection criteria. In addition, it highlights the challenges, both logistical and financial, that the NHS faces – challenges further exacerbated by the COVID-19 pandemic. COVID-19 has had a significant impact on the volume of neurosurgical procedures, and the volumes continue to be less than the pre-COVID era. Utilizing the shift away from elective and setting up extra dedicated day case neurosurgery theaters would be a practical way of dealing with the backlog of procedures.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB, Reference number: 22HIP32.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
SUPPLEMENTARY FIGURES
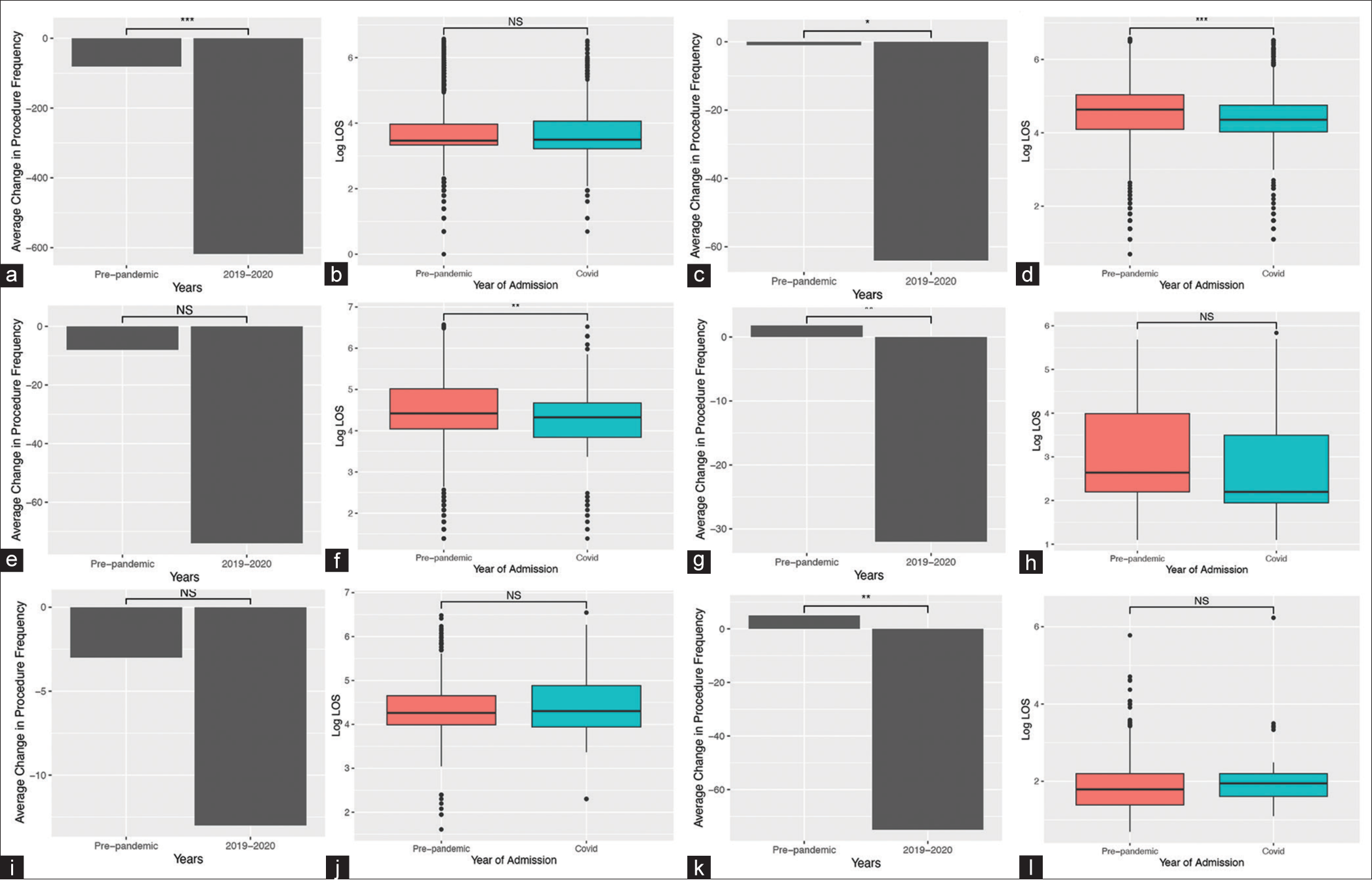
Supplementary Figure 1:
Plots representing the change observed in Frequency and post-operative length of stay (LOS) due to the COVID-19 pandemic in 6 neurosurgical subspecialties, (a) Average change in frequency of spinal procedures, *** = P < 0.001. (b) Box plot of the log LOS for spinal surgery pre-pandemic compared to the years most affected by COVID-19 (2020 and 2021), NS = not significant. (c) Average change in frequency of neuro-oncological procedures, * = P < 0.05. (d) Box plot of the log LOS for neuro-oncological surgery pre-pandemic compared to the years most affected by COVID-19, *** = P < 0.001. (e) Average change in frequency of skull base procedures, NS = not significant. (f) Box plot of the log LOS