- Department of Surgery, Universitas Khairun, Ternate, Indonesia.
Correspondence Address:
Aryandhito Widhi Nugroho, Department of Surgery, Universitas Khairun, Ternate, Indonesia.
DOI:10.25259/SNI_1026_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aryandhito Widhi Nugroho. The start-up of a neurosurgical service in an East Indonesian archipelagic province: The first 2-year experience of North Maluku Database in Neurosurgery (NOMADEN). 16-Feb-2024;15:53
How to cite this URL: Aryandhito Widhi Nugroho. The start-up of a neurosurgical service in an East Indonesian archipelagic province: The first 2-year experience of North Maluku Database in Neurosurgery (NOMADEN). 16-Feb-2024;15:53. Available from: https://surgicalneurologyint.com/surgicalint-articles/12749/
Abstract
Background: Despite encouraging developments after its initial founding in Indonesia more than seven decades ago, inequity in access and availability of neurosurgical services throughout the country continues to pose a challenge. We aimed to elaborate on the start-up of a previously inactive neurosurgical service in North Maluku, an archipelagic province in East Indonesia, and describe cases managed within the first two years of service.
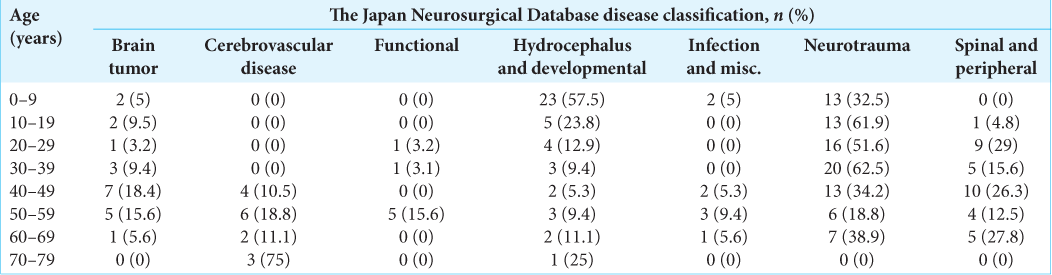
