- Department of Neurosurgery, College of Medicine, Neurosciences Hospital, University of Baghdad, Iraq.
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq.
- Department of Emergency, Neurosciences Hospital, Baghdad, Iraq.
Correspondence Address:
Samer S. Hoz
Department of Emergency, Neurosciences Hospital, Baghdad, Iraq.
DOI:10.25259/SNI_361_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Moneer K. Faraj1, Samer S. Hoz2, Amjad J. Mohammad3. The use of three-dimensional anatomical patient-specific printed models in surgical clipping of intracranial aneurysm: A pilot study. 11-Nov-2020;11:381
How to cite this URL: Moneer K. Faraj1, Samer S. Hoz2, Amjad J. Mohammad3. The use of three-dimensional anatomical patient-specific printed models in surgical clipping of intracranial aneurysm: A pilot study. 11-Nov-2020;11:381. Available from: https://surgicalneurologyint.com/surgicalint-articles/10391/
Abstract
Background: In the present study, we aim to develop simulation models based on computed tomography angiography images of intracranial aneurysms (IAs) and their parent vessels using three-dimensional (3D) printing technology. The study focuses on the value of these 3D models in presurgical planning and intraoperative navigation and ultimately their impact on patient outcomes. To the best of our knowledge, this is the first report of its kind from a war-torn country, like Iraq.
Methods: This is a prospective study of a series of 11, consecutively enrolled, patients suffering from IAs for the period between February and September 2019. The study represents a collaboration between the two major neurosurgical centers in Baghdad/Iraq; Neurosciences Teaching Hospital and Neurosurgery Teaching Hospital. We analyzed the data of eleven patients with IAs treated by microsurgical clipping. These data include patient demographics, clinical, surgical, and outcomes along with the data of the 3D-printed replica used in these surgeries. All cases were operated on by one surgeon.
Results: Our study included 11 patients, with a total of 11 aneurysms clipped. The mean age was 44 ± 8, with a median of 42.5 and a range of 35–61 years. About 60% of our patients were female with a female-to-male ratio of 1:5. About 60% of the aneurysms were located at the anterior communicating artery (Acom) while the remaining 40% were equally distributed between the posterior communicating and internal carotid arteries bifurcation. The standard pterional approach was followed in 50% of cases, whereas the other 50% of patients were treated through the lateral supraorbital approach. About 90% (n = 9) of the patients had a Glasgow Outcome Scale (GOS) of 5 and 10% had a GOS of 4. The 3D-printed models successfully replicated the aneurysm size, location, and relation to the parent vessel with 100% accuracy and were used for intraoperative guidance. The average production time was 24–48 h and the production cost was 10–20 US dollars.
Conclusion: 3D printing is a promising technology that is rapidly penetrating the field of neurosurgery. In particular, the use of 3D-printed patient-matched, anatomically accurate replicas of the cerebral vascular tree is valuable adjunct to the microsurgical clipping of IAs, and our study conclusions support this concept. However, both the feasibility and clinical utility of 3D printing remain the subject of much, ongoing investigations.
