- Department of Pediatrics, Rush University Medical Center, Chicago, Illinois, United States.
- Department of Pediatrics, Division of Neonatology, Rush University Medical Center, Chicago, Illinois, United States.
- Department of Neurological Surgery, Rush University Medical Center, Chicago, Illinois, United States.
Correspondence Address:
Genesis Talia Mancha, Department of Pediatrics, Rush University Medical Center, Chicago, Illinois, United States.
DOI:10.25259/SNI_59_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Genesis Talia Mancha1, Suhagi Kadakia2, Lorenzo Muñoz3, Laura M. Seske2. Ten-year review of neonatal neurosurgical outcomes and cost analysis. 16-Jun-2023;14:203
How to cite this URL: Genesis Talia Mancha1, Suhagi Kadakia2, Lorenzo Muñoz3, Laura M. Seske2. Ten-year review of neonatal neurosurgical outcomes and cost analysis. 16-Jun-2023;14:203. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12369
Abstract
Background: Neurosurgical interventions in neonates may contribute to increased neonatal intensive care unit (NICU) stay. The impact of neurosurgical interventions on length of stay (LOS) and cost is not well-documented in the literature. In addition to LOS, other factors may impact overall resource utilization. Our objective was to perform a cost analysis of neonates who underwent neurosurgical procedures.
Methods: A retrospective chart review was performed on NICU patients who underwent ventriculoperitoneal and/or subgaleal shunt placement between January 1, 2010, and April 30, 2021. Postoperative outcomes were analyzed, including LOS, revisions, infections, emergency department (ED) visits following discharge, and readmissions accounting for health care utilization cost.
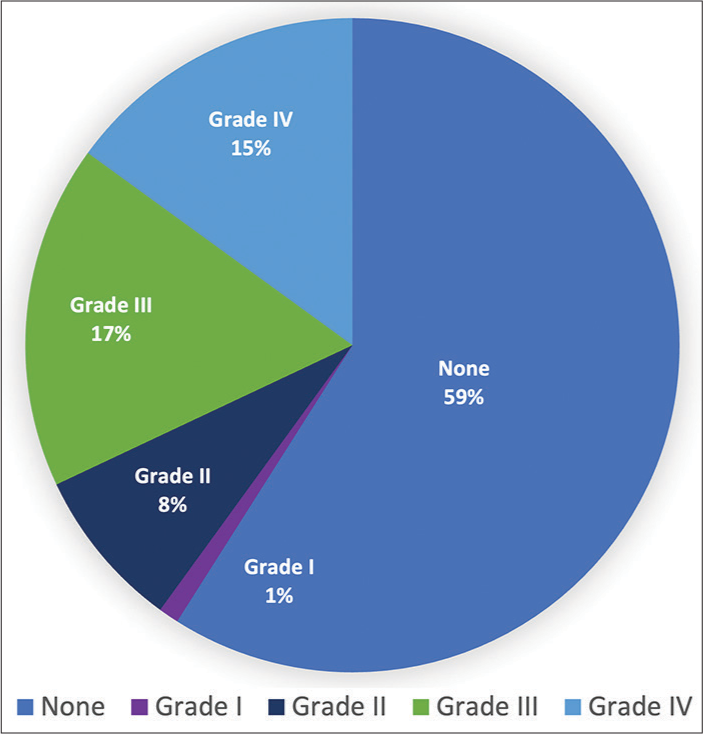
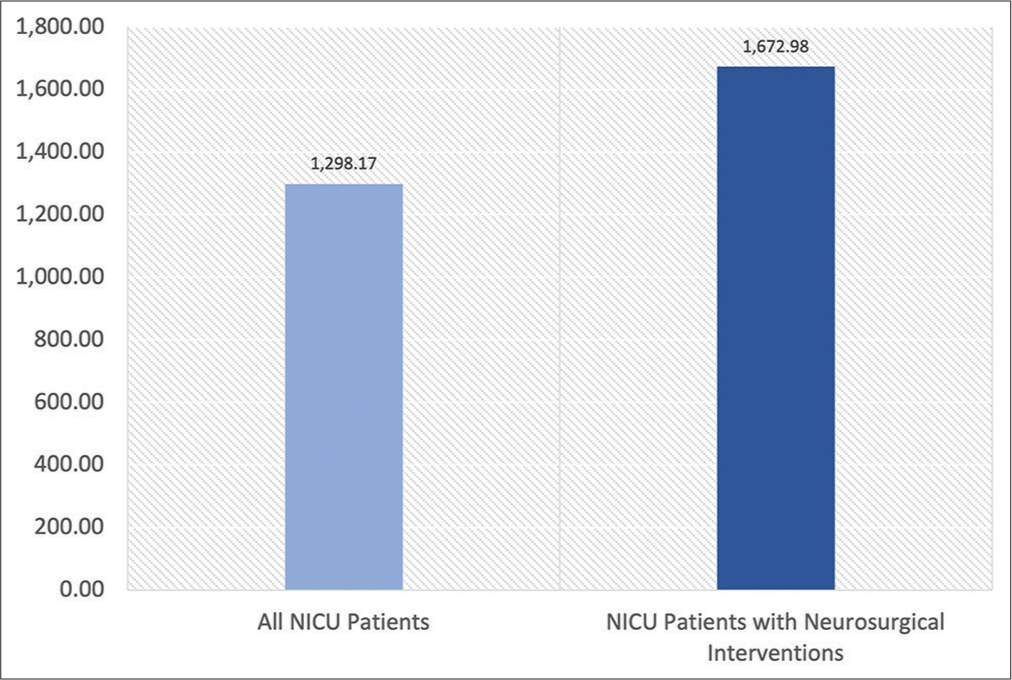
Results: Sixty-six neonates underwent shunt placement during our study period. Out of our 66 patients, 40% of infants had intraventricular hemorrhage (IVH). About 81% had hydrocephalus. Specific diagnoses for our patient population varied and included: 37.9% of patients had IVH complicated by posthemorrhagic hydrocephalus, 27.3% had Chiari II malformation, 9.1% had a cystic malformation leading to hydrocephalus, 7.5% had solely hydrocephalus or ventriculomegaly, 6.0% had myelomeningocele, 4.5% had Dandy-Walker malformation, 3.0% had aqueductal stenosis, and the remaining 4.5% had varying other pathologies. In our patient population, 11% of patients had an identified or suspected infection within 30 days after surgery. The average LOS was 59 days versus 67 days for patients with a postoperative infection. Number of patients who visited the ED within 30 days of discharge was 21%. Of these ED visits, 57% led to readmission. Complete cost analysis was available for 35 out of 66 patients. The average LOS was 63 days with average cost of admission of $209,703.43. Average cost for readmission was $25,757.02. Average daily cost for neurosurgical patients was $1,672.98 versus $1,298.17 for all NICU patients.