for skull base surgery pre-pandemic compared to the years most affected by COVID-19, ** = P < 0.005. (g) Average change in frequency of functional procedures, ** = P < 0.005. (h) Box plot of the log LOS for functional neurosurgery pre-pandemic compared to the years most affected by COVID-19, NS = not significant. (i) Average change in frequency of CSF procedures, NS = not significant. (j) Box plot of the log LOS for CSF surgery pre-pandemic compared to the years most affected by COVID-19, NS = not significant. (k) Average change in frequency of peripheral nerve procedures, ** = P < 0.005. (l) Box plot of the log LOS for peripheral nerve surgery pre-pandemic compared to the years most affected by COVID-19, NS = not significant.
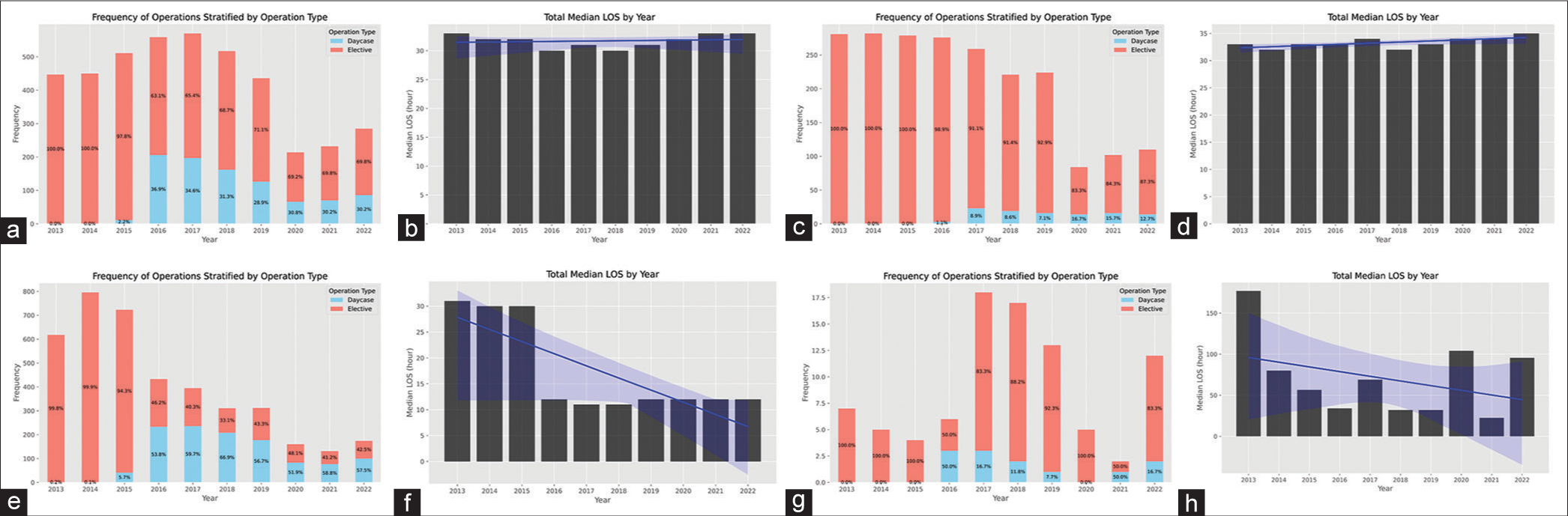
Supplementary Figure 2:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022: (a) frequency of all “decompression of lumbar spine” operations, (b) median LOS for all “decompression of lumbar spine” operations, (c) frequency of all “anterior cervical discectomy and fusion” operations, (d) median LOS for all “anterior cervical discectomy and fusion” operations, (e) frequency of all “excision of lumbar intervertebral disc” operations, (f) median LOS for all “excision of lumbar intervertebral disc” operations, (g) frequency of all “lumbar fusion” operations, and (h) median LOS for all “lumbar fusion” operations.
