- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, United States.
Correspondence Address:
Mokshal H. Porwal, Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, United States.
DOI:10.25259/SNI_457_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mokshal H. Porwal, Danyon J. Anderson, Omar Hussain, Brandon Robert Winston Laing, Hesham Soliman. Temporary standalone percutaneous fixation with pedicle screws for the treatment of subacute tuberculous osteomyelitis with kyphotic deformity in the lumbar spine. 17-Jun-2022;13:256
How to cite this URL: Mokshal H. Porwal, Danyon J. Anderson, Omar Hussain, Brandon Robert Winston Laing, Hesham Soliman. Temporary standalone percutaneous fixation with pedicle screws for the treatment of subacute tuberculous osteomyelitis with kyphotic deformity in the lumbar spine. 17-Jun-2022;13:256. Available from: https://surgicalneurologyint.com/surgicalint-articles/11657/
Abstract
Background: Tuberculous (TB) osteomyelitis is a rare, but challenging infection, that mandates antituberculosis antibiotics, and potentially surgical intervention. Per the Gulhane Askeri Tip Akademisi (GATA) classification system, corrective reconstruction is indicated in severe cases, where the kyphotic deformity is >20° (GATA Class III). Here, we describe a case of BCG vaccine-induced lumbar TB osteomyelitis at the L1-2 level in a patient presenting with mechanical pain and a focal, nonfixed kyphotic deformity of 36.1°. Surgery consisted of percutaneous fixation with pedicle screws without debridement, fusion arthrodesis, or anterior reconstruction.
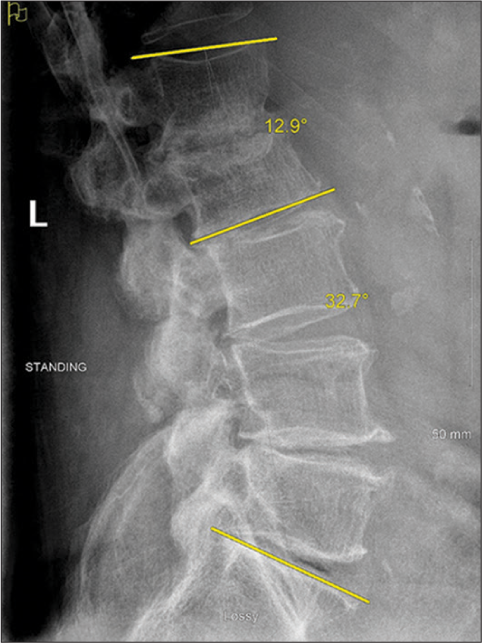
Case Description: A 77-year-old male presented with L1-2 TB osteomyelitis secondary to intravesical BCG application. A 36.1° focal nonfixed kyphotic deformity was evident on standing X-rays that reduced in the supine position. He underwent posterior percutaneous screw fixation with rods extending from the T12 to L3 levels, with resolution of his mechanical pain. Nine months later, the CT demonstrated reconstitution of the vertebral bodies (i.e., volume increase of 6.99 cm3 (21%) and 7.49 cm3 (27%) at L1 and L2, respectively). Standing X-rays after hardware removal demonstrated 32.7° of lumbar lordosis and a reduction of focal kyphosis to 12.9°.
Conclusion: Here, we present an exceedingly rare case of BCG vaccine-induced L1-2 spinal tuberculosis with extensive vertebral body destruction and deformity. This was effectively treated with standalone temporary pedicle fixation instead of corpectomy and reconstruction.
Keywords: BCG vaccine, GATA classification, Percutaneous fixation, Spinal tuberculosis, Tuberculous osteomyelitis
INTRODUCTION
Mycobacterium tuberculosis and, rarely, Mycobacterium bovis are two uncommon microbes which can cause Tuberculous (TB) osteomyelitis, also referred to as Pott’s disease of the spine. For TB-related infections, the treatment typically includes long-term antibiotic therapy. External brace immobilization is also often recommended for pain control and requires close clinical and radiographic follow-up.[
Surgery
Per the Gulhane Askeri Tip Akademisi (GATA) classification system, correction of deformity, reconstruction, and decompression are indicated when overt deformities of >20°, instability, or vertebral collapse are present.[
METHODS
We present a case report and review of the literature involving 54 patients with TB who underwent standalone percutaneous instrumentation, without fusion, for TB osteomyelitis in the thoracolumbar spine.
