- Department of Orthopedic Surgery, Institute of Orthopedics “Carlos E. Ottolenghi,” Hospital Italiano de Buenos Aires, Buenos Aires, Argentina,
- Department of Orthopaedics, University of California, Irvine, California, United States,
- Department of Orthopedics, Hospital Español de Mendoza, Mendoza, Argentina,
- Department of Neurosurgery, University of California, Irvine, California, United States.
Correspondence Address:
Gaston Camino-Willhuber, Department of Orthopedic Surgery, Institute of Orthopedics “Carlos E. Ottolenghi,” Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
DOI:10.25259/SNI_641_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gaston Camino-Willhuber1, Sarah Oyadomari2, Jonathan Ochoa2, Fernando Holc1, Alfredo Guiroy3, Hansen Bow4, Sohaib Hashmi2, Michael Oh4, Nitin Bhatia2, Yu-po Lee2. The impact of stratified hypoalbuminemia and dialysis on morbidity/mortality after posterior spinal fusion surgery: An ACS-NSQIP study. 12-Aug-2022;13:359
How to cite this URL: Gaston Camino-Willhuber1, Sarah Oyadomari2, Jonathan Ochoa2, Fernando Holc1, Alfredo Guiroy3, Hansen Bow4, Sohaib Hashmi2, Michael Oh4, Nitin Bhatia2, Yu-po Lee2. The impact of stratified hypoalbuminemia and dialysis on morbidity/mortality after posterior spinal fusion surgery: An ACS-NSQIP study. 12-Aug-2022;13:359. Available from: https://surgicalneurologyint.com/surgicalint-articles/11786/
Abstract
Background: Preoperative optimization in patients undergoing posterior spinal fusion is essential to limit the number and severity of postoperative complications. Here, we, additionally, evaluated the impact of hypoalbuminemia on morbidity and mortality after posterior spinal fusion surgery.
Methods: This retrospective analysis was performed using data from a prospective multicentric database (ACSNSQIP:2015–2020) regarding patients undergoing posterior spinal fusions. Factors studied included; baseline demographics and 30-day postoperative complications (i.e., reoperations, readmissions, and mortality rates).
Results: There were 6805 patients who met the inclusion criteria. They averaged 62 years of age and had an average BMI of 30.2. Within the 30-day postoperative period, 634 (9.3%) sustained complications; 467 (6.9%) were readmitted, 263 (3.9%) required reoperations, and 37 (0.5%) expired. Although multiple preoperative risk factors were analyzed, hypoalbuminemia, severe hypoalbuminemia, and dialysis were the strongest independent risk factors associated with complications (i.e., reoperations, readmissions, and mortality).
Conclusion: Hypoalbuminemia, severe hypoalbuminemia, and dialysis were significant predictors for morbidity and mortality after posterior spinal fusion surgery.
Keywords: Adverse events, Complications, Dialysis, Hypoalbuminemia, Fusion surgery, Mortality, Readmission, Severe hypoalbuminemia
INTRODUCTION
Multiple preoperative risk factors have already been identified as contributing to postoperative complications following posterior spinal fusions.[
MATERIALS AND METHODS
Study design and criteria
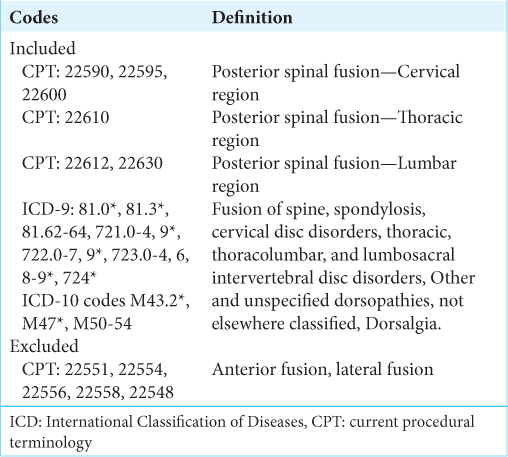
This was a descriptive retrospective study performed using the American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) database for patients undergoing posterior spinal fusions for degenerative disease/ deformity between 2015 and 2020. Patients were selected based on primary Current Procedural Terminology codes, then further filtered based on International Classification of Diseases 9 and 10 codes [
Baseline characteristics
Between 2015 and 2020, 6805 of 16,219 patients from the NSQIP database undergoing posterior spinal fusion met our inclusion criteria. The 3455 males and 3350 females averaged 62 years of age [
Statistical analysis
Outcomes were analyzed utilizing univariate analysis based on demographics, preoperative comorbidities, and other surgical variables. Comparisons were performed using Chi-square tests, Fisher’s exact tests, or Student t-tests.