Methods: In the North Maluku Database in the Neurosurgery register, demographic and clinical information of neurosurgical patients admitted to Chasan Boesoirie General Hospital, Ternate, from January 2021 to December 2022, were analyzed. Surgically managed patients were rendered visually according to their decades of life and districts of events.
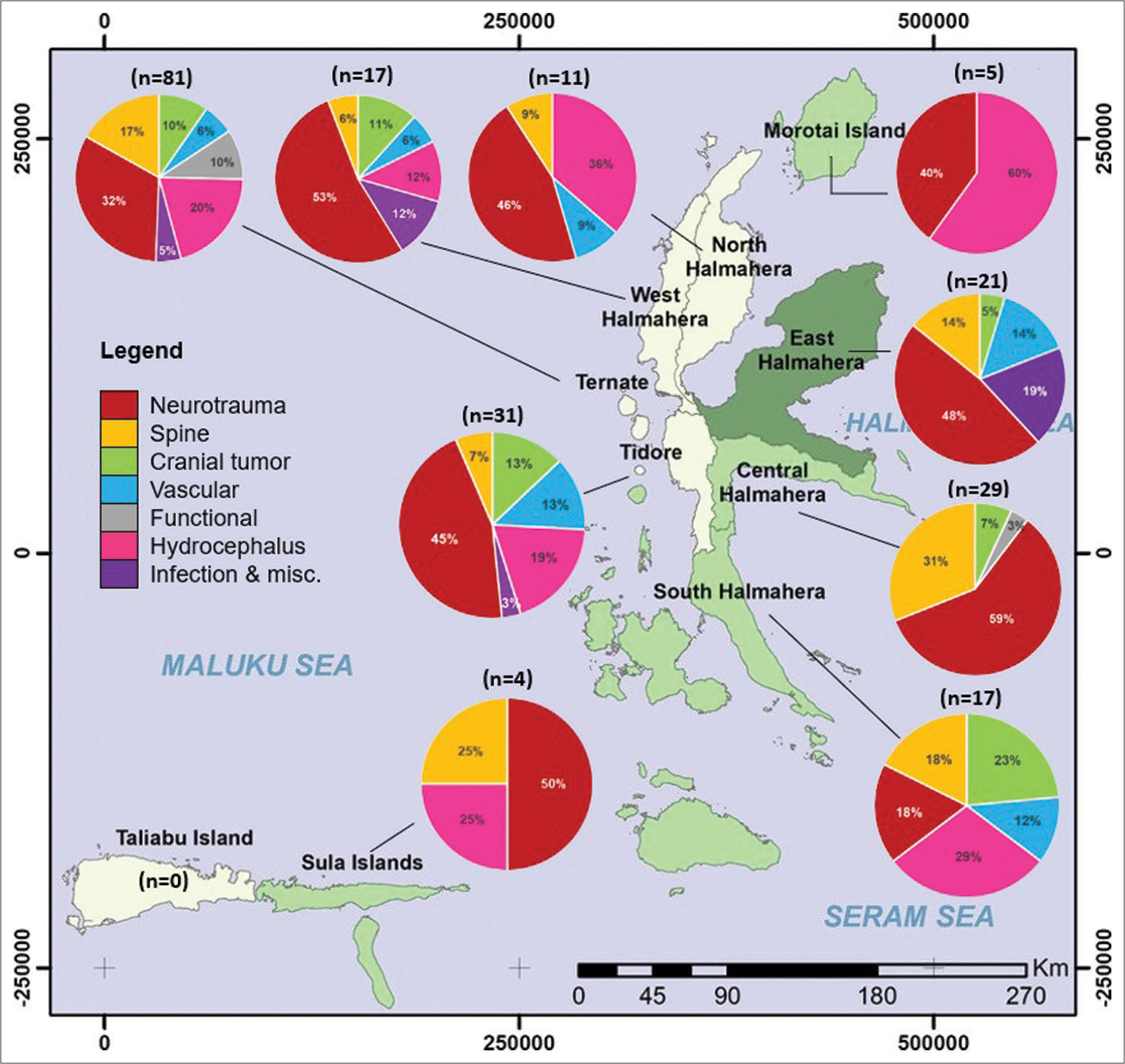
Results: There were 998 new patients (mean age ± standard deviation [SD]: 34.7 ± 19.6 years, 60.3% male) managed and 216 neurosurgical procedures (mean age ± SD: 33 ± 20.4 years, 67.1% male) performed. The majority of patients operated were within the 1st decade of life (18.5%), presented to the emergency room (56.5%), covered by national health insurance (69.4%), from outside Ternate (62.5%), diagnosed with neurotrauma (40.7%), and discharged alive (80.1%). Ternate was the only district where all seven types of neurological diseases were encountered. No surgeries were performed for patients from Taliabu, the farthest district from Ternate.
Conclusion: A large portion of neurosurgical patients in North Maluku were those young and at productive age who were transported from outside Ternate with acute neurological disease (particularly neurotrauma). Distance and geographical circumstances may have a profound effect on access to neurosurgical services.
