- Department of Surgery Dr. Soetomo General-Academic Hospital, Surabaya, Indonesia.
- Department of Urology, Dr. Soetomo General-Academic Hospital, Surabaya, Indonesia.
Correspondence Address:
Illona Okvita Wiyogo, Department of Surgery, Dr. Soetomo General-Academic Hospital, Surabaya, Indonesia.
DOI:10.25259/SNI_615_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Barmadisatrio1, Illona Okvita Wiyogo1, Yudhistira Pradnyan Kloping2. The role of interferential current electrical stimulation in pediatric urology: A systematic review of randomized controlled trials. 24-Nov-2023;14:404
How to cite this URL: Barmadisatrio1, Illona Okvita Wiyogo1, Yudhistira Pradnyan Kloping2. The role of interferential current electrical stimulation in pediatric urology: A systematic review of randomized controlled trials. 24-Nov-2023;14:404. Available from: https://surgicalneurologyint.com/surgicalint-articles/12647/
Abstract
Background: In recent years, interferential current (IFC) electrical stimulation has been studied as a novel treatment for various lower urinary tract dysfunctions in children. As the findings of multiple studies may vary, we aimed to evaluate the current view on IFC in pediatric urology problems based on the findings of randomized clinical trials (RCTs).
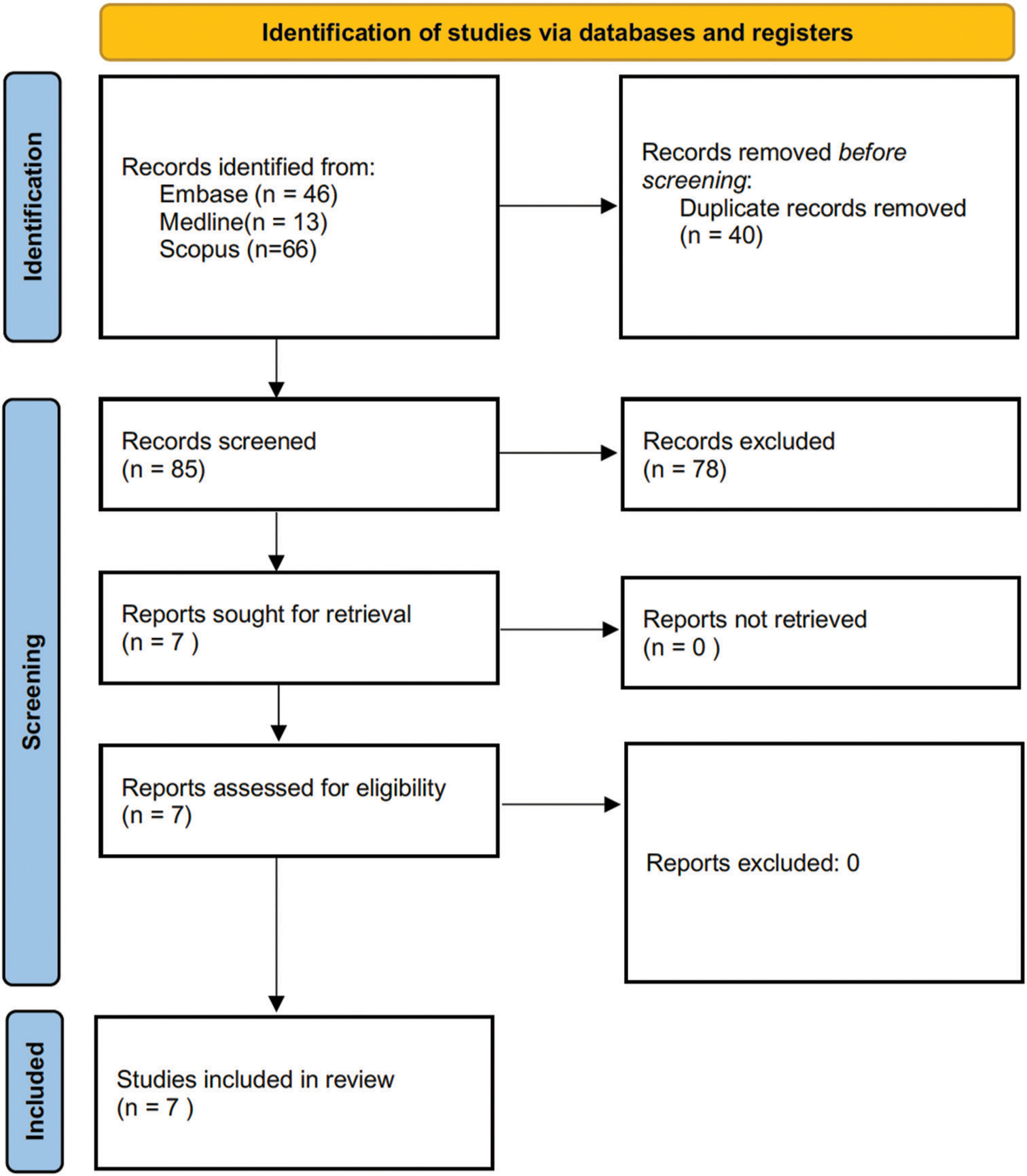
Methods: We performed a systematic search in the Embase, Medline, and SCOPUS databases in accordance with the latest Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines. Eligible studies comprised studies evaluating IFC for lower urinary tract problems in children. The studies’ quality was assessed using the Cochrane risk of bias (RoB) tool 2.