Case presentation
A 77-year-old male with a history of bladder cancer was treated in early 2018 with intravesical injection of BCG (i.e., a stimulant for a cell-mediated immune response). A few months following his last dose, he presented with severe lower back pain and lumbar radiculopathy. A biopsy of a L1-2 vertebral lesion documented M. bovis (i.e., TB osteomyelitis). Despite anti-TB antibiotics including rifampin, isoniazid, and ethambutol, his symptoms progressed. When the MRI demonstrated progressive degenerative L1–L5 stenosis, he underwent a L1-5 laminectomy. Following this procedure, his radiculopathy and hip pain resolved [
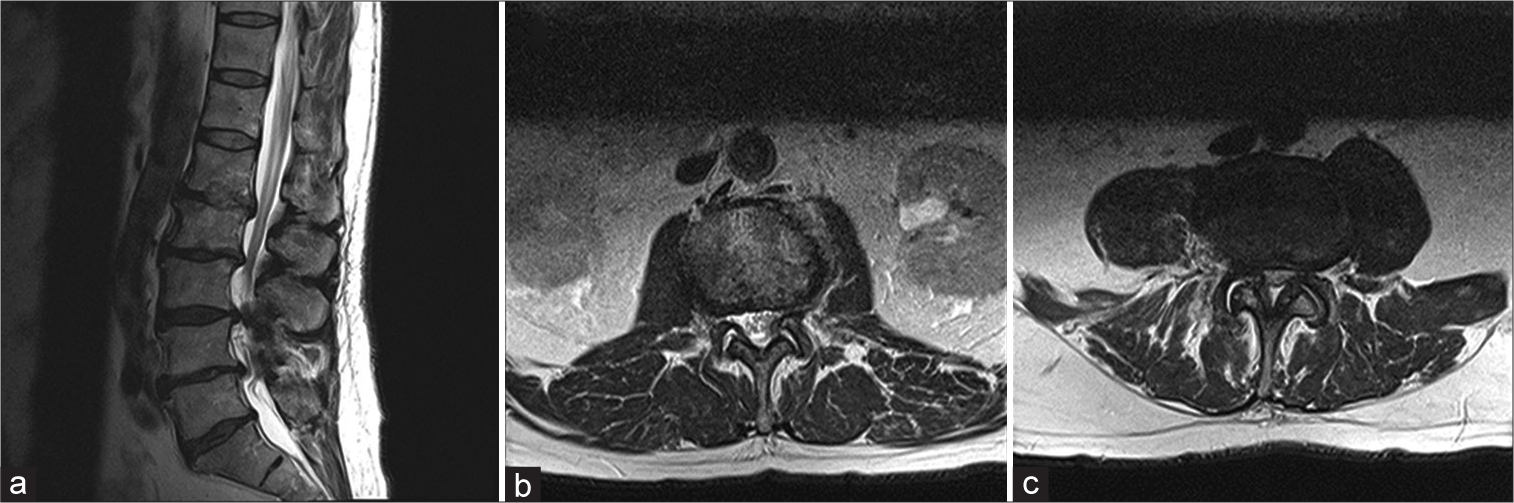
Figure 1:
Prelaminectomy T2 MRI (a) sagittal lumbar spine, (b) axial L1-2 spine, (c) axial L3-4 spine multilevel degenerative changes are noted resulting in severe canal stenosis particularly at L2–L3 and L3–L4 and slightly less pronounced canal narrowing at L4–L5 and L1–L2. Multilevel foraminal narrowing are noted from L1 to S1.