Keywords: Aneurysm surgery, Neurosurgery, Rapid prototyping, Three-dimensional printing
INTRODUCTION
Intracranial aneurysms (IAs) are localized dilatations in the cerebral vasculature with an inherently high risk of rupture, resulting in subarachnoid hemorrhage (SAH); a devastating form of hemorrhagic stroke. The overall prevalence of IAs in adults without specific risk factors for SAH is estimated to be between 2% and 3.2%.[
The management guidelines for both ruptured and unruptured IAs are continuously evolving. To date, the two main treatment modalities for IAs include microsurgical clipping and endovascular coil embolization. Several multicenter, randomized, controlled trials have compared the relative safety and efficacy of each treatment strategy; including the International Subarachnoid Aneurysm Trial, the Barrow Ruptured Aneurysm Trial, and the Prospective Registry of Subarachnoid Aneurysms Treatment, among others.[
As evident from the aforementioned trials, neurosurgical treatment for IAs is here to stay, despite the development of the more attractive, less invasive strategies. However, it is also true that the rate of intraoperative rupture (IOR) during IA clipping is almost quadruple that of endovascular coiling; 19% and 5%, respectively, as per the IA Rupture After Treatment study.[
The field of neurovascular surgery has been revolutionized by the introduction of modern stereo imaging modalities such as computed tomography angiography (CTA) and digital subtraction angiography (DSA). However, a significant gap between the details revealed by these conventional imaging modalities and the in vivo anatomy still exists;[
In August 1984, Charles W Chuck filed a patent for “Apparatus for production of 3D objects by Stereolithography” and was subsequently accredited with the invention of the world’s first 3D printer (US Patent 4,575,330, 1986.).[
Over the subsequent decades, the 3D printing technology was enthusiastically embraced by several industries, with the health-care sector being at the forefront. The 3D printing technology relies on the principle of “additive manufacture” (AM), whereby successive layers of material are “printed” to create a 3D replica of a complex computer-designed model.
The main applications for 3D printing in surgery are (1) research and simulation-based teaching, (2) surgical planning, and (3) building tailor-made patient implants.[
As an educational tool, 3D simulation models have been successfully trialed by multiple neurosurgery residency programs. These models offer an immersive virtual reality environment for junior neurosurgeons, enabling them to hone their skills in a controlled, standardized, and minimum risk setting.[
In the operating room, personalized, patient-matched, 3D models are being increasingly acknowledged as indispensable assets to the operating neurosurgeon. Throughout the operation, the ex vivo use of these models is highly valuable in maintaining the surgeon’s orientation, particularly concerning the aneurysm’s size, location, angulation, and parent vessel geometry; this is especially valuable in cases that involve complex and variant vascular anatomy.[
In the present study, we aim to develop simulation models based on CTA images of IAs and their parent vessels using 3D printing technology. The study focuses on the value of these 3D models in presurgical planning and intraoperative navigation and ultimately their impact on patient outcomes. To the best of our knowledge, this is the first report of its kind from Iraq.
MATERIALS AND METHODS
This is a prospective study of a series of 11, consecutively enrolled, patients suffering from IAs for the period between February and September 2019. The study represents a collaboration between the two major neurosurgical centers in Baghdad/Iraq; Neurosciences Teaching Hospital and Neurosurgery Teaching Hospital. We analyzed the data of 11 patients with IAs treated by microsurgical clipping. These data include patient demographics, clinical, surgical, and outcomes along with the data of the 3D-printed replica used in these surgeries. All cases were operated on by one surgeon.
The generation and postprocessing of CTA data
Dynamic CTA images procured. We used the following parameters, slice thickness, 1 mm; the field of view 240 mm.
Images exported in standard digital imaging (DICOM) format to the 3D calculation software (3D Slicer). The bones outside the field of interest, soft tissues, and brain tissue removed. The vascular and nearby bone area segmented by the software the virtual 3D angiogram generated. The skull, intracranial artery and aneurysm distinguished in different colors. Data from the segmented area exported in STL format to the XYZ printer software to produce a patient-specific prototype.
The manufacturing process of the 3D-printed models
We used two types of materials to produce the prototype. They were prerequisites by the printing machine itself. They were PLA and ABS filaments. These are semi-rigid and rigid, respectively. Eleven new models fabricated.
Preoperative planning
In the preoperative period, the vascular neurosurgeon suggested the ideal surgical approach for each model. The 3D models were used to simulate the route to reach the target aneurysm and to determine the size and shape of the clip for the aneurysms. The model-based preoperative plans were compared with the CTA-based, planned, surgical approach to examine the value of the model in preoperative planning.