Results: A total of 125 articles were initially obtained, among which 40 articles were duplicates. There were six eligible RCTs with an overall low RoB. All subjects underwent 10–18 sessions of treatment. The outcomes measured consisted of the alleviation of symptoms and urodynamic parameters. The trials reported that 61–90% of patients responded positively to the treatment. Both IFC and transcutaneous electrical nerve stimulation generated improvements in the subjects. However, overall the IFC group showed better immediate and short-term improvement.
Conclusion: IFC is a promising therapy for bladder dysfunction and enuresis in children. More comparative RCTs are required in the future to quantitatively determine the superiority of IFC to other alternatives. The safety aspects of the treatment should also be studied further before it can be used in a clinical setting as the standard and protocol for children are still unclear.
Keywords: Bladder dysfunction, Interferential electrical stimulation, Pediatric urology
INTRODUCTION
Interferential current (IFC) was developed in the 1950s and this is readily observable as a recommended method of reeducating muscle activity.[
These electrical currents, on the other hand, can affect sensory, motor, glandular, and secretory functions as well. Changes in neurotransmitter availability, reducing cholinergic activity, and increasing beta-adrenergic activity have also been reported as an effect of electrical stimulation therapy.[
The most common problem in the referral of children to pediatric urology clinics is lower urinary tract dysfunction (LUTD), including several different conditions such as dysfunctional voiding, urinary incontinence, overacting bladder, and underactive bladder (UAB). This condition requires treatment early in life to optimize a long-term outcome.[
The widespread use of IFC as one of the alternative treatments for several urinary tract problems in children may become an interesting subject for further research. As the findings of multiple studies may vary, we aimed to evaluate the current view on IFC in pediatric urology problems based on the findings of randomized clinical trials (RCTs).
MATERIALS AND METHODS
The search was performed using databases from Embase, Medline, and Scopus by the latest Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines. Literature reviews were done by multiple investigators (IO, YPK, and BS), on three databases: Embase, Medline, and Scopus. The main keywords are (1) “Transcutaneous nerve stimulation or transcutaneous interferential electrical stimulation or transcutaneous electrical nerve stimulation” (TENS), and (2) “Enuresis or nocturnal enuresis,” “1 and 2.”
Randomized control trial studies were included. Identified articles from all databases were screened for duplication. Screening based on title and abstract was done and articles that fulfilled exclusion criteria were further excluded. In the end, eligible articles were included in a qualitative synthesis. Eligible studies that were included in this systematic review are based on the following: Population, intervention, comparison, and outcome criteria. The defined population was children who had a lower urinary tract problem. The intervention was using IFC or another therapy and IFC as a choice. The comparison was using therapy other than IFC. The outcome was an improvement in the condition and complaints of pediatric patients who had a lower urinary tract problem. The study’s quality was assessed using the Cochrane risk of bias tool 2.