Recurrent symptoms/signs of TB L1–L2 osteomyelitis
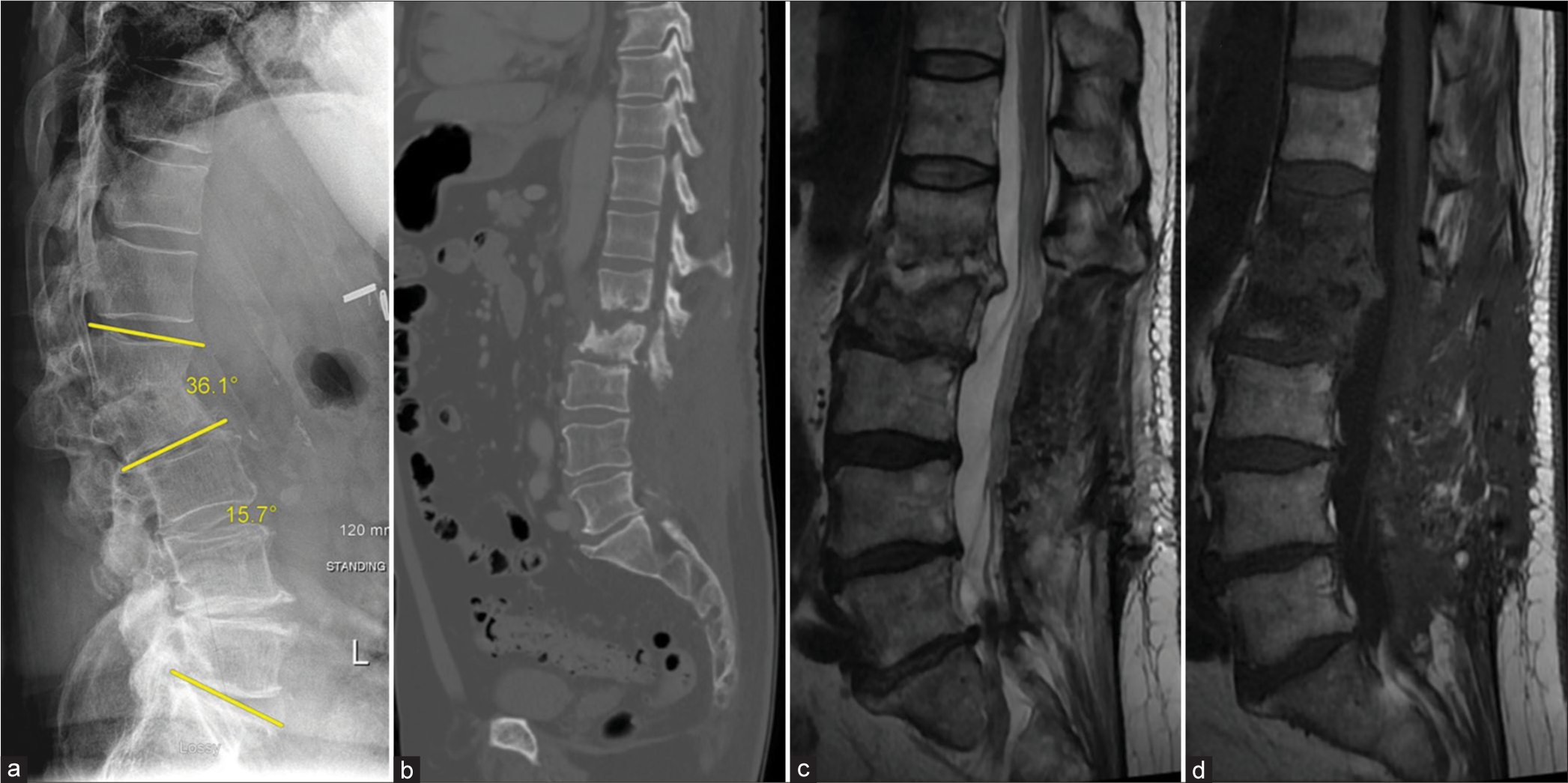
Five weeks later, he experienced progressive mechanical back pain despite bracing, night sweats, and fever. X-rays and the CT studies confirmed progressive osteomyelitic destruction of the L1–L2 vertebral bodies [
Figure 2:
Prefixation scans: (a) standing lateral X-ray: lumbar Lordosis 15.7° and L1-2 kyphosis 36.1° (as illustrated by yellow lines), (b) CT scan: L1-2 erosion, L1 vertebral volume is 33.81 cm3, and L2 volume are 27.59 cm3, (c) T2, and (d) T1 sagittal lumbar spine MRI post contrast. There is L1 and L2 edema and destruction with L1-2 disk enhancement.