RESULTS
Our study included 11 patients, with a total of 11 aneurysms clipped. The mean age was 44 ± 8, with a median of 42.5 and a range of 35–61 years. About 60% (n = 6) of our patients were female with a female-to-male ratio of 1.5. About 60% (n = 6) of the aneurysms were located at the Acom while the remaining 40% (n = 4) were equally distributed between the posterior communicating artery and the internal carotid artery bifurcation. The standard pterional approach for aneurysm clipping was followed in 50% (n=5) of cases, whereas the other 50% of patients (n = 5) were treated through the lateral supraorbital approach. Intraoperative aneurysm rupture occurred in 30% of the surgeries (n = 3). About 90% (n = 9) of the patients had a GOS of 5 and 10% (n = 1) had a GOS of 4. All surgeries were performed by the same surgeon. The 3D-printed models successfully replicated the aneurysm size, location, and relation to the parent vessel with a 100% accuracy and were used for intraoperative guidance [
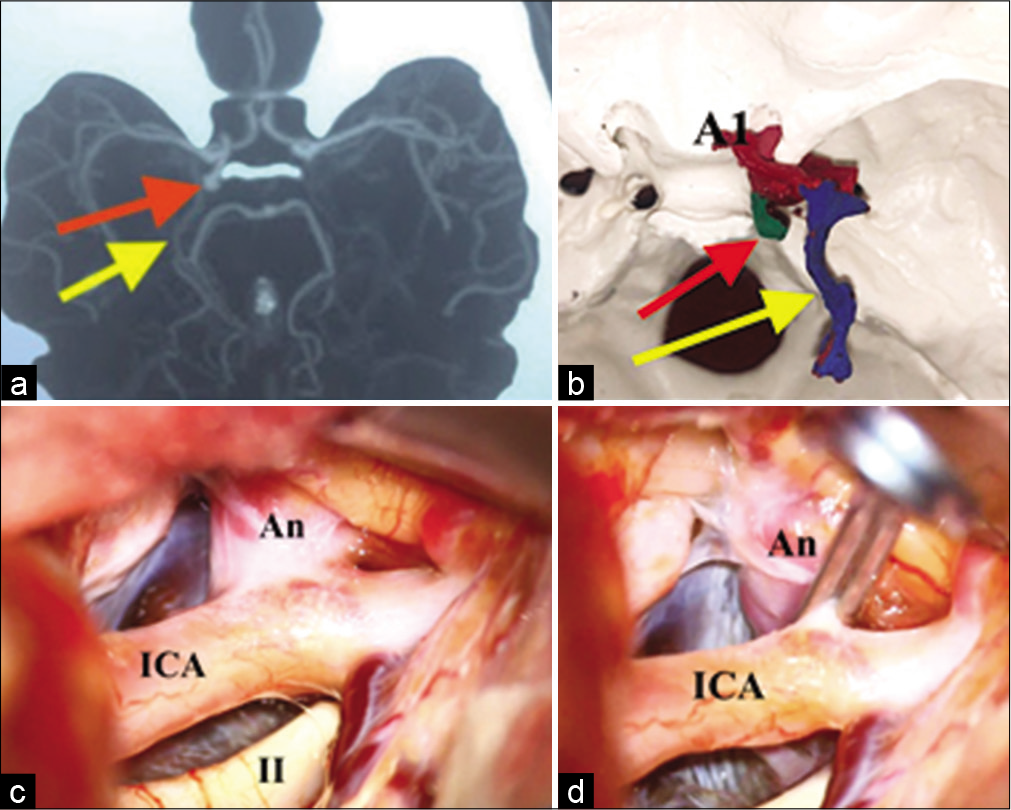
Figure 1:
Images showing the comparison between: (a) the CT angiography image of (5 mm) posterolateral directed right posterior communicating artery aneurysm. The aneurysm (red arrow) and the basal vein of Rosenthal (yellow arrow). (b) 3D physical prototyped biomodel, (c) the intraoperative finding, before the clipping (c) and after the clipping (d). A1: Anterior cerebral artery, precommunicating segment. An: Aneurysm. ICA: Internal carotid artery. II: Optic nerve.