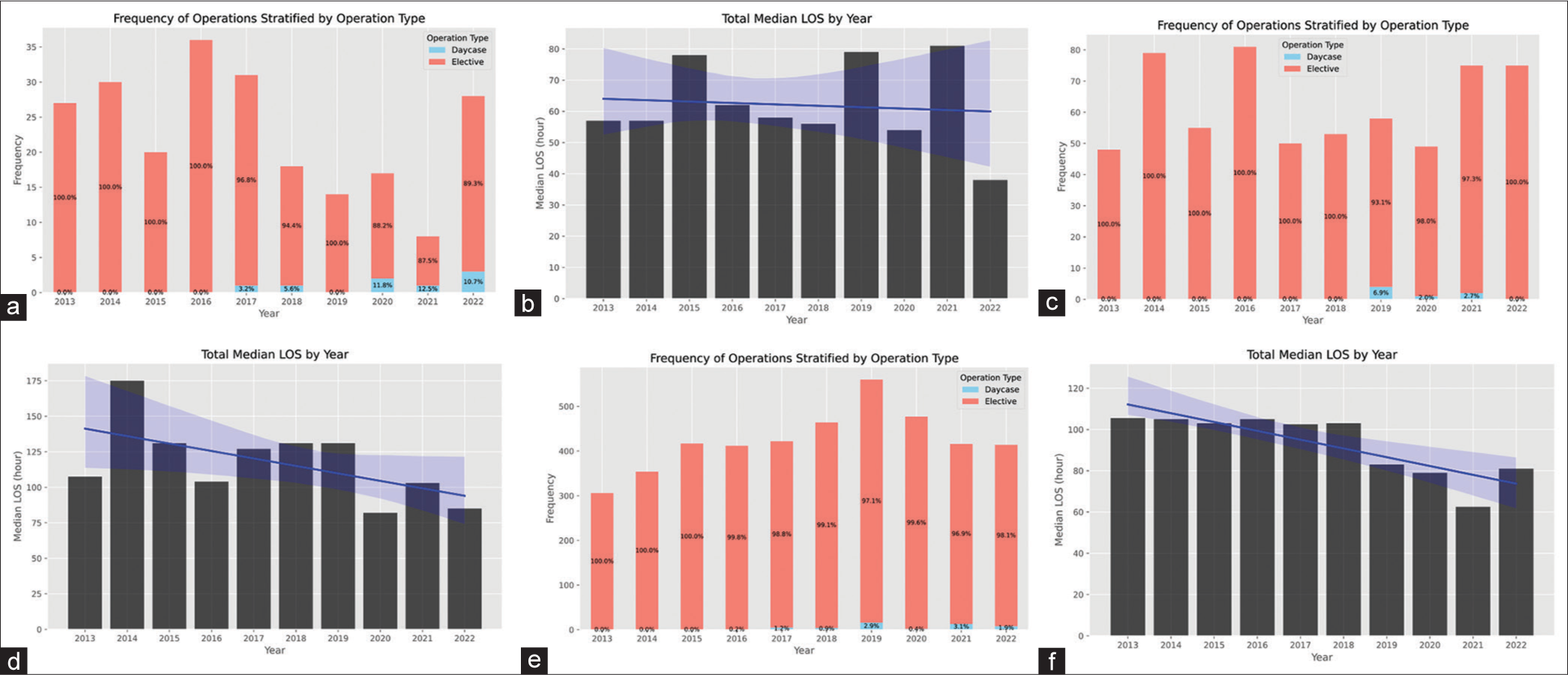
Supplementary Figure 3:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022: (a) frequency of all “biopsy of lesion of nervous system” operations, (b) median LOS for all “biopsy of lesion of nervous system” operations, (c) frequency of all “excision of lesion of meninges of brain” operations, (d) median LOS for all “excision of lesion of meninges of brain” operations, (e) frequency of all “excision of lesion of tissue of brain” operations, and (f) median LOS for all “excision of lesion of tissue of brain” operations.