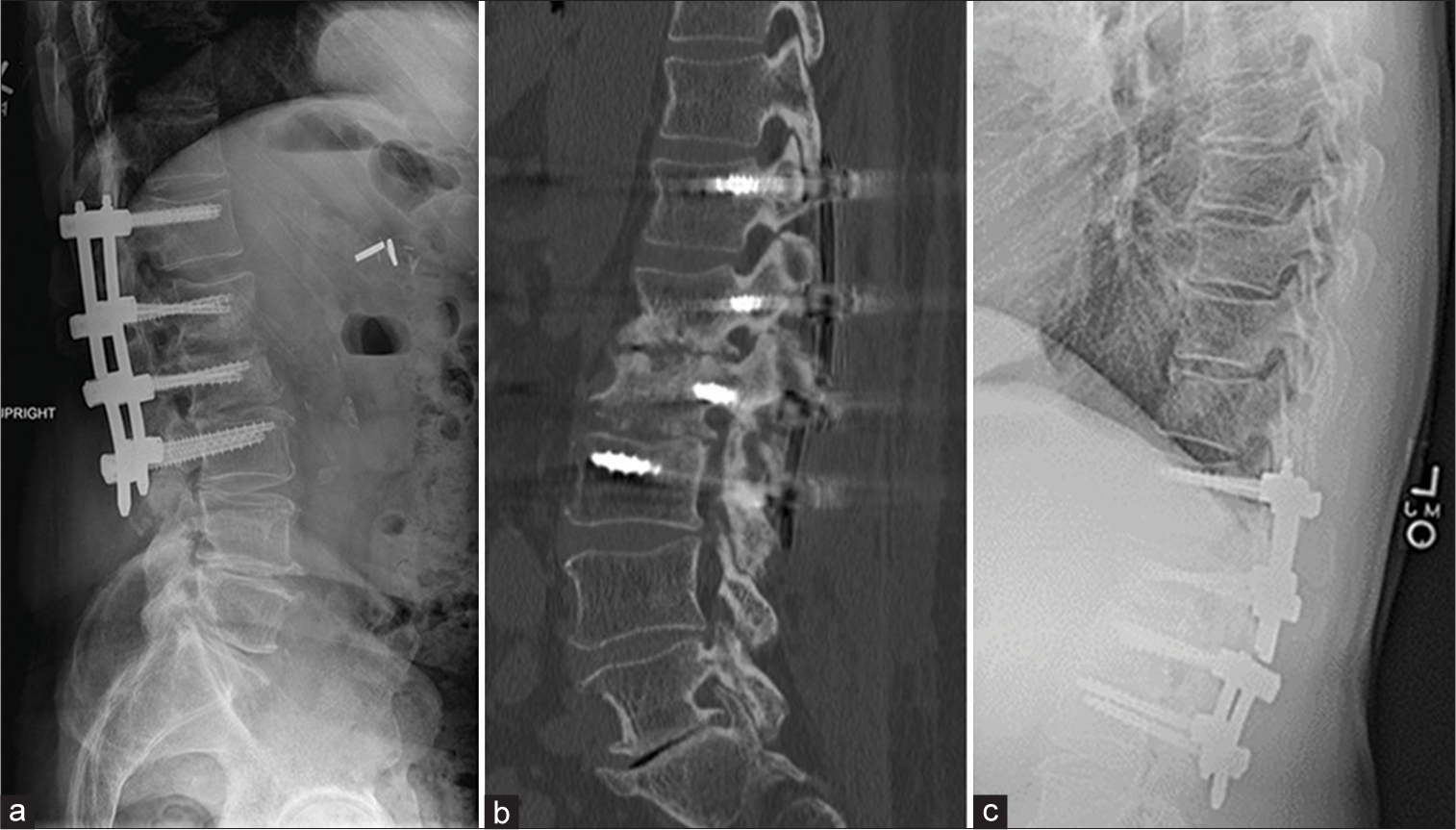
Secondary surgery
The patient underwent posterior percutaneous pedicle screw fixation with rods from T12 to L3 that successfully reduced the kyphotic deformity [
DISCUSSION
BCG treatment of bladder cancer with 5% rare complication of osteomyelitis
The BCG vaccine is a live, attenuated form of M. bovis commonly used to prevent tuberculosis infection in high-risk countries. A unique additional use of this vaccine is for intravesical injection in the treatment of bladder cancer; <5% of patients experience adverse reactions to this treatment.[
Anti-TB antibiotics are the mainstay treatment of spinal TB to treat the underlying infection.[
Literature review
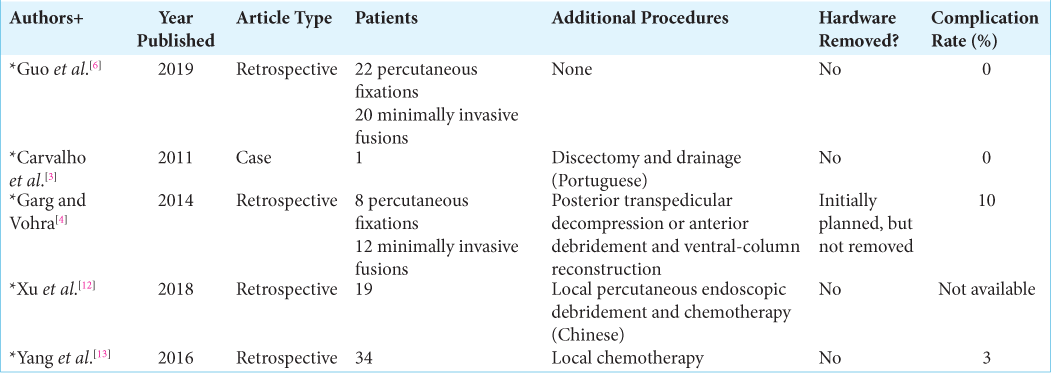
Percutaneous instrumentation/fixation, without fusion arthrodesis, with pedicle screws has been previously described in the setting of bacterial pyogenic osteomyelitis, including spinal TB [
CONCLUSION
We present a rare case of BCG vaccine-induced L1-2 TB osteomyelitis with extensive (42% at L1, 41% at L2) vertebral body destruction that was successfully treated with a stand-alone percutaneous fixation technique instead of utilizing traditional decompression and/or fusion procedures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alam S, Phan K, Karim R, Jonayed SA, Munir HK, Chakraborty S. Surgery for spinal tuberculosis: A multi-center experience of 582 case. Glob Spine J. 2016. 1: 65-71
2. Broekx S, Buelens E. Tuberculous spondylitis following intravesical bcg-instillation in the treatment of transitional cell carcinoma: Case report and systematic review. Clin Neurol Neurosurg. 2020. 194: 105944