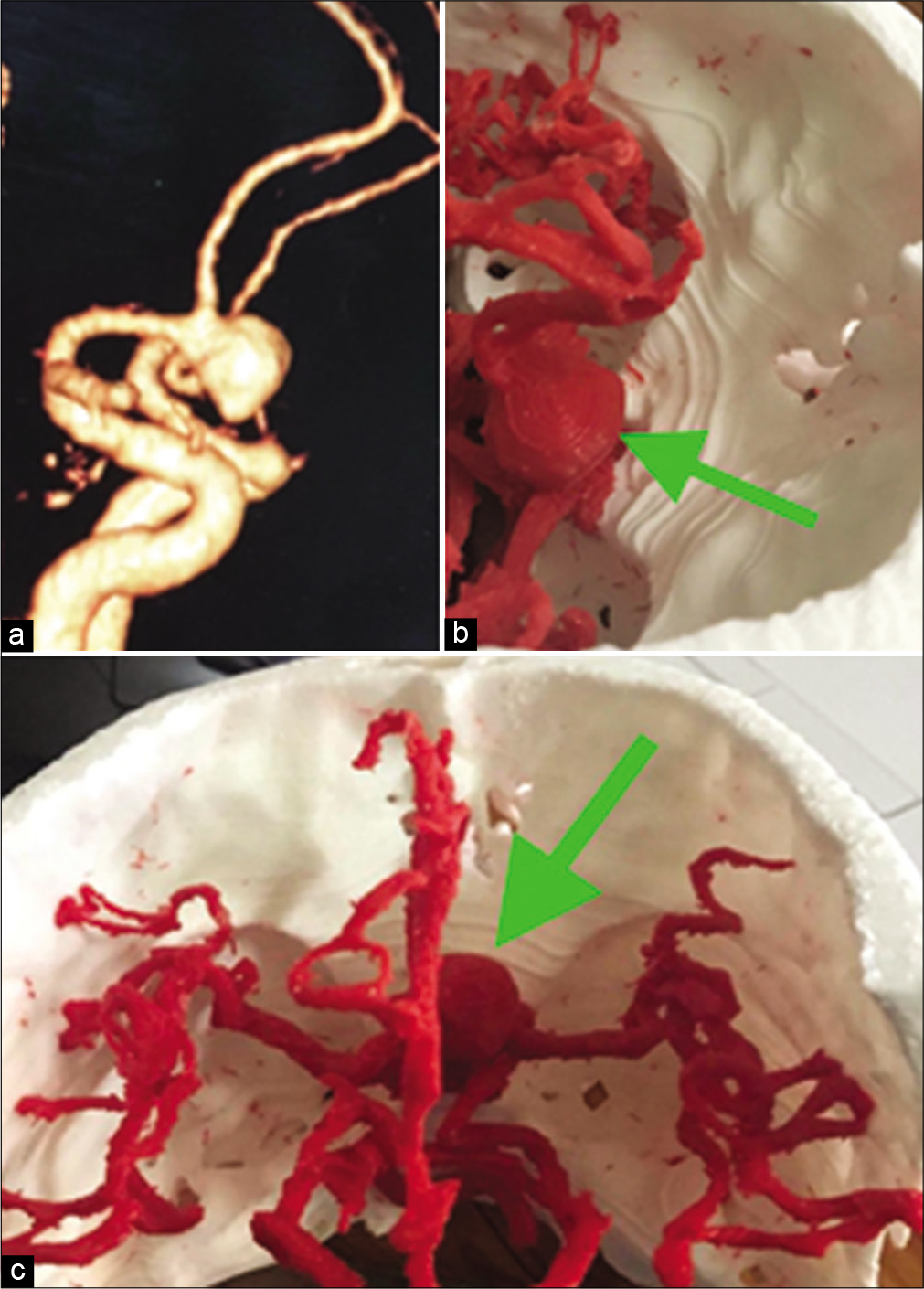
Figure 2:
A case of large anterior communicating artery aneurysm. CT angiography three-dimensional (3D) reconstructed image (a). The 3D prototyped biomodel of the aneurysm, surrounding arteries and the skull base viewed from different angle to enhance preoperative planning and thus intraoperative orientation (b and c). Green arrow: Aneurysm.