Conclusion: Neonates who underwent neurosurgical procedures had longer LOS as well as higher daily cost. LOS for infants with infections following procedures was increased by 10.6%. Further research is needed to optimize health-care utilization for these high-risk neonates.
Keywords: Hydrocephalus, Length of stay, Neonates, Readmissions, Ventriculoperitoneal shunt
INTRODUCTION
Hydrocephalus in children results from impaired cerebrospinal fluid (CSF) resorption or CSF obstruction. Hydrocephalus is one of the most common conditions requiring procedural intervention by pediatric neurosurgeons. Nearly 400,000 cases of pediatric hydrocephalus present each year globally, with a global prevalence of 85/100,000.[
Despite the advances in shunt technology, there are several potential complications of shunt placement surgery, including infection, migration, obstruction, mechanical failure, under-drainage, and over-drainage.[
Complications of shunt placement in neonates may lead to a prolonged length of stay (LOS) and cost of admission in the neonatal intensive care unit (NICU). These potential sequelae may also negatively impact morbidity and mortality in this high-risk population. Complications are well-documented, but there is a dearth of literature on the impact of neurosurgical interventions on the length of NICU stay and cost of admission. Importantly, cost may also be influenced by other factors independent of LOS alone.
To fill this gap, we performed a cost analysis of NICU hospitalization, 30-day readmissions, and emergency department (ED) visits for neonates who underwent VP and/or subgaleal shunt placement during the initial NICU admission. Studying and optimizing these metrics have become crucial during a pandemic.
MATERIALS AND METHODS
This study was approved by the institutional review board. We conducted a retrospective review between January 1, 2010, and April 30, 2021, at a tertiary care center in an urban hospital in the Midwest. A total of 66 patients were included in the study. Infants who underwent either a VP shunt or subgaleal shunt placement during initial hospitalization from birth in the NICU were included in the study. Patients who had shunts placed after initial discharge home from the hospital, or any infants with central nervous system (CNS) abnormalities not requiring surgical intervention were excluded from the study.