Supplementary Figure 4:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022: (a) frequency of all “excision of lesion of meninges of skull base” operations, (b) median LOS for all “excision of lesion of meninges of skull base” operations, (c) frequency of all “microvascular decompression of cranial nerve” operations, (d) median LOS for all “microvascular decompression of cranial nerve” operations, (e) frequency of all “excision of lesion of pituitary gland” operations, (f) median LOS for all “excision of lesion of pituitary gland” operations, (g) frequency of all “excision of lesion of cranial nerve” operations, and (h) median LOS for all “excision of lesion of cranial nerve” operations.
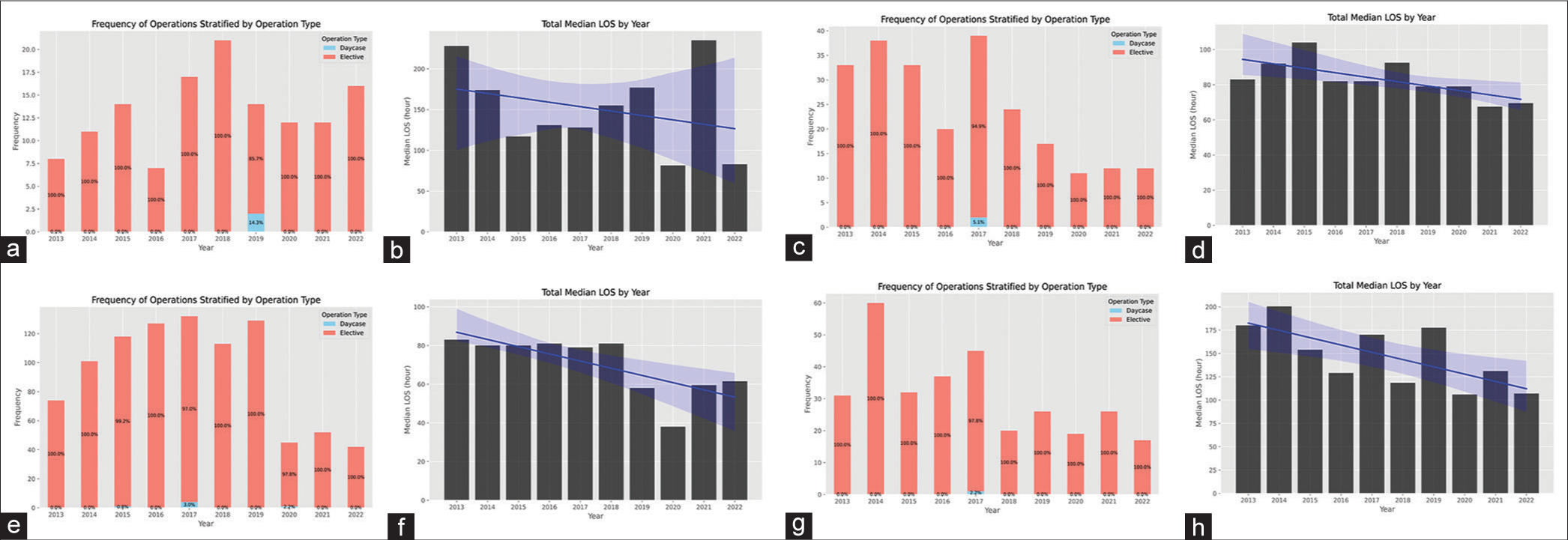
Supplementary Figure 5:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022: (a) frequency of all “deep brain stimulation” operations, (b) median LOS for all “deep brain stimulation” operations, (c) frequency of all “vagus nerve stimulation” operations, and (d) median LOS for all “vagus nerve stimulation” operations.