Keywords: Access, Archipelago, Equity, Neurosurgery, Register
INTRODUCTION
Neurosurgery has always been an indispensable subspecialty of medicine that is demanding not only to its practitioners – neurosurgeons – but also to the whole health and education systems, ensuring its sustainability. It is therefore unsurprising that difficulties in assuring the quality of, availability, and access to neurosurgical services will often be encountered by low- to middle-income countries (LMICs), where the greatest burden of global mortality (78.5%) and disability-adjusted life years (77.3%) due to neurological disorders lie.[
Indonesia, as one of the LMIC countries, has benefited from neurosurgical care for 75 years after its conception in 1948 by Lenshoek, an Indonesian-born Dutch neurosurgeon.[
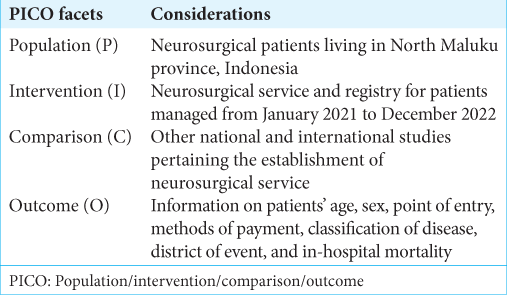
The shortage of basic neurosurgical accouterment, the lack of guarantee of welfare and well-being for neurosurgeons, and the complicated bureaucratic access and protocols may dishearten any attempts to establish neurosurgical service in areas devoid of it. Far from braggadocio, any accounts that apprise the inception of such a framework may inspire and embolden fellow neurosurgeons dealing with similar challenges. Herewith, the author sought to elaborate on the start-up of a previously inactive neurosurgical service in North Maluku, an archipelagic rural province in East Indonesia, and to describe all cases managed within two years of service. The population/intervention/comparison/outcome statement is shown in
MATERIALS AND METHODS
Regional information
North Maluku, formerly renowned as the powerhouse of world spice trade in the 14th–16th century, has a total area of 31,982.50 km2, consisting of 30.9% land and 69.1% sea. Of 1474 islands, only 10% are inhabited. The total population in 2022 is estimated to be 1,319,338 people. There are 147 primary healthcare centers unequally distributed among the islands, with ten public hospitals in each ten districts. Dr. Chasan Boesoirie General Hospital, the only public hospital with neurosurgical capability, is located in Ternate Island, a district with a total area of 162.17 km2 and an estimated population in 2022 of 206,475 people. The other nine districts, with their respective capital, approximate distance to Ternate (in the ascending order), and estimated population in 2022, are Tidore Islands (Tidore; 14.2 km; 118,247), West Halmahera (Jailolo; 36.1 km; 137,541), Central Halmahera (Weda; 73.9 km; 59,096), East Halmahera (Maba; 102.6 km; 94,510), North Halmahera (Tobelo; 125.2 km; 202,755), South Halmahera (Labuha; 157.5 km; 255,795), Morotai Islands (Morotai; 178.7 km; 76,102), Sula Islands (Sanana; 350.9 km; 105,293), and Taliabu Islands (Taliabu; 449.3 km; 58,744). As Ternate is completely separated from other districts by the Molucca Sea, passage thither must be undertaken by boats or ferries. Because a dedicated water ambulance is unavailable, transportation of neurosurgical patients is always delayed, having to conform to the public transportation schedule.
History of establishment
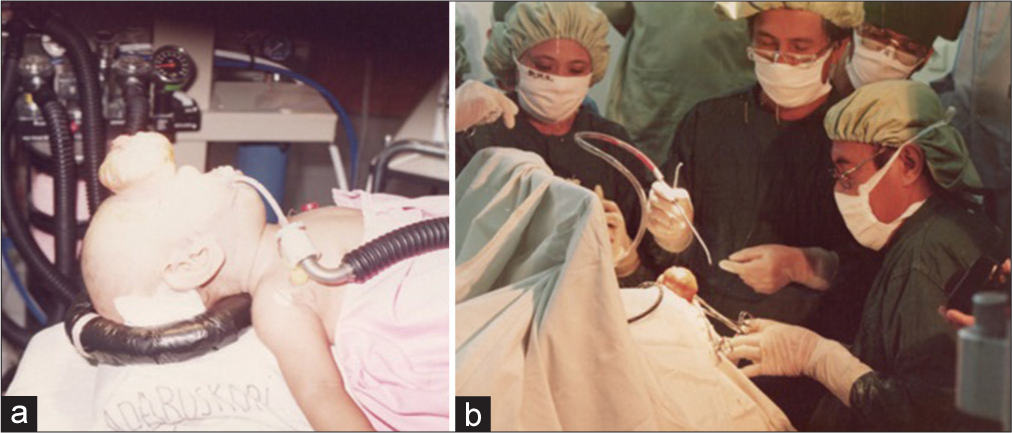
The first step of neurosurgery in the area can be traced back to the year 1993, when Professor R.M. Padmosantjojo performed reconstructive surgery on a 2-year-old anterior meningoencephalocele patient at the invitation of Chasan Boesoirie General Hospital, Ternate. As the public interest in the relatively new and unknown medical condition was high, the event was broadcast live by the local television station [
Figure 1:
The first neurosurgical case managed in North Maluku, Indonesia. (a) A 2-year-old patient who suffered from anterior meningoencephalocele. (b) Professor R.M. Padmosantjojo (sitting) performed surgery with the assistance of Dr. Petonengan, the attending general surgeon (Source: Chasan Boesoirie General Hospital Archive).