DISCUSSION
The 3D printing technology is rapidly gaining popularity among neurosurgeons due to its promising potential to improve patient care. Although numerous proof-of-principle reports have confirmed the safety, efficacy, feasibility, accuracy, reproducibility, and cost-effectiveness of 3D printing in vascular neurosurgery,[
Our 3D-printed replicas exhibited good correlation with the real anatomy in all cases; a finding replicated in almost all studies that examined the use of 3D-printed constructs in vascular neurosurgery.[
It is also worth noting that, in this particular study, the source images were obtained using CTA data; none of the cases underwent DSA; this is in contrast to the majority of similar type studies where DSA was the primary source of images.[
The average manufacturing time was 24–48 h per model, measured from the obtainment of the CTA image to the last step in the production of the final 3D product. Zhao et al. reported an average manufacturing time of 20 h.[
The type of materials we used, which were mandated by the type of the 3D printer, meant that the final constructs were too rigid and brittle to be compared to human vessels. Thus, the models were not amenable to the practice of vessel dissection and clipping. As our study aim focuses on the utility of the models in surgical guidance more so than training, the models were sufficient for our purposes. Nonetheless, using different resins can produce more flexible aneurysms that closely match reality with extended applicability for simulation and training purposes. A similar limitation was initially reported by Kang et al. who subsequently replicated their experiment to create models of flexible aneurysms enclosed in rigid skulls. According to the authors, these human-like models ultimately enabled an immersing virtual reality for surgeons allowing them to practice both craniotomy and clipping.[
CONCLUSION
3D printing is a promising technology that is rapidly penetrating the field of neurosurgery. In particular, the use of 3D-printed patient-matched, anatomically accurate replicas of the cerebral vascular tree is valuable adjunct to the microsurgical clipping of IAs, and our study conclusions support this concept. However, both the feasibility and clinical utility of 3D printing remain the subject of much, ongoing investigations.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anderson JR, Thompson WL, Alkattan AK, Diaz O, Klucznik R, Zhang YJ. Three-dimensional printing of anatomically accurate, patient specific intracranial aneurysm models. J Neurointerv Surg. 2016. 8: 517-20
2. Clarke M. Systematic review of reviews of risk factors for intracranial aneurysms. Neuroradiology. 2008. 50: 653-64
3. Elijovich L, Higashida RT, Lawton MT, Duckwiler G, Giannotta S, Johnston SC. Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: The CARAT study. Stroke. 2008. 39: 1501-6
4. Gölitz P, Struffert T, Knossalla F, Saake M, Ott S, Ganslandt O. Angiographic CT with intravenous contrast injection compared with conventional rotational angiography in the diagnostic work-up of cerebral aneurysms. AJNR Am J Neuroradiol. 2012. 33: 982-7
5. Ionita CN, Mokin M, Varble N, Bednarek DR, Xiang J, Snyder KV. Challenges and limitations of patient-specific vascular phantom fabrication using 3D Polyjet printing. Proc SPIE Int Soc Opt Eng. 2014. 9038: 90380M
6. Khan IS, Kelly PD, Singer RJ. Prototyping of cerebral vasculature physical models. Surg Neurol Int. 2014. 5: 11
7. Kim JA, Kim HN, Im SK, Chung S, Kang JY, Choi N. Collagen-based brain microvasculature model in vitro using three-dimensional printed template. Biomicrofluidics. 2015. 9: 024115
