- Athens Medical Center, Athens, Greece,
- Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece.
Correspondence Address:
Stylianos Kapetanakis
Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece.
DOI:10.25259/SNI_581_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Stylianos Kapetanakis, Nikolaos Gkantsinikoudis, Tryfon Thomaidis, Panagiotis Theodosiadis. The role of full-endoscopic lumbar discectomy in patients with neurodegenerative disorders: Technical note and short literature review. 14-Feb-2020;11:23
How to cite this URL: Stylianos Kapetanakis, Nikolaos Gkantsinikoudis, Tryfon Thomaidis, Panagiotis Theodosiadis. The role of full-endoscopic lumbar discectomy in patients with neurodegenerative disorders: Technical note and short literature review. 14-Feb-2020;11:23. Available from: https://surgicalneurologyint.com/surgicalint-articles/9870/
Abstract
Background: Motor neuron disease includes a spectrum of neurodegenerative diseases with progressive courses and unfavorable prognoses. Here, we described a patient with a lumbar disc herniation (LDH) and isolated bulbar palsy (IBP), who successfully underwent a transforaminal full-endoscopic discectomy (TFED) without incurring the added risks of general anesthesia.
Case Description: A 58-year-old male with IBP had an LDH at the L4-L5 level. Avoiding general anesthesia, a TFED was successfully performed under local anesthesia with mild sedation. There were no perioperative complications, and the patient was discharged on the 1st postoperative day. The patient experienced complete relief of radicular symptomatology 1 year postoperatively.