Current activity
Because the nature of neurosurgery and its paraphernalia was relatively unknown to everyone in the region, during the 1st year, the author tried to build a good rapport with the hospital management (particularly staff in charge of daily medical service, billing, and procurement), contacted necessary instruments and medical consumables suppliers, and provided public information on neurological diseases and its management (e.g., the importance of wearing helmets and obeying the traffic rule to prevent traumatic brain injury (TBI), the importance of antenatal care and folic acid supplementation to detect congenital disease, e.g., hydrocephalus and dysraphism) through university lectures, local social events, on-air radio shows, etc.
The outpatient clinic is scheduled three times a week, and elective procedures are scheduled two days a week due to the limited capacity of the operating theater. Pre- and postoperative patients are admitted to a shared ward (30 beds) with other surgical specialties. Basic laboratory work-ups (e.g., blood count, electrolyte, and coagulation function) are available, but not cerebrospinal fluid analysis, blood serum culture, gas analysis, or inflammatory marker tests. Histopathological analyses must be done overseas since no in-house pathologist is present. The computed tomography scan was operational until February 2023, after which it malfunctioned due to technical issues. Magnetic resonance imaging is unavailable. All radiological images during the 1st year of service were self-analyzed by the neurosurgeon due to the absence of a radiologist.
Operating theater appurtenances
Three “mock-up” operating theaters are available for all types of general surgeries. These rooms, being originally designed to be admission wards, lacked the essential features of operating theaters, for example, proper surgical lighting, controlled heating-ventilation-air conditioning systems, monitored water sources, and high-efficiency particulate air filters, increasing the risk of bacterial contamination. The lack of basic neurosurgical instruments has caused the author to use self-owned Hudson drills, Gigli wires, Penfield dissectors, shunt passers, and other necessary instruments. No microscope, microsurgical sets, endoscope, head fixation set, or C-arm were procured, and the plight remained until the time this article was written. The intensive care unit is occupied by three anesthesiologists, seven beds, and three ventilator machines that were often inoperable due to technical reasons. Central oxygen supply was unreliable, mobile X-ray was nonexistent, and power outage was a common event. No surgical nursing team had undergone specific neurosurgical nursing experience.
Patients database
The North Maluku Database in Neurosurgery (NOMADEN) is an effort to build a neurosurgical registry in North Maluku, Indonesia, encompassing all types of neurological disorders encountered. Information on age, sex, point of entry, methods of payment, classification of diseases, district of event, and in-hospital mortality from patients managed in Chasan Boesoirie General Hospital, Ternate, from January 2021 to December 2022 were prospectively recorded and cross-matched with the operating room procedure log book and the hospital medical record daily. The point of entry was divided into emergency department, ward (inpatient consultation), and outpatient. Methods of payment consisted of the National Health Insurance (NHI), out-of-pocket, and others (private insurance, social donation, etc.) Classification of diseases was based on the Japan Neurosurgical Database (JND) classifications, that is brain tumor, cerebrovascular diseases, functional, hydrocephalus/developmental anomalies, encephalitis/infection/inflammatory and miscellaneous diseases, neurotrauma, and spinal and peripheral nerve disorders.[
Statistical analysis
Descriptive analyses were performed on two main groups: (i) the overall cohort group, consisting of new patients and their main diagnoses, and (ii) the neurosurgical subgroup, comprising patients who had undergone at least one neurosurgical procedure related to the main diagnosis, with additional procedures related to the subsidiary diagnoses if any. Continuous variables were presented as mean ± standard deviation (SD), and categorical variables as count and percentages. Within each year of service, means of age were compared using the Student’s t-test, while differences between frequencies of categorical variables were examined through the Chi-square test or Fisher’s exact test, whenever appropriate, to test for statistical significance. All analyses were done using IBM Statistical Package for the Social Sciences version 25 software.