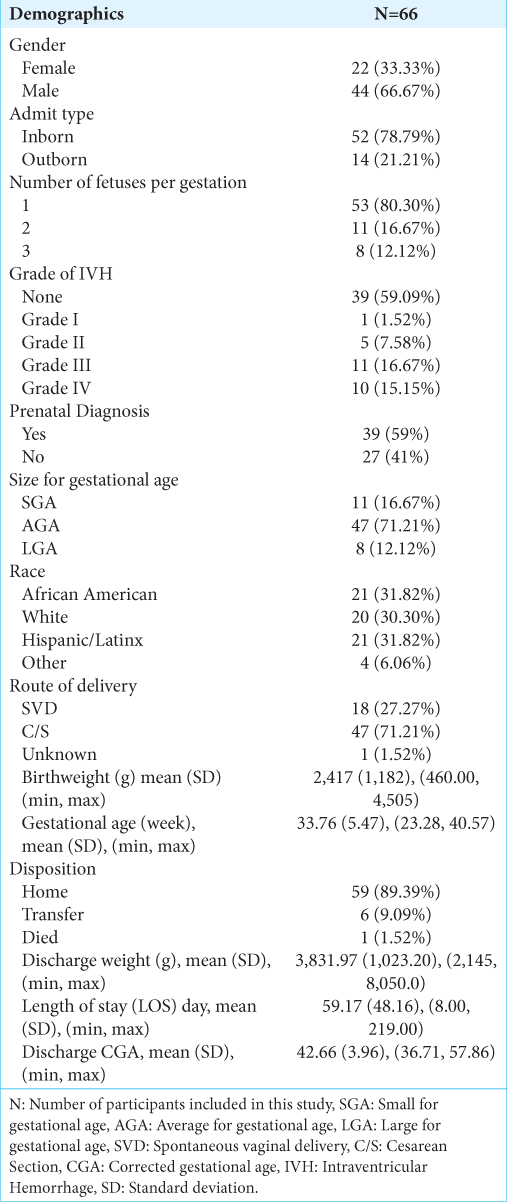
Study variables included admission type, birth weight in grams, gestational age at birth in weeks, discharge corrected gestational age (CGA), number of gestations per pregnancy, size for gestational age, sex, race, delivery type, indication for delivery, maternal risk factors, Apgar scores, LOS, disposition upon discharge, discharge weight in grams, grade of intraventricular hemorrhage (IVH), presence of hydrocephalus, requirement of VP shunt placement, subgaleal shunt placement, shunt placement and revision time, infection after shunt placement, type of infection, timing of infection, seizures pre and post shunt placement, bleed after shunt placement, requirement of gastrostomy tube placement, respiratory support at time of discharge, requirement of tracheostomy, congenital anomalies or genetic syndromes, 30 day readmission, ED visits within 30 days of discharge, and requirement of direct admission from clinic, as well as dates and CGA of all events [
Data analysis was performed through the institution’s Clinical Informatics and Biostatistics Department using descriptive statistics with R 4.1.3 software. Cost data were obtained through the institution’s financial analysis team. Consistent definitions and costing methodology available since 2015 were used to complete cost analysis for 35 out of 66 patients. These data were utilized to calculate the average daily cost of admission, ED visits, and readmissions for our patient population. In addition, cost analysis of average neonatal patients in NICU was obtained for comparison purposes during the study period.
RESULTS
Sixty-six neonates were included in our study. A total of 52 (78.8%) patients were in-born and 14 (21.2%) were transferred to our NICU from other institutions [
The average LOS was 59 days for all 66 neonates. For the seven patients who had an infection, average LOS was 67 days. For the remaining 59 patients, the average LOS was 58 days. Fifteen out of our 66 neonates who had prenatal diagnoses had a LOS of 20 days or less. Average LOS across all NICU patients in our institution from October 2018 to April 2021 was 22.73 days. Following discharge from the NICU, 21% of patients (n = 14) presented to the ED within 30 days of discharge. Of these 14 ED visits, 57% (n = 8) led to readmission. Of the total 10 readmissions, 2 (20%) were direct admissions from clinic.
The average LOS for the 35 patients for whom a complete cost analysis was completed was 63 days. Average LOS for all NICU patients from 2018 to 2021 was 22 days. The average cost of admission for the available study patients was $209,703.43 with a range of $28,515.51–$1,491,942.40. Average daily cost for our patient population was $1,672.98, whereas average daily cost for all NICU patients was $1,298.17. Five patients required readmission with an average cost of readmission $25,757.02 ranging from $1,998.71 to $56,805.36 [
DISCUSSION
To the best of our knowledge following review of available literature, this is the first study to show cost analysis in neonates with neurosurgical procedures. We examined patient outcomes for neonates having undergone neurosurgical procedures in our NICU with particular emphasis on how outcomes impact both LOS as well as resource utilization. Our patient population included a wide variety of demographics from all gestational ages. A potential confounding factor in our analysis is that prematurity alone is a risk factor for increased morbidity and mortality and therefore could increase patient LOS regardless of surgical intervention. Although there are many factors that may contribute to both metrics, these data may help elucidate whether some outcomes can be anticipated and addressed to decrease both LOS and resource utilization.
