- Department of Neurosurgery, Institute of Neurosurgery, Catholic University, Rome, Italy
- Department of Interventional Radiology, Institute of Radiology, Catholic University, Rome, Italy
Correspondence Address:
Nicola Montano
Department of Neurosurgery, Institute of Neurosurgery, Catholic University, Rome, Italy
DOI:10.4103/2152-7806.159490
Copyright: © 2015 Papacci F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Papacci F, Pedicelli A, Montano N. The role of preoperative angiography in the management of giant meningiomas associated to vascular malformation. Surg Neurol Int 29-Jun-2015;6:114
How to cite this URL: Papacci F, Pedicelli A, Montano N. The role of preoperative angiography in the management of giant meningiomas associated to vascular malformation. Surg Neurol Int 29-Jun-2015;6:114. Available from: http://surgicalneurologyint.com/surgicalint_articles/the-role-of-preoperative-angiography-in-the-management-of-giant-meningiomas-associated-to-vascular-malformation/
Abstract
Background:The role of preoperative digital subtraction angiography (DSA) in meningiomas is currently under discussion because of the introduction of noninvasive magnetic resonance imaging (MRI) angiography to study vascular anatomy associated to the tumor. Preoperative DSA is mainly performed to obtain embolization of the lesion, although a number of complications have been reported after this procedure. Nonetheless, the coexistence of meningiomas with vascular malformations has previously been reported and it has been evidenced that this event could be underestimated because of neglect of preoperative DSA. Here, we report on two challenging cases of giant meningiomas associated to vascular malformations and we discuss the pertinent literature.
Case Descriptions:In the first case: A large right temporal meningioma with erosion of the sphenoid greater wing and extension toward infratemporal fossa and right orbit - a large pseudoaneurysm of right middle cerebral artery branch was found end embolized during DSA. In the second case: A giant parieto-temporal meningioma - DSA permitted the full visualization of an abnormal drainage of superior sagittal sinus like a “sinus pericranii” that was respected during the following surgery.
Conclusion:We think that MRI angiography is the exam of choice to study vascular anatomy in meningiomas. Nonetheless, DSA remains a useful tool in giant meningiomas not only to embolizate the lesion but also to treat tumor associated vascular malformation and to achieve the full knowledge of vascular anatomy. We think that a wide communication between interventionalist and surgeon is essential for the optimal management of these patients.
Keywords: Aneurysm, diagnosis, magnetic resonance imaging, meningioma, preoperative angiography, vascular malformations
INTRODUCTION
The usefulness of preoperative digital subtraction angiography (DSA) in meningiomas is currently under discussion. Its role as a diagnostic tool to study vascular abnormal anatomy associated to the tumor has been reduced because of the introduction of magnetic resonance imaging (MRI) angiography.[
CASE REPORTS
Case 1
A 44-year-old female was admitted to our department because of a 3-year history of headache and a progressive worsening of right exophthalmos with a brain MRI showing a giant enhancing right temporal mass with erosion of the sphenoid greater wing and extension toward infratemporal fossa and right orbit [Figure
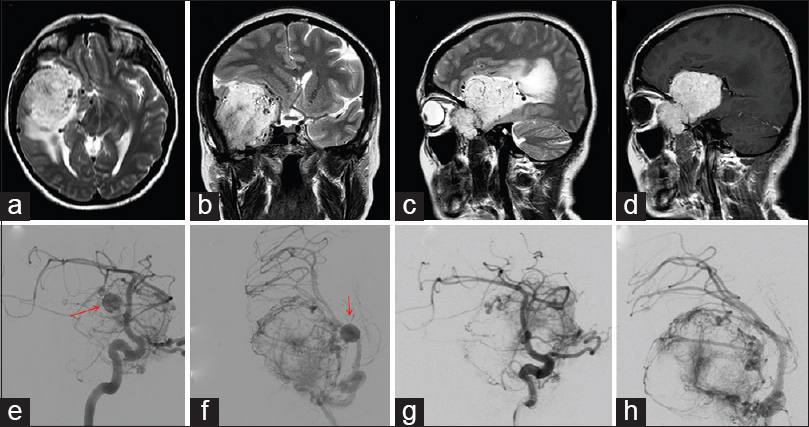
Figure 1
Axial (a), coronal (b) and sagittal (c) T2-weighted brain magnetic resonance imaging showing a large right temporal meningioma with erosion of the sphenoid greater wing and extension toward infratemporal fossa and right orbit. The tumor shows wide enhancement after Gadolinium administration (d). A pseudo-aneurysm of right middle cerebral artery branch before (e and f; red arrow) and after (g and h) embolization with Glubran2 glue
No complication after the DSA was evident. Thus, 3 days later the patient underwent tumor removal by frontotemporal-transzygomatic approach. Postoperative course was uneventful. Histological diagnosis was meningioma (World Health Organization [WHO] I). The patient is in good clinical conditions with no recurrence of meningioma at 3-year follow-up.