RESULTS
The overall cohort group: Basic characteristics
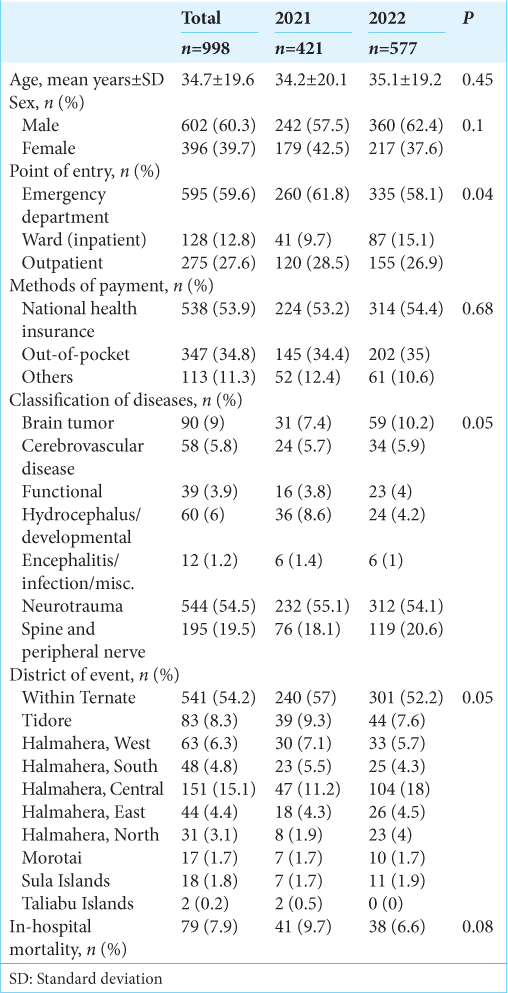
Within the research period, 998 new patients were registered, with a mean age ± SD of 34.7 ± 19.6 years [
The neurosurgical subgroup: Basic characteristics
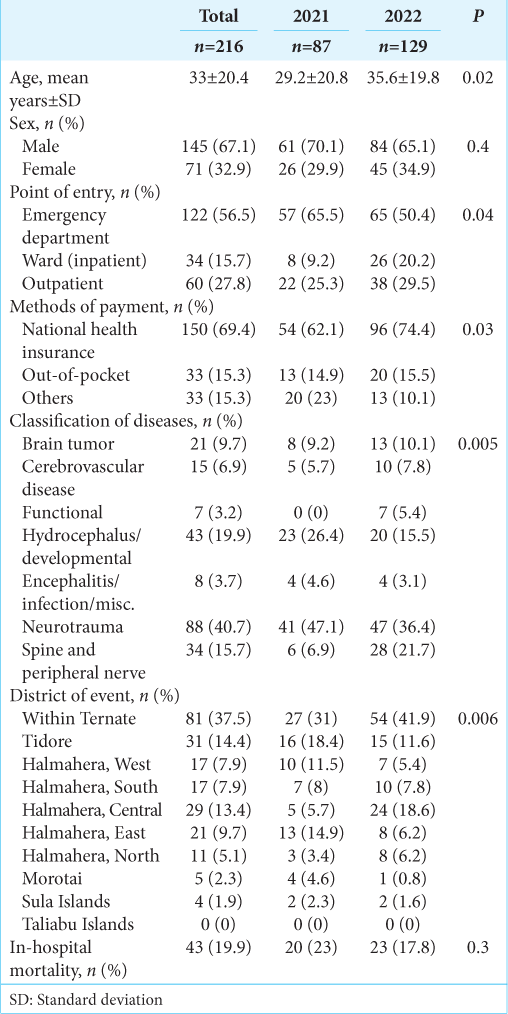
In total, 216 procedures were performed [
The neurosurgical subgroup: Distribution across age decades and districts
Surgery was mostly performed on patients in their 1st decade of life (18.5%), in which group hydrocephalus/developmental anomalies was the most prevalent disease operated [
DISCUSSION
The NOMADEN register
In the era of evidence-based medicine, a patient registry is crucial for the evaluation and sustainment of good medical-surgical practice, educative public information, and effective healthcare policy-making. The NOMADEN register was founded for such purposes. Since the 3rd year of service is currently ongoing, only the first 2-year journey was depicted. To the best of our knowledge, no study from Indonesia has attempted to provide a comparable overview on a provincial level.