Conclusion: Here, we present a rare instance of a patient with IBP who successfully underwent a TFED for an LDH performed under local anesthesia utilizing mild sedation, avoiding the risks of general anesthesia.
Keywords: Full-endoscopic lumbar discectomy, Lumbar disc herniation, Motor neuron disease, Neurodegenerative disorders, Percutaneous transforaminal endoscopic discectomy
INTRODUCTION
Motor neuron disease (MND) constitutes a group of neurodegenerative disorders that include isolated bulbar palsy (IBP). The clinical picture is characterized by the insidious emergence of dysphagia and dysarthria, with the initial preservation of respiratory function
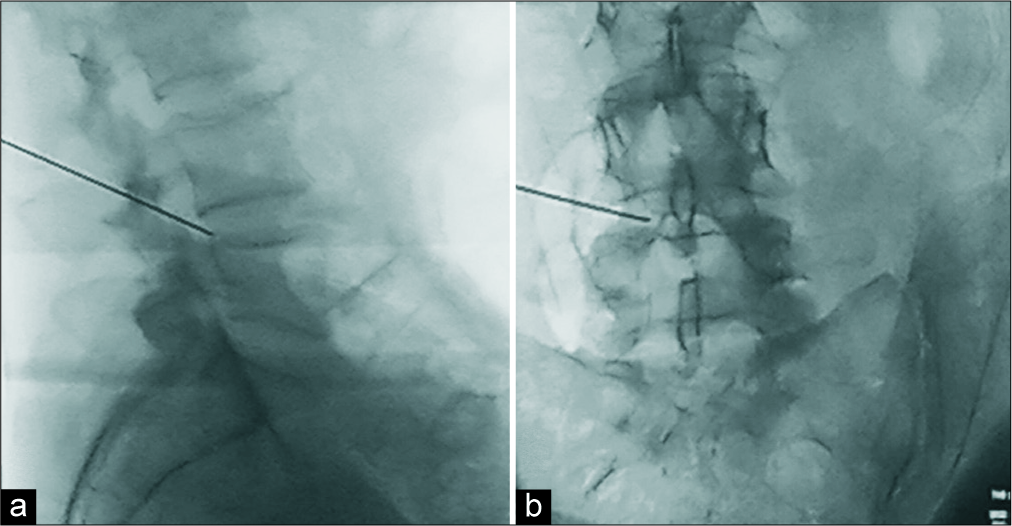
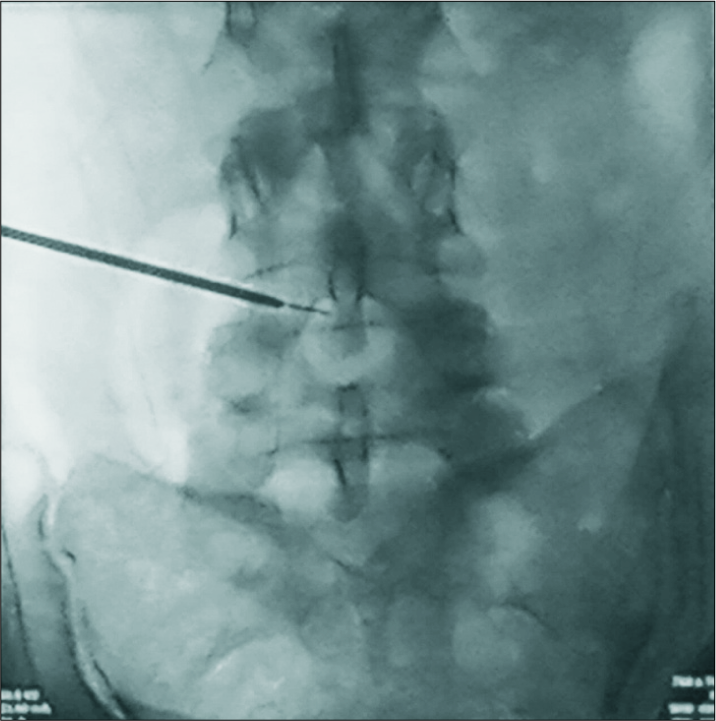
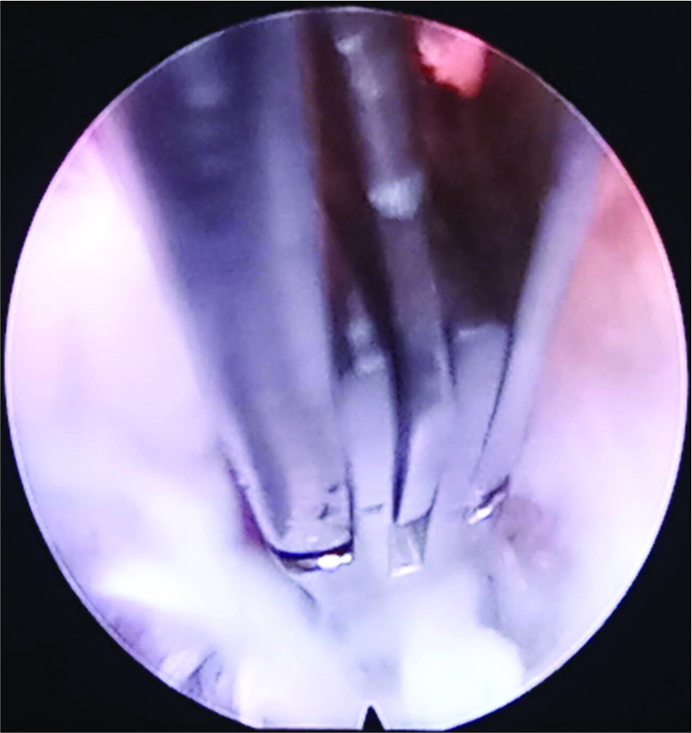
Full-endoscopic lumbar discectomy (FELD) has gained recognition for its preservation of the dorsal musculature/spine elements that minimize intraoperative hemorrhage, thereby reducing perioperative morbidity and more rapid postoperative rehabilitation efforts. Further, advantages include the ability to perform transforaminal full-endoscopic discectomy (TFED) or interlaminar full-endoscopic discectomy under local anesthesia and mild sedation.[
Here, we present a patient with IBP who successfully underwent a TFED for an L4-L5 lumbar disc herniation (LDH) and under local anesthesia.
CASE PRESENTATION
A 58-year-old male with a history of IBP and chronic symptoms of dysphagia/dysarthria over the past 10 years, acutely presented with the right-sided sciatica. Clinically, he had the right L4 and L5 radiculopathy (2/5 weakness/sensory changes).