3. Carvalho B, Pereira P, Silva PS, Silva J, Pinto M, Vazs R. Lumbar tuberculous spondylodiscitis: A minimally invasive surgical approach. Acta Reumatol Port. 2011. 36: 57-60
4. Garg N, Vohra R. Minimally invasive surgical approaches in the management of tuberculosis of the thoracic and lumbar spine. Clin Orthop Relat Res. 2014. 472: 1855-67
5. Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2011. 34: 440-54
6. Guo S, Zhu K, Zhang S, Ma B, Yang M, Yan M. Percutaneous pedicle screw fixation alone versus debridement and fusion surgery for the treatment of early spinal tuberculosis: A retrospective cohort study. Med Sci Monit. 2019. 25: 1549-57
7. Lamm DL. Efficacy and safety of bacille Calmette-Guérin immunotherapy in superficial bladder cancer. Clin Inf Dis. 2000. 31: S86-90
8. Oguz E, Sehirlioglu A, Altinmakas M, Ozturk C, Komurcu M, Solakoglu C. A new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop. 2008. 32: 127
9. Rutges JP, Kempen DH, van Dijk M, Oner FC. Outcome of conservative and surgical treatment of pyogenic spondylodiscitis: A systematic literature review. Eur Spine J. 2016. 25: 983-99
10. Schirmer P, Renault CA, Holodniy M. Is spinal tuberculosis contagious?. Int J Infect Dis. 2010. 14: e659-66
11. von Reyn CF, Vuola JM. New vaccines for the prevention of tuberculosis. Clin Infect Dis. 2002. 35: 465-74
12. Xu NJ, Chen YL, Jiang WY, Ma WH. Treatment of senile spinal tuberculosis with posterior percutaneous pedicle screw fixation combined with local percutaneous endoscopic debridement. Zhongguo Gu Shang. 2018. 31: 1005-11
13. Yang H, Song F, Zhang L, Li N, Zhang X, Wang Y. Management of spine tuberculosis with chemotherapy and percutaneous pedicle screws in adjacent vertebrae: A retrospective study of 34 cases. Spine (Phila Pa 1976). 2016. 41: E1415-20