Within two years, nearly a thousand new patients were taken care of, with almost a quarter of them experiencing neurosurgical procedures. These were accomplished amid sociodemographic, sociocultural, geographical, and clinical circumstances that might potentially beset the care provision. As a society living in the eastern part of Indonesia, the North Maluku people have different traditional perceptions and beliefs toward disease and procedures from their counterparts in the West.[
Point of entry and methods of payment
The majority of patients were presented to the emergency department, indicating acute conditions necessitating prompt diagnosis and management, conservatively and surgically. Although the state of affairs was manageable at that moment by a single neurosurgeon, who was constantly on alert for 24 hours for two years, this is far from ideal. It is known that there has to be at least one neurosurgeon per 212,000 people to provide neurotrauma management, while in North Maluku, one neurosurgeon was responsible for 1.3 million people.[
In this paper, NHI was identified as the payment method of choice, particularly by those who underwent surgery. This optimal usage of one of the world’s largest single-payer health insurance is in line with the aim stated by the Indonesian government in its introduction in 2014: To achieve Universal Health Coverage for all citizens.[
The neurological disease classification
The JND major classification of diseases was utilized for its generality.[
Neurotrauma: A multifaceted disease
Neurotrauma/TBI was identified as the most prevalent pathology encountered and managed operatively. We postulated that this is most likely related to motorcycle-related road traffic injury (RTI), which is responsible for 72.7% of trauma cases in Indonesia.[
The burden of an archipelagic region
Distance, duration, and mode of transportation are innate issues that arise with North Maluku being a rural archipelagic province. It is suggested that the ideal neurosurgery center is accessible within four hours of disease onset, a goal that those factors may hinder. In this research, it is evident that the number of patients decreased as the distance to the neurosurgery center increased, even reaching zero in the case of Taliabu district. However, with the majority of patients who underwent surgery being referred from outside Ternate (62.5%), expeditious solutions must be found to elevate the quality of care. To objectively identify weaknesses in neurosurgical care accessibility and equity and to provide hard evidence to the government for improvement and support, the author suggests the utilization of geographic information systems and spatial analyses of population, public facilities, and roads in the future, such as one performed in the Maluku province.[
Comparison with similar neurosurgical initiative
Despite its existence in Indonesia for more than seven decades, details about the establishment of neurosurgical enterprises nationally, especially in rural areas, are rarely chronicled and scientifically published. One report by Wicaksono et al., however, provided an exemplary story of how neurosurgery consultants and trainees from Dr. Sardjito General Hospital, Yogyakarta, were able to provide support for three general hospitals located outside Java Island, all devoid of any neurosurgical service, from September 2017 to September 2019.[
Overseas, a study by Farhan et al. about the newly founded neurosurgical service in Gilgit-Baltistan, a remote area in northern Pakistan populated by almost two million people, described nearly parallel circumstances with our study: With limited diagnostic and operative tools, the neurosurgeon single-handedly managed to handle 223 neurosurgical cases in its first two years of service, the majority of which was neurotrauma (46.6%).[
Other Indonesian neurosurgery registries
There are a handful of publications of note from Indonesia that focus on particular neurological diseases managed neurosurgically. Thohar Arifin et al. reported their experience with 589 surgically managed epilepsy patients from 1999 to 2017 in two neurosurgical centers in Semarang, Central Java.[
Future directions and sustainability
Of all neurosurgical cases left unattended globally due to the care deficit, half of which are identified in Southeast Asian countries.[
Limitation and strength
Some notable limitations are identified. This study is a snapshot of the neurosurgical service in North Maluku in the year 2021–2022, the situation of which might have changed by the time the article was published. The study population consisted of patients residing in an archipelagic area in a developing country whose distinct characteristics cannot be generalized to other populations. Selection bias was unavoidable since only those presented to the neurosurgery center were registered, decreasing the study’s representativeness. The actual onset-to-admission or onset-to-surgery time, a factor that influences patients’ outcomes, was not included due to poor information reliability, either verbal (from witnesses or family relatives) or in writing (medical records). Human error might be introduced in the data registration since the author was the one performing clinical and research works altogether, where exhaustion is an inevitable issue. Nonetheless, because no other neurosurgical center exists in the area, this pilot research may be perceived as the only picture of the real-world situation of the neurosurgical service in North Maluku.