Supplementary Figure 6:
Bar plots representing the temporal trends in operative frequency and postoperative length of stay (LOS) from 2013 to 2022 for CSF and peripheral subspecialties: (a) frequency of all “creation of shunt” operations, (b) median LOS for all “creation of shunt” operations, (c) frequency of all “carpal tunnel release” operations, and (d) median LOS for all “carpal tunnel release” operations.
References
1. Aljoghaiman M, Martyniuk A, Farrokhyar F, Cenic A, Kachur E. Survey of lumbar discectomy practices: 10 years in the making. J Spine Surg. 2020. 6: 572-80
2. Ansari SF, Yan H, Zou J, Worth RM, Barbaro NM. Hospital length of stay and re-admission rate for neurosurgical patients. Neurosurgery. 2018. 82: 173-81
3. Arora A, Demb J, Cummins DD, Callahan M, Clark AJ, Theologis AA. Predictive models to assess risk of extended length of stay in adults with spinal deformity and lumbar degenerative pathology: Development and internal validation. Spine J. 2023. 23: 457-66
4. Ashkan K, Jung J, Velicu AM, Raslan A, Faruque M, Kulkarni P. Neurosurgery and Coronavirus: Impact and challenges-lessons learnt from the first wave of a global pandemic. Acta Neurochir (Wien). 2021. 163: 317-29
5. Batchelor TJ. Enhanced recovery after surgery and chest tube management. J Thorac Dis. 2023. 15: 901-8
6. Chrusciel J, Girardon F, Roquette L, Laplanche D, Duclos A, Sanchez S. The prediction of hospital length of stay using unstructured data. BMC Med Inform Decis Mak. 2021. 21: 351
7. Dodo Y, Okano I, Kelly NA, Sanchez LA, Haffer H, Muellner M. Risk factors for ambulatory surgery conversion to extended stay among patients undergoing one-level or two-level posterior lumbar decompression. Spine (Phila Pa 1976). 2023. 48: 748-57
8. ElGhamry AN, Jayakumar N, Youssef M, Shumon S, Mitchell P. COVID-19 and changes in neurosurgical workload in the United Kingdom. World Neurosurg. 2021. 148: e689-94
9. Hasan M, Diep D, Manoranjan B, Maharaj A, Chaudhry S, Shaheen S. Analysis of factors that influence neurosurgical length of hospital stay among newly diagnosed pediatric brain tumor patients. Pediatr Blood Cancer. 2020. 67: e28041
10. Kamat AS, Parker A. The evolution of neurosurgery: How has our practice changed?. Br J Neurosurg. 2013. 27: 747-51
11. Linzey JR, Foshee R, Moriguchi F, Adapa AR, Koduri S, Kahn EN. Length of stay beyond medical readiness in a neurosurgical patient population and associated healthcare costs. Neurosurgery. 2021. 88: E259-64
12. Magge RS, Barbaro M, Fine HA. Innovations in neurooncology. World Neurosurg. 2021. 151: 386-91
13. Makaryus R, Miller TE, Gan TJ. Current concepts of fluid management in enhanced recovery pathways. Br J Anaesth. 2018. 120: 376-83
14. Malek N. Deep brain stimulation in Parkinson’s disease. Neurol India. 2019. 67: 968-78
15. Mazzatenta D, Zoli M, Cavallo MA, Ferro S, Giombelli E, Pavesi G. Remodulation of neurosurgical activities in an Italian region (Emilia-Romagna) under COVID-19 emergency: Maintaining the standard of care during the crisis. J Neurosurg Sci. 2022. 66: 234-9