8. Kondo K, Nemoto M, Masuda H, Okonogi S, Nomoto J, Harada N. Anatomical reproducibility of a head model molded by a three-dimensional printer. Neurol Med Chir (Tokyo). 2015. 55: 592-8
9. Lanzino G, Murad MH, d’Urso PI, Rabinstein AA. Coil embolization versus clipping for ruptured intracranial aneurysms: A meta-analysis of prospective controlled published studies. AJNR Am J Neuroradiol. 2013. 34: 1764-8
10. Mashiko T, Otani K, Kawano R, Konno T, Kaneko N, Ito Y. Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 2015. 83: 351-61
11. McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P. The barrow ruptured aneurysm trial. J Neurosurg. 2012. 116: 135-44
12. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005. 366: 809-17
13. Namba K, Higaki A, Kaneko N, Mashiko T, Nemoto S, Watanabe E. Microcatheter shaping for intracranial aneurysm coiling using the 3-dimensional printing rapid prototyping technology: Preliminary result in the first 10 consecutive cases. World Neurosurg. 2015. 84: 178-86
14. Randazzo M, Pisapia JM, Singh N, Thawani JP. 3D printing in neurosurgery: A systematic review. Surg Neurol Int. 2016. 7: S801-9
15. Rinkel GJ. Intracranial aneurysm screening: Indications and advice for practice. Lancet Neurol. 2005. 4: 122-8
16. Serafin Z, Strześniewski P, Lasek W, Beuth W. Follow-up after embolization of ruptured intracranial aneurysms: A prospective comparison of two-dimensional digital subtraction angiography, three-dimensional digital subtraction angiography, and time-of-flight magnetic resonance angiography. Neuroradiology. 2012. 54: 1253-60
17. Sutradhar A, Park J, Carrau D, Miller MJ. Experimental validation of 3D printed patient-specific implants using digital image correlation and finite element analysis. Comput Biol Med. 2014. 52: 8-17
18. Taki W, Sakai N, Suzuki H, PRESAT Group. Determinants of poor outcome after aneurysmal subarachnoid hemorrhage when both clipping and coiling are available: Prospective registry of subarachnoid aneurysms treatment (PRESAT) in Japan. World Neurosurg. 2011. 76: 437-45
19. Vaishya R, Vaish A.editors. 3D Printing in Orthopedics. Berlin: Springer; 2019. p. 583-90
20. Vanninen R, Koivisto T, Saari T, Hernesniemi J, Vapalahti M. Ruptured intracranial aneurysms: Acute endovascular treatment with electrolytically detachable coils-a prospective randomized study. Radiology. 1999. 211: 325-36
21. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011. 10: 626-36
22. Wang JL, Yuan ZG, Qian GL, Bao WQ, Jin GL. 3D printing of intracranial aneurysm based on intracranial digital subtraction angiography and its clinical application. Medicine (Baltimore). 2018. 97: e11103
23. Wang L, Ye X, Hao Q, Ma L, Chen X, Wang H. Three-dimensional intracranial middle cerebral artery aneurysm models for aneurysm surgery and training. J Clin Neurosci. 2018. 50: 77-82
24. Weinstock P, Prabhu SP, Flynn K, Orbach DB, Smith E. Optimizing cerebrovascular surgical and endovascular procedures in children via personalized 3D printing. J Neurosurg Pediatr. 2015. 16: 584-9
25. Whitaker M. The history of 3D printing in healthcare. Bull R Coll Surg Engl. 2014. 96: 228-9
26. Wurm G, Tomancok B, Pogady P, Holl K, Trenkler J. Cerebrovascular stereolithographic biomodeling for aneurysm surgery. Technical note. J Neurosurg. 2004. 100: 139-45
27. Xu WH, Liu J, Li ML, Sun ZY, Chen J, Wu JH. 3D printing of intracranial artery stenosis based on the source images of magnetic resonance angiograph. Ann Transl Med. 2014. 2: 74
28. Zhao J, Lin H, Summers R, Yang M, Cousins BG, Tsui J. Current Treatment Strategies for Intracranial Aneurysms: An Overview. Angiology. 2018. 69: 17-30