CONCLUSION
A large portion of neurosurgery patients in North Maluku were those young and at productive age who were transported from outside Ternate with acute neurological disease (particularly neurotrauma). Distance and geographical circumstances may have a profound effect on access to neurosurgical services. Although barely initiated and laden with problems, great strides have been made in the history of neurosurgery in Indonesia by the presence of this service. The start-up journey may be viewed as a walkthrough for other neurosurgeons facing the same difficulties. Undoubtedly, the education of native neurosurgeons, support from experienced neurosurgeons, national and international medical associations, and, more importantly, the local and central government in forms of clinical and surgical works, knowledge transfers, surgical equipment provision, and funding for patient care are critical for ensuring sustainable service.[
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Suparmi , Achadi EL. Universal health coverage in Indonesia: Concept, progress, and challenges. Lancet. 2019. 393: 75-102
2. Ashraf M, Ashraf N. Underage motorbike driving in Pakistan: A neurosurgical burden heading towards societal disaster. Surg Neurol Int. 2022. 13: 37
3. Corgozinho MM, Montagner MA. Sociodemographic profile of motorcyclists and their vulnerabilities in traffic. Rev Bras Med Trab. 2022. 20: 262-71
4. Corley J, Lepard J, Barthélemy E, Ashby JL, Park KB. Essential neurosurgical workforce needed to address neurotrauma in low-and middle-income countries. World Neurosurg. 2019. 123: 295-9
5. Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA. Global neurosurgery: The current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change. J Neurosurg. 2018. 130: 1055-64
6. Faried A, Bachani AM, Sendjaja AN, Hung YW, Arifin MZ. Characteristics of moderate and severe traumatic brain injury of motorcycle crashes in Bandung, Indonesia. World Neurosurg. 2017. 100: 195-200
7. Farhan M, Alam S, Zulqarnain I, Haider T, Basit J, Imran M. Pattern of neurosurgical cases and procedures in Gilgit Baltistan: Two-year experience at a newly established neurosurgical department. Hosp Pract (1995). 2022. 50: 368-72
8. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborato. Global, regional, and national burden of traumatic brain injury and spinal cord injury 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019. 18: 56-87
9. Gelinne A, Thakrar R, Tranmer BI, Durham SR, Jewell RP, Penar PL. Differential patterns of referral to neurosurgery: A comparison of allopathic physicians, osteopathic physicians, nurse practitioners, physician assistants, and chiropractors. World Neurosurg. 2019. 126: e564-9
10. Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC. The global burden of injury: Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016. 22: 3-18
11. Iihara K, Tominaga T, Saito N, Suzuki M, Date I, Fujii Y. The Japan neurosurgical database: Overview and results of the first-year survey. Neurol Med Chir (Tokyo). 2020. 60: 165-90
12. Indonesian Central Bureau of Statisti, editors. The 2020 regional statistic of north Maluku province. Indonesia: Central Bureau of Statistics; 2021. p.
13. Indonesian Society of Neurosurge, editors. Info PERSPEBSI. Jakarta: PERSPEBSI; 2021. p.
14. Kanmounye US, Nguembu S, Djiofack D, Zolo Y, Tétinou F, Ghomsi N. Patient attitudes toward neurosurgery in low-and middle-income countries: A systematic review. Neurol India. 2021. 69: 12-20
15. Kato Y, Liew BS, Sufianov AA, Rasulic L, Arnautovic KI, Dong VH. Review of global neurosurgery education: Horizon of neurosurgery in the developing countries. Chin Neurosurg J. 2020. 6: 19
16. Korps Lalu Lintas Kepolisian Negara Republik Indones, editors. Jumlah data kendaraan di Kepolisian Daerah Maluku Utara. Indonesia: Korlantas POLRI; 2022. p.
17. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, RoderDeWan S. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob Health. 2018. 6: e1196-252
18. Lartigue JW, Dada OE, Haq M, Rapaport S, Sebopelo LA, Senyuy WP. Emphasizing the role of neurosurgery within global health and national health systems: A call to action. Front Surg. 2021. 8: 690735
19. Lenshoek CH. Over neurochirurgie in Indonesië [About neurosurgery in Indonesia]. Med Maandbl. 1948. 43: 535-41
20. Leosari Y, Uelmen JA, Carney RM. Spatial evaluation of healthcare accessibility across archipelagic communities of Maluku Province, Indonesia. PLOS Glob Public Health. 2023. 3: e0001600
21. Mediratta S, Lepard JR, Barthélemy EJ, Corley J, Park KB. Barriers to neurotrauma care in low-to middle-income countries: An international survey of neurotrauma providers. J Neurosurg. 2021. 137: 789-98
22. Park KB, Johnson WD, Dempsey RJ. Global neurosurgery: The unmet need. World Neurosurg. 2016. 88: 32-5
23. Prasetya M, Adidharma P, Sulistyanto A, Inoue T, Arham A. Characteristics of patients with trigeminal neuralgia referred to the Indonesian National Brain Center Neurosurgery Clinic. Front Surg. 2022. 8: 747463
24. Pratiwi AB, Setiyaningsih H, Kok MO, Hoekstra T, Mukti AG, Pisani E. Is Indonesia achieving universal health coverage? Secondary analysis of national data on insurance coverage, health spending and service availability. BMJ Open. 2021. 11: e050565
25. Punchak M, Mukhopadhyay S, Sachdev S, Hung YC, Peeters S, Rattani A. Neurosurgical care: Availability and access in low-income and middle-income countries. World Neurosurg. 2018. 112: e240-54
26. Riskesd, editors. Riset kesehatan dasar 2018 [Basic health research 2018]. Indonesia: Kementrian Kesehatan Republik Indonesia; 2018. p. 1-100
27. Rosyidi RM, Priyanto B, Laraswati NK, Islam A, Hatta M, Bukhari A. Characteristics and clinical outcome of traumatic brain injury in Lombok, Indonesia. Interdiscip Neurosurg. 2019. 18: 100470
28. Sobana M, Halim D, Ardisasmita MN, Imron A, Gamyani U, Achmad TH. Periventricular hypodensity is associated with the incidence of pre-shunt seizure in hydrocephalic children. Childs Nerv Syst. 2022. 38: 1321-9
29. Tandian D, Harlyjoy A, Nugroho SW, Ichwan S. Risk factors associated with post-therapeutic outcome for medulloblastoma: An experience from Indonesia. Asian J Neurosurg. 2021. 16: 494-9
30. Thohar Arifin M, Hanaya R, Bakhtiar Y, Bintoro AC, Iida K, Kurisu K. Initiating an epilepsy surgery program with limited resources in Indonesia. Sci Rep. 2021. 11: 5066
31. Wahyuhadi J, Pratama MF, Wathoni RT, Basuki H. The Indonesian central nervous system tumors registry (Ina-CTR): 7 years result from single institution of primary brain tumor epidemiology. Indones J Neurosurg. 2021. 4: 25-35
32. Wicaksono AS, Tamba DA, Sudiharto P, Basuki E, Pramusinto H, Hartanto RA. Neurosurgery residency program in Yogyakarta, Indonesia: Improving neurosurgical care distribution to reduce inequality. Neurosurg Focus. 2020. 48: E5
33. Widayanti AW, Green JA, Heydon S, Norris P. Health-seeking behavior of people in Indonesia: A narrative review. J Epidemiol Glob Health. 2020. 10: 6-15