- Department of Neurology and Neurosurgery, IRCCS Galeazzi, Milan, Italy, Via Riccardo Galeazzi 4, Milan, Italy Cap 20161
Correspondence Address:
Domenico Servello
Department of Neurology and Neurosurgery, IRCCS Galeazzi, Milan, Italy, Via Riccardo Galeazzi 4, Milan, Italy Cap 20161
DOI:10.4103/2152-7806.161242
Copyright: © 2015 Zekaj E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Zekaj E, Saleh C, Porta M, Servello D. Temporary deep brain stimulation in Gilles de la Tourette syndrome: A feasible approach?. Surg Neurol Int 21-Jul-2015;6:122
How to cite this URL: Zekaj E, Saleh C, Porta M, Servello D. Temporary deep brain stimulation in Gilles de la Tourette syndrome: A feasible approach?. Surg Neurol Int 21-Jul-2015;6:122. Available from: http://surgicalneurologyint.com/surgicalint_articles/temporary-deep-brain-stimulation-in-gilles-de-la-tourette-syndrome-a-feasible-approach/
Abstract
Background:Gilles de la Tourette Syndrome (GTS) is a complex neuropsychiatric disorder, characterized by chronic motor and vocal tics, associated in 50-90% of cases with psychiatric comorbidities. Patients with moderate and severe clinical picture are treated with psychotherapy and pharmacological therapy. Deep brain stimulation (DBS) is reserved for pharmacological refractory GTS patients. As GTS tends to improve with time and potentially resolves in the second decade of life, the major concern of DBS in GTS is the age at which the patient undergoes surgical procedure. Some authors suggest performing DBS after 18 years, others after 25 years of age.
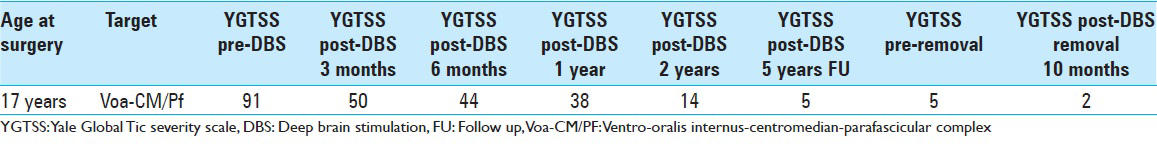
Case Description:We present a 25-year-old patient with GTS, who was aged 17 years and was treated with thalamic DBS. DBS resulted in progressive and sustained improvement of tics and co-morbidities. After 6 years of DBS treatment, it was noted that the clinical improvement was maintained also in OFF stimulation setting, so it was decided to keep it off. After 2 years in off-setting and stable clinical picture the entire DBS device was removed. Six months after DBS device removal the patient remained symptom-free.
Conclusions:DBS is a therapeutic option reserved for severe and refractory GTS cases. In our opinion DBS might be considered as a temporary application in GTS.
Keywords: Deep brain stimulation, Gilles de la Tourette syndrome, management, timing
INTRODUCTION
Gilles de la Tourette syndrome (GTS) is a chronic neuropsychiatric disorder, characterized by multiple vocal and motor tics.[
CASE REPORT
We present a patient with GTS,[
DISCUSSION
In the late 1990s, Vandewalle et al. applied the first stereotactic bilateral DBS for refractory GTS targeting the Vo-Cm/Pf complex.[
CONCLUSION
DBS is experimental in GTS and unfortunately large clinical trials remain rare in DBS, whatever its indication. This has several reasons, as the important financial aspects of a complex surgical intervention, the difficulties to standardize the procedure and the strict eligibility criteria for DBS, foremost for subjects per definition refractory to conventional treatment. The publication of every case, favorable and unfavorable outcomes,[
DBS application needs to be weighted against the severity of the disease and its co-morbidies, for which no other therapeutic means are available.
SUPPLEMENTAL VIDEO INFORMATION
Pre-DBS, at 9 months post-DBS, 1 year DBS off
Pertinent translations:
9 months post-DBS:
MP (Mauro Porta): How are you Simone?
Patient: I feel much better now.
MP: When did you have the implantation of the pacemaker?
Patient: Last year in April.
MP: And now you do not have any more tics?
Patient: No, not now anymore.
MP: Also no vocal tics?
Patient: No, no.
MP: So, you feel fine.
Patient: Yes.
At one year DBS off the patient is saying that he benefited much from DBS and that he could also take the driving license, thanks to it. He works now as an electrician.
Video Available at: www.surgicalneurologyinternational.com/video/GTS_DBS.wmv
References
1. Ackermans L, Neuner I, Temel Y, Duits A, Kuhn J, Visser-Vandewalle V. Thalamic deep brain stimulation for tourette syndrome. Behav Neurol. 2013. 27: 133-8
2. .editors. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: 2000. p.
3. Dueck A, Wolters A, Wunsch K, Bohne-Suraj S, Mueller JU, Haessler F. Deep brain stimulation of globus pallidus internus in a 16-year-old boy with severe tourette syndrome and mental retardation. Neuropediatrics. 2009. 40: 239-42
4. Hassler R, Dieckmann G. Stereotaxic treatment of tics and inarticulate cries or coprolalia considered as motor obsessional phenomena in gilles de la tourette's disease. Rev Neurol. 1970. 123: 89-100
5. Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C. Course of tic severity in tourette syndrome: The first two decades. Pediatrics. 1998. 102: 14-9
6. Mink JW, Walkup J, Frey KA, Como P, Cath D, Delong MR. Patient selection and assessment recommendations for deep brain stimulation in tourette syndrome. Mov Disord. 2006. 21: 1831-8
7. Muller-Vahl KR, Cath DC, Cavanna AE, Dehning S, Porta M, Robertson MM. European clinical guidelines for tourette syndrome and other tic disorders.Part IV: Deep brain stimulation. Eur Child Adolesc Psychiatry. 2011. 20: 209-17
8. Robertson MM. Gilles de la tourette syndrome: The complexities of phenotype and treatment. Br J Hosp Med. 2011. 72: 100-7
9. Saleh C, Gonzalez V, Cif L, Coubes P. Deep brain stimulation of the globus pallidus internus and gilles de la tourette syndrome: Toward multiple networks modulation. Surg Neurol Int. 2012. 3: S127-42
10. Servello D, Sassi M, Brambilla A, Defendi S, Porta M. Long-term, post-deep brain stimulation management of a series of 36 patients affected with refractory gilles de la tourette syndrome. Neuromodulation. 2010. 13: 187-94
11. Vandewalle V, van der Linden C, Groenewegen HJ, Caemaert J. Stereotactic treatment of gilles de la tourette syndrome by high frequency stimulation of thalamus. Lancet. 1999. 353: 724-






enrico de divitiis
Posted September 2, 2015, 12:17 pm
A reference related this field: de Divitiis E, D’Errico A, Cerillo A: Stereotactic surgery in Gilles de la Tourette syndrome. Acta Neurochir (Wien). 1977;(Suppl 24):73.
If interested Video of pre/post operative condition of patient is available.