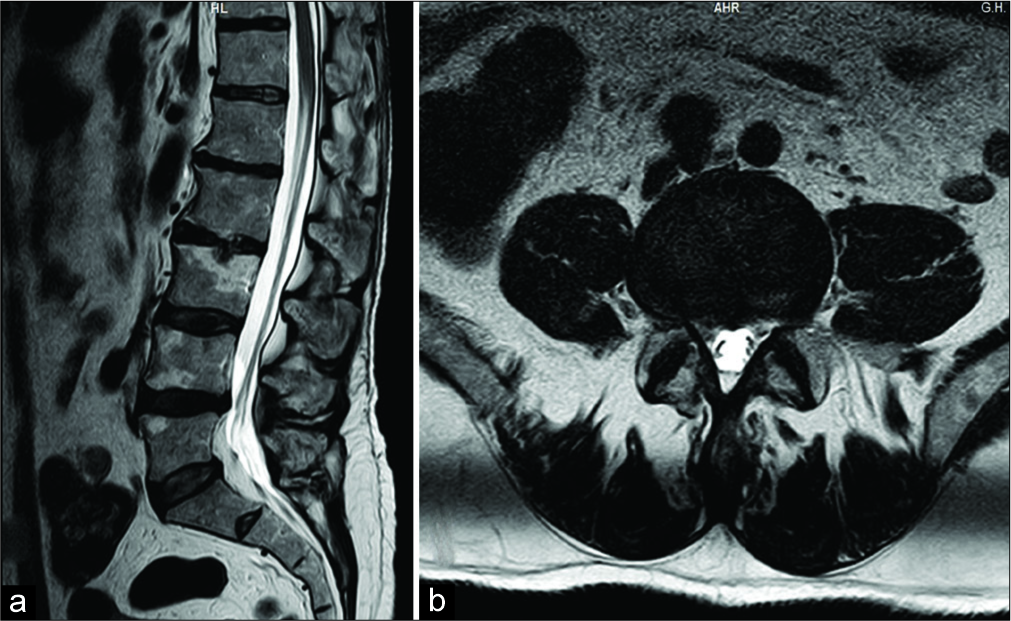
The MR showed a right-sided lateral foraminal-extraforaminal disc herniation at the L4-L5 with mild lateral recess stenosis [
The patient’s postoperative course was uneventful; he was discharged on the 1st postoperative day.
DISCUSSION
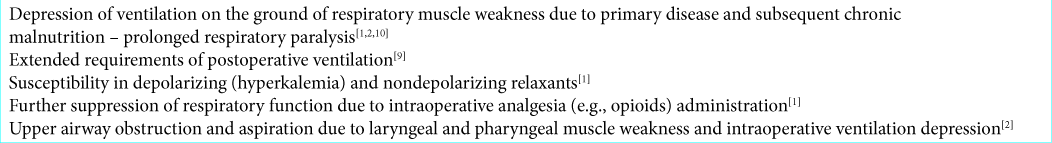
The intraoperative management of IBP constitutes an especial challenge for the surgeon and anesthesiologist. Specifically, there are multiple contraindications for using general anesthesia, for example, significantly burden respiratory system [
We, therefore, performed a minimally invasive TFED (e.g., preservation of dorsal musculature and spine anatomic elements, diminished traumatization, as well as minimization of intraoperative hemorrhage) under local anesthesia with mild sedation.[
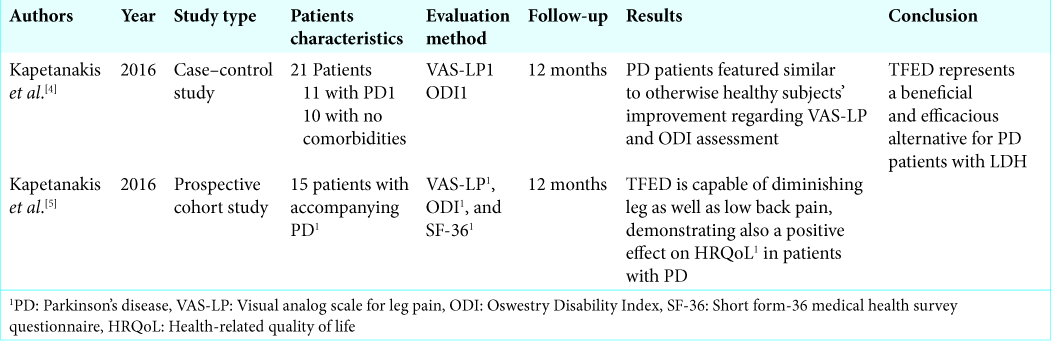
FELD has been performed in other patients with accompanying neurodegenerative disorders/Parkinson’s disease (PD) [
Kapetanakis et al. first described performing TFED for LDH in 11 patients with PD versus ten patients with LDH and no accompanying comorbidities’ comparable clinical improvement were observed in both groups.[
Kapetanakis et al. later prospectively studied 15 patients with PD and LDH for 12 months following TFED. Visual analog scale for leg pain, Oswestry Disability Index, as well as all aspects of SF-36 showed statistically significant improvement 1 year postoperatively and the final outcome was not affected by sex or the operated level.[
CONCLUSION
To our best knowledge, implementation of FELD for LDH in patients with neurodegenerative MND has never been reported in current literature. TFED under local anesthesia and mild sedation was uneventfully performed in a patient with LDH and IBP, for who general anesthesia administration would be remarkably perilous. Postoperative favorable outcomes demonstrate that TFED may be successfully conducted in this patient subgroup, when LDH is present. Nevertheless, further studies with greater population sizes are required in order to delineate the precise role of FELD in these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Gu J, Lin X. Anesthesia and postoperative analgesia for a patient with amyotrophic lateral sclerosis. Minerva Anestesiol. 2017. 83: 1216-7