Case 2
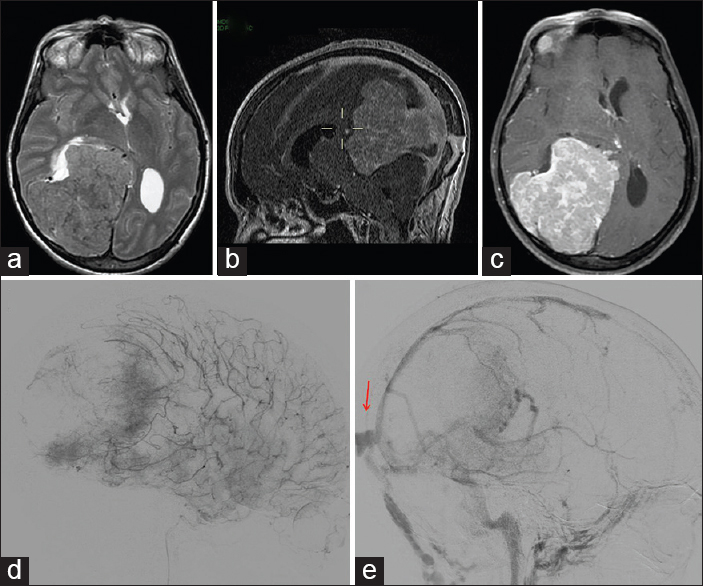
A 50-year-old female was admitted to Emergency Department because of the onset of status epilepticus requiring intubation. Brain MRI with venous angiography showed a parietotemporal enhancing giant mass extending toward pineal region determining mass effect on brain parenchyma, compression of the ventricular system and midline shift with an abnormal vascular drainage of superior sagittal sinus [Figure
Figure 2
Axial T2-weighted (a) brain magnetic resonance imaging (MRI) showing a giant parieto-temporal meningioma enhancing after Gadolinium administration (c). Sagittal MRI venous angiography (b) evidenced an abnormal superior sagittal sinus drainage. Preoperative angiography with embolization of the lesion (d). During venous phase of angiography, the abnormal drainage of superior sagittal sinus like “sinus pericranii” was clearly confirmed (e, red arrow)
DISCUSSION
The role of DSA as a diagnostic tool to study vascular abnormal anatomy associated to meningiomas has been reduced due to the introduction of MRI angiography.[
CONCLUSION
We think that a wide communication between interventionalist and surgeon is essential for the optimal management of these patients in order to identify the appropriate cases to submit to DSA and to avoid the misuse of this procedure that is associated to rare but potentially serious complications.
References
1. Bendszus M, Monoranu CM, Schütz A, Nölte I, Vince GH, Solymosi L. Neurologic complications after particle embolization of intracranial meningiomas. AJNR Am J Neuroradiol. 2005. 26: 1413-9
2. Bozzao A, Finocchi V, Romano A, Ferrante M, Fasoli F, Trillò G. Role of contrast-enhanced MR venography in the preoperative evaluation of parasagittal meningiomas. Eur Radiol. 2005. 15: 1790-6
3. Carli DF, Sluzewski M, Beute GN, van Rooij WJ. Complications of particle embolization of meningiomas: Frequency, risk factors, and outcome. AJNR Am J Neuroradiol. 2010. 31: 152-4
4. Ellis JA, D’Amico R, Sisti MB, Bruce JN, McKhann GM, Lavine SD. Pre-operative intracranial meningioma embolization. Expert Rev Neurother. 2011. 11: 545-56
5. Handa J, Matsuda I, Handa H. Association of brain tumor and intracranial aneurysms. Surg Neurol. 1976. 6: 25-9
6. Javalkar V, Guthikonda B, Vannemreddy P, Nanda A. Association of meningioma and intracranial aneurysm: Report of five cases and review of literature. Neurol India. 2009. 57: 772-6
7. Licata C, Pasqualin A, Freschini A, Barone G, Da Pian R. Management of associated primary cerebral neoplasms and vascular malformations: I. Intracranial aneurysms. Acta Neurochir (Wien). 1986. 82: 28-38
8. Mine B, Delpierre I, Hassid S, De Witte O, Lubicz B. The role of interventional neuroradiology in the management of skull base tumours and related surgical complications. B-ENT. 2011. 7: 61-6
9. Pia HW, Obrador S, Martin JG. Association of brain tumours and arterial intracranial aneurysms. Acta Neurochir (Wien). 1972. 27: 189-204
10. Zhong Z, Sun Y, Lin D, Sun Q, Bian L. Surgical treatment of brain tumor coexisted with intracranial aneurysm – Case series and review of the literature. Neurosurg Rev. 2013. 36: 645-56