RESULTS
A total of 125 studies were identified at the beginning and after a thorough process, six studies were included in this study. Forty studies were excluded due to duplicate records, 78 studies were excluded after screening the title and abstract, and finally, one study was excluded for reasons [
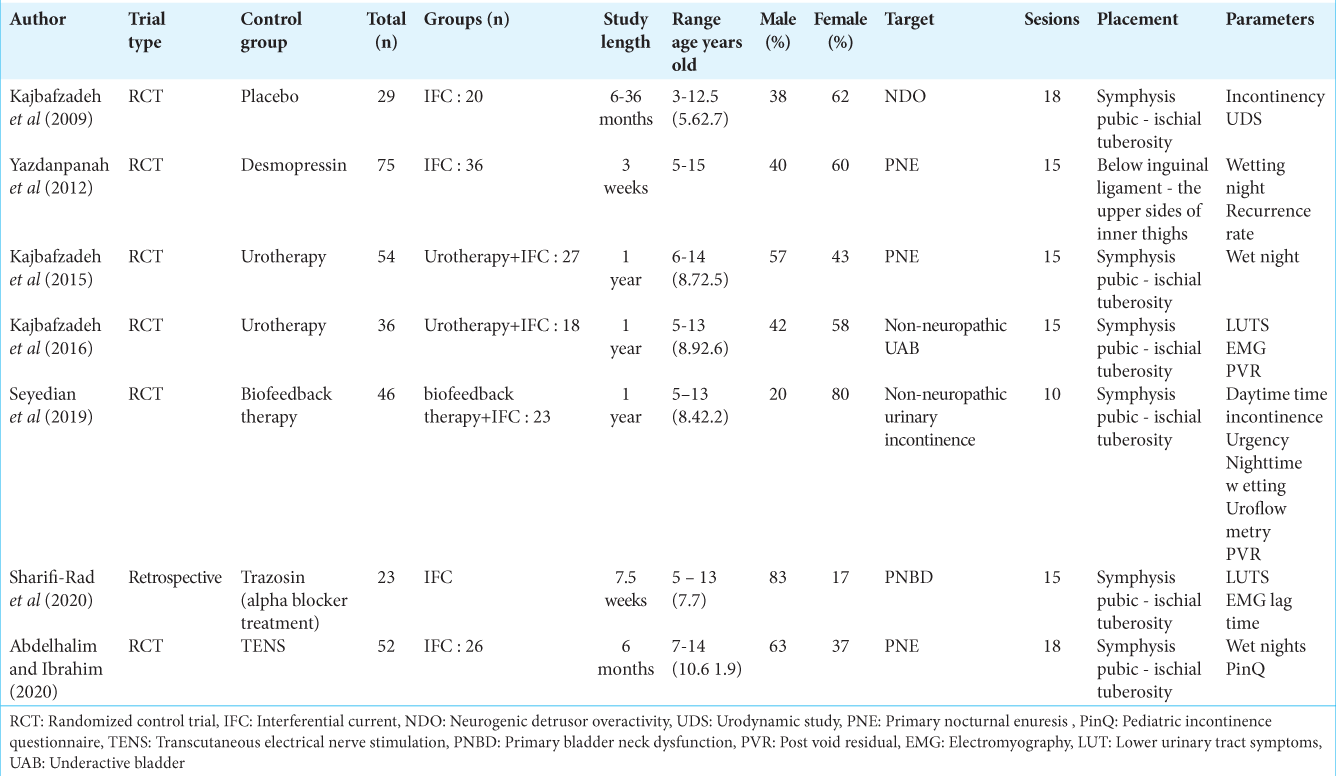
Of the six studies obtained, RCT was used as a research method. Three studies used IFC as the intervention group,[
DISCUSSION
IFC therapy is a challenging procedure, with a lack of published data on its efficacy, especially in children. From the six studies analyzed, a total of 149 children underwent IFC treatment (68 children receive combination therapy), with the youngest patients being 3 years old in Kajbafzadeh et al.’s report.[
From the method and technique perspective, all of the authors mention similar duration, current frequency, and location of the therapy: 20 min session with 250 μs for each shock and 6–6, 6 s of shock repetition, on a low-medium current frequency (4000–4500 Hz), and done in bladder and/or sphincter muscles. In addition, it is preferable to create a strong yet comfortable level of sensory stimulation for the patient during the procedure, without visible muscle contraction or pain complaint. Goats,[
For the IFC result, there was a significant response between IFC therapy and other therapies in treating pediatric patients with lower urinary tract disorders. From these studies, children who were treated using IFC had significantly better results than those who used other therapies. The trials reported that 61–90% of patients responded positively to the therapy. Both IFC and TENS produced improvements in the subjects. However, overall the IFC group showed better improvement in the short-and long-term compared to the TENS group.[
Only half of the studies discussed about complications and safety of the therapy, and most of them stated that no side effects occurred.[
CONCLUSION
IFC is a promising therapy for bladder dysfunction and enuresis in children. More comparative RCTs are required in the future to quantitatively determine the superiority of IFC to other alternatives through a meta-analysis. The safety aspect of the treatment should also be studied further before it can be used in a clinical setting as the standard and protocol for children are still unclear.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdelhalim NM, Ibrahim MM. A comparative study of transcutaneous interferential electrical stimulation and transcutaneous electrical nerve stimulation on children with primary nocturnal enuresis: A randomized clinical trial. Int Urol Nephrol. 2020. 52: 409-15
2. Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn. 2016. 35: 471-81
3. Berry A, Rudick K, Richter M, Zderic S. Objective versus subjective outcome measures of biofeedback: What really matters?. J Pediatr Urol. 2014. 10: 620-6