The diagnosis of ventriculomegaly can be made on screening prenatal ultrasound (US), demonstrated by atrial dilation of >10 mm.[
Prior studies have demonstrated that rates of shunt infection for patients that undergo VP shunt placement are between 10% and 14% in neonates.[
Timing of shunt placement is complex for each patient’s unique circumstance. Prior studies have shown that the relative risk for infection is higher in late shunt placement versus early shunt placement. In patients with late shunt placement, there were increased cases of CSF leakage which was thought to be due to progressive hydrocephalus leading to wound bulging and subsequent CSF leakage thus leading to higher rates of infection.[
Previous studies examining overall cost-effectiveness of different interventions for hydrocephalus demonstrated that VP shunt placement was more clinically and cost-effective when compared to endoscopic third ventriculostomy (ETV) or ETV with choroid plexus cauterization.[
Limitations
There were several potential limitations of our study. First, it was a single-center study, and analysis of readmission and ED visits was limited to review institutional EMR. The study also was not an age matched control study. Consistent definitions and costing methodology utilized have been the same since 2015 and thus adjustments for inflation were not performed. The cost of surgery is multi-factorial due to additional costs associated with each procedure (e.g., anesthesia) and the report from the financial data mart did not delineate this information, as each case had different contributing factors.
CONCLUSION
Neonates who underwent neurosurgical procedures during initial NICU hospitalization had increased LOS and health-care utilization costs compared to average neonates during the study period. Further research is needed to optimize health-care utilization for these high-risk neonates along with studying other pathologies and LOS. The importance of such efforts has only been further emphasized by the recent COVID-19 pandemic, which has brought to light the need for cost-effective care and resource optimization. Increased efforts in prenatal testing of CNS abnormalities as well as individual neurologic pathologies could also be of great advantage due to potential planning for these patients which as a result could help guide care.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
We thank Sarah Basharkhah, MS3 for her assistance with data collection and insightful contributions to literature review.
References
1. Agarwal N, Shukla RM, Agarwal D, Gupta K, Luthra R, Gupta J. Pediatric ventriculoperitoneal shunts and their complications: An analysis. J Indian Assoc Pediatr Surg. 2017. 22: 155-7
2. Bakhsh A. CSF Shunt complications in infants-an experience from Pakistan. Pediatr Neurosurg. 2011. 47: 93-8
3. Clemmensen D, Rasmussen MM, Mosdal C. A retrospective study of infections after primary VP shunt placement in the newborn with myelomeningocele without prophylactic antibiotics. Childs Nerv Syst. 2010. 26: 1517-21
4. Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE. Global hydrocephalus epidemiology and incidence: Systematic review and meta-analysis. J Neurosurg. 2018. 130: 1065-79
5. Kaestner S, Poetschke M, Kehler U, Antes S, Krause M, Deinsberger W. Revision surgery following CSF shunt insertion: How often could it be avoided?. Acta Neurochir (Wien). 2020. 162: 9-14
6. Lim J, Tang AR, Liles C, Hysong AA, Hale AT, Bonfield CM. The cost of hydrocephalus: A cost-effectiveness model for evaluating surgical techniques. J Neurosurg Pediatr. 2019. 23: 109-18
7. McGirt MJ, Leveque JC, Wellons JC, Villavicencio AT, Hopkins JS, Fuchs HE. Cerebrospinal fluid shunt survival and etiology of failures: A seven-year institutional experience. Pediatr Neurosurg. 2002. 36: 248-55
8. Mitchell KA, Zelko I, Shay T, Horen S, Williams A, Luciano M. The impact of hydrocephalus shunt devices on quality of life. J Craniofac Surg. 2021. 32: 1746-50
9. Morton CC, Metcalfe A, Yusuf K, Sibbald B, Wilson RD. The impact of prenatal diagnosis of selected central nervous system anomalies for prenatal counselling based on significant pregnancy morbidity and neonatal outcomes. J Obstet Gynaecol Can. 2019. 41: 166-73.e1
10. Paff M, Alexandru-Abrams D, Muhonen M, Loudon W. Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg Adv Tech Case Manag. 2018. 13: 66-70
11. Pisapia JM, Sinha S, Zarnow DM, Johnson MP, Heuer GG. Fetal ventriculomegaly: Diagnosis, treatment and future directions. Childs Nerv Syst. 2017. 33: 1113-23
12. Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014. 81: 404-10
13. Spader HS, Hertzler DA, Kestle JR, Riva-Cambrin J. Risk factors for infection and the effect of an institutional shunt protocol on the incidence of ventricular access device infections in preterm infants. J Neurosurg Pediatr. 2015. 15: 156-60
14. Sweeney J, Zyck S, Tovar-Spinoza Z, Krishnamurthy S, Chin L, Bodman A. Evidence-based perioperative protocol for ventriculoperitoneal shunt infection reduction at a single institution. World Neurosurg. 2019. 128: e814-22