16. Perez-Roman RJ, Govindarajan V, Levi DJ, Luther E, Levi AD. The declining incidence of cervical spine surgery in patients with rheumatoid arthritis: A single-surgeon series and literature review. J Neurosurg Spine. 2022. 37: 350-6
17. Perry R, Herbert G, Atkinson C, England C, Northstone K, Baos S. Pre-admission interventions (prehabilitation) to improve outcome after major elective surgery: A systematic review and meta-analysis. BMJ Open. 2021. 11: e050806
18. Petr O, Grassner L, Warner FM, Dedeciusová M, Voldřich R, Geiger P. Current trends and outcomes of non-elective neurosurgical care in Central Europe during the second year of the COVID-19 pandemic. Sci Rep. 2022. 12: 14631
19. Pierce KE, Gerling MC, Bortz CA, Alas H, Brown AE, Woo D. Factors influencing length of stay following cervical spine surgery: A comparison of myelopathy and radiculopathy patients. J Clin Neurosci. 2019. 67: 109-13
20. Simon NG, Spinner RJ, Kline DG, Kliot M. Advances in the neurological and neurosurgical management of peripheral nerve trauma. J Neurol Neurosurg Psychiatry. 2016. 87: 198-208
21. Singh R, Richter KR, Pollock JR, Haglin JM, Balli N, Catapano JS. Trends in neurosurgical practice size: Increased consolidation 2014-2019. World Neurosurg. 2021. 149: e714-20
22. Stone K, Zwiggelaar R, Jones P, Mac Parthaláin N. A systematic review of the prediction of hospital length of stay: Towards a unified framework. PLOS Digit Health. 2022. 1: e0000017
23. Sun R, Sharma S, Benghiat H, Meade S, Sanghera P, Bramwell G. Reconfiguration from emergency to urgent elective neurosurgery for glioblastoma patients improves length of stay, surgical adjunct use, and extent of resective surgery. Neurooncol Pract. 2022. 9: 420-8
24. Tarnaris A, Arvin B, Ashkan K. Evolution in practice: How has British neurosurgery changed in the last 10 years?. Ann R Coll Surg Engl. 2008. 90: 508-12
25. Turel MK, Bernstein M. Outpatient neurosurgery. Expert Rev Neurother. 2016. 16: 425-36
26. UK Department of Health and Social Ca, editors. Hospital discharge and community support guidance. London: UK Department of Health and Social Care; 2022. p.
27. Vandiver MS, Vacas S. Interventions to improve perioperative neurologic outcomes. Curr Opin Anaesthesiol. 2020. 33: 661-7
28. Wahba AJ, Cromwell DA, Hutchinson PJ, Mathew RK, Phillips N. Patterns and outcomes of neurosurgery in England over a five-year period: A national retrospective cohort study. Int J Surg. 2022. 99: 106256
29. Wali AR, Ryba BE, Kang K, Santiago-Dieppa DR, Steinberg J, Diaz-Aguilar LD. Impact of COVID-19 on a neurosurgical service: Lessons from the university of California San Diego. World Neurosurg. 2021. 148: e172-81
30. Wang KY, McNeely EL, Dhanjani SA, Raad M, Puvanesarajah V, Neuman BJ. COVID-19 significantly impacted hospital length of stay and discharge patterns for adult spinal deformity patients. Spine (Phila Pa 1976). 2021. 46: 1551-6
31. Zhao EJ, Yeluru A, Manjunath L, Zhong LR, Hsu HT, Lee CK. A long wait: Barriers to discharge for long length of stay patients. Postgrad Med J. 2018. 94: 546-50