4. Bower WF, editors. Electrical stimulation. Pelvic floor re-education. London: Springer London; 2008. p. 190-5 Available from: https://link.springer.com/10.1007/978-1-84628-505-9_20 [Last accessed on 2023 Sep 21]
5. de Oliveira LF, de Oliveira DM, da Silva de Paula LI, de Figueiredo AA, de Bessa J, de Sá CA. Transcutaneous parasacral electrical neural stimulation in children with primary monosymptomatic enuresis: A prospective randomized clinical trial. J Urol. 2013. 190: 1359-63
6. Goats GC. Interferential current therapy. Br J Sports Med. 1990. 24: 87-92
7. Huang T, Shu X, Huang YS, Cheuk DK. Complementary and miscellaneous interventions for nocturnal enuresis in children. Cochrane Database Syst Rev. 2011. 12: CD005230
8. Kajbafzadeh AM, Sharifi-Rad L, Baradaran N, Nejat F. Effect of pelvic floor interferential electrostimulation on urodynamic parameters and incontinency of children with myelomeningocele and detrusor overactivity. Urology. 2009. 74: 324-9
9. Kajbafzadeh AM, Sharifi-Rad L, Mozafarpour S, LadiSeyedian SS. Efficacy of transcutaneous interferential electrical stimulation in treatment of children with primary nocturnal enuresis: A randomized clinical trial. Pediatr Nephrol. 2015. 30: 1139-45
10. Kajbafzadeh AM, Sharifi-Rad L, Ladi-Seyedian SS, Mozafarpour S. Transcutaneous interferential electrical stimulation for the management of non-neuropathic underactive bladder in children: A randomised clinical trial. BJU Int. 2016. 117: 793-800
11. Krzemińska K, Maternik M, Drożyńska-Duklas M, Szcześniak P, Czarniak P, Gołębiewski A. High efficacy of biofeedback therapy for treatment of dysfunctional voiding in children. Cent European J Urol. 2012. 65: 212-5
12. Ladi-Seyedian SS, Sharifi-Rad L, Kajbafzadeh AM. Pelvic floor electrical stimulation and muscles training: A combined rehabilitative approach for management of nonneuropathic urinary incontinence in children. J Pediatr Surg. 2019. 54: 825-30
13. Sharifi-Rad L, Ladi-Seyedian SS, Manouchehri N, Alimadadi H, Allahverdi B, Motamed F. Effects of interferential electrical stimulation plus pelvic floor muscles exercises on functional constipation in children: A randomized clinical trial. Am J Gastroenterol. 2018. 113: 295-302
14. Tim W. Electrotherapy: Evidence based practice. Available from: https://site.ebrary.com/id/10511813 [Last accessed on 2023 Sep 21].
15. Tugtepe H, Thomas DT, Ergun R, Kalyoncu A, Kaynak A, Kastarli C. The effectiveness of transcutaneous electrical neural stimulation therapy in patients with urinary incontinence resistant to initial medical treatment or biofeedback. J Pediatr Urol. 2015. 11: 137.e1-5
16. Yazdanpanah P, Ali M, Mehrabi S. Assessment of interferential currents therapy efficacy in management of primary nocturnal enuresis in 5-15 years old children: A randomized clinical trial. J Nov Physiother. 2012. 2: 10-2