RESULTS
Overall complications, wound-related complications, and mortality
Notably, 634 patients (9.3%) suffered at least one postoperative complication [
Reoperation and readmission
There were 467 patients (6.9%) who had unplanned readmissions within the 30-postoperative days, with 263 (3.9%) requiring reoperations. Dialysis was the main risk factor for both readmissions (OR = 5.4, P = 0.00) and reoperations (OR = 3, P = 0.025) while hypoalbuminemia was not (i.e., based upon multivariate analysis) [
DISCUSSION
Albumin’s role in healing process
In our study, mild hypoalbuminemia and severe hypoalbuminemia were significantly associated with higher rates of overall complications and mortality compared with normoalbuminemic patients undergoing posterior spinal fusions. These findings are consistent with existing literature.[
Other studies have demonstrated albumin’s role in the healing process and associated hypoalbuminemia with wound-related complications.[
No association between hypoalbuminemia and reoperations/unplanned readmission
Interestingly, we found no significant association between hypoalbuminemia and reoperations or unplanned readmissions. Alternatively, Phan et al.,[
Impact of dialysis
In our study, dialysis was an independent risk factor significantly contributing to complication, readmission, reoperation, and mortality, rates. These findings have been reported in other studies.[
Risk factors increasing mortality rates for spinal fusions
We found other independent risk factors such as operative time, ASA III-IV, thoracic location, and diabetes that increased mortality rates for spinal fusions. However, these factors demonstrated a weaker significant association when compared to hypoalbuminemia and dialysis. These finding were also previously reported in the literature.[
CONCLUSION
Mild hypoalbuminemia, severe hypoalbuminemia, and dialysis significantly increase morbidity and mortality rates for patients undergoing posterior spinal fusions. These results support the fact that albumin levels should be optimized in the preoperative setting to improve outcomes.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adogwa O, Martin JR, Huang K, Verla T, Fatemi P, Thompson P. Preoperative serum albumin level as a predictor of postoperative complication after spine fusion. Spine (Phila Pa 1976). 2014. 39: 1513-9
2. Camino-Willhuber G, Franklin A, Rosecrance K, Oyadomari S, Chan J, Holc F. Preoperative hypoalbuminemia and dialysis increase morbidity/mortality after spine surgery for primary pyogenic spinal infections (ACS-NSQIP Study). Surg Neurol Int. 2022. 13: 193
3. Camino-Willhuber G, Guiroy A, Servidio M, Astur N, NinVilaró F, Alvarado-Gomez F. Unplanned readmission following early postoperative complications after fusion surgery in adult spine deformity: A multicentric study. Global Spine J. 2021. 2192568221991101:
4. Gelfand Y, De la Garza Ramos R, Nakhla JP, Echt M, Yanamadala V, Yassari R. Predictive value of hypoalbuminemia and severe hypoalbuminemia in oncologic spine surgery. Clin Neurol Neurosurg. 2021. 210: 107009
5. Haller C. Hypoalbuminemia in renal failure: Pathogenesis and therapeutic considerations. Kidney Blood Press Res. 2005. 28: 307-10
6. He Z, Zhou K, Tang K, Quan Z, Liu S, Su B. Perioperative hypoalbuminemia is a risk factor for wound complications following posterior lumbar interbody fusion. J Orthop Surg Res. 2020. 15: 538
7. Hori Y, Takahashi S, Terai H, Hoshino M, Toyoda H, Suzuki A. Impact of hemodialysis on surgical outcomes and mortality rate after lumbar spine surgery: A matched cohort study. Spine Surg Relat Res. 2018. 3: 151-6
8. Ottesen TD, McLynn RP, Zogg CK, Shultz BN, Ondeck NT, Bovonratwet P. Dialysis is an independent risk factor for perioperative adverse events, readmission, reoperation, and mortality for patients undergoing elective spine surgery. Spine J. 2018. 18: 2033-42
9. Phan K, Ranson W, White SJ, Cheung ZB, Kim J, Shin JI. Thirty-day perioperative complications, prolonged length of stay, and readmission following elective posterior lumbar fusion associated with poor nutritional status. Global Spine J. 2019. 9: 417-23
10. Willhuber GC, Elizondo C, Slullitel P. Analysis of postoperative complications in spinal surgery, hospital length of stay, and unplanned readmission: Application of Dindo-Clavien classification to spine surgery. Global Spine J. 2019. 9: 279-86