2. Hadjikoutis S, Wiles CM. Respiratory complications related to bulbar dysfunction in motor neuron disease. Acta Neurol Scand. 2001. 103: 207-13
3. Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res. 1987. 223: 145-54
4. Kapetanakis S, Giovannopoulou E, Charitoudis G, Kazakos K. Transforaminal percutaneous endoscopic discectomy for lumbar disc herniation in parkinson’s disease: A case-control study. Asian Spine J. 2016. 10: 671-7
5. Kapetanakis S, Giovannopoulou E, Thomaidis T, Charitoudis G, Pavlidis P, Kazakos K. Transforaminal percutaneous endoscopic discectomy in parkinson disease: Preliminary results and short review of the literature. Korean J Spine. 2016. 13: 144-50
6. Kapetanakis S, Gkantsinikoudis N, Charitoudis G. The role of full-endoscopic lumbar discectomy in surgical treatment of recurrent lumbar disc herniation: A health-related quality of life approach. Neurospine. 2019. 16: 96-104
7. Kapetanakis S, Gkantsinikoudis N, Papathanasiou JV, Charitoudis G, Thomaidis T. Percutaneous endoscopic ventral facetectomy: An innovative substitute of open decompression surgery for lateral recess stenosis surgical treatment?. J Craniovertebr Junction Spine. 2018. 9: 188-95
8. Kapetanakis S, Gkantsinikoudis N, Thomaidis T, Charitoudis G, Theodosiadis P. The Role of Percutaneous Transforaminal Endoscopic Surgery in Lateral Recess Stenosis in Elderly Patients. Asian Spine J. 2019. 13: 638-47
9. Niyogi S, Mukherjee D, Chakraborty J, Mitra P, Santra S, Acharya A. Anaesthetic management of a patient with motor neuron disease posted for microlaryngeal surgery. J Indian Med Assoc. 2012. 110: 933-4
10. Xiao W, Zhao L, Wang F, Sun H, Wang T, Zhao G. Total intravenous anesthesia without muscle relaxant in a parturient with amyotrophic lateral sclerosis undergoing cesarean section: A case report. J Clin Anesth. 2017. 36: 107-9
11. Zhang HG, Chen L, Tang L, Zhang N, Fan DS. Clinical features of isolated bulbar palsy of amyotrophic lateral sclerosis in Chinese population. Chin Med J (Engl). 2017. 130: 1768-72