- Department of Neurosurgery, University of South Carolina School of Medicine Greenville, Greenville, United States
- Department of Surgery, College of Medicine, University of Toledo College of Medicine and Life Sciences, Toledo, United States
- Department of Neurological Surgery, University of North Carolina, Chapel Hill, United States
- Department of Neurological Surgery, Miami, United States
- School of Medicine, University of Miami Miller School of Medicine, Miami, United States
- Department of Clinical Medical Sciences, The University of the West Indies, Trinidad and Tobago
Correspondence Address:
Allan D. Levi, Department of Neurological Surgery, University of Miami Miller School of Medicine, Miami, United States.
DOI:10.25259/SNI_580_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mareshah N. Sowah1, Benjamin R. Klein2, Mark Attiah3, Nidia I. Perez Pereda4, Roseanna A. Murray5, Danny Lincoln John5, Avidesh Panday6, Allan D. Levi4. The use of ultrasound-guided imaging to localize peripheral nerve injury in pediatric patients: A case report. 27-Sep-2024;15:347
How to cite this URL: Mareshah N. Sowah1, Benjamin R. Klein2, Mark Attiah3, Nidia I. Perez Pereda4, Roseanna A. Murray5, Danny Lincoln John5, Avidesh Panday6, Allan D. Levi4. The use of ultrasound-guided imaging to localize peripheral nerve injury in pediatric patients: A case report. 27-Sep-2024;15:347. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13124
Abstract
Background: The use of ultrasonography to diagnose and manage peripheral nerve injury is not routinely performed, but is an advantageous alternative to magnetic resonance imaging (MRI) in the pediatric population.
Case Description: The authors report a case of a toddler-aged female who sustained a supracondylar fracture and subsequent median and ulnar nerve injuries. All preoperative and postoperative imaging was performed through high-resolution ultrasound as opposed to MRI. Starting at 6 months post-nerve repair and with 18 months of follow-up, the patient exhibited substantial improvement in motor strength and sensory function. This case demonstrated a successful outcome while providing an imaging alternative that is portable, relatively low-cost, lacks ionizing radiation, provides additional information on vascular integrity, and obviates the need for general anesthetic such as MRI.
Conclusion: The authors conclude that the use of ultrasonography to diagnose and manage traumatic peripheral nerve injury is advantageous, particularly in the pediatric population.
Keywords: Median nerve, Pediatrics, Peripheral nerve, Ulnar nerve, Ultrasounds
INTRODUCTION
Peripheral nerve injuries can cause severe impairment and disrupt regular activities of daily living in patients. Including brachial and lumbar plexus injuries, the global prevalence of peripheral nerve injuries is 5% and can present acutely as a result of a trauma or chronically due to issues such as overstretching.[
Advanced imaging modalities such as computerized axial tomography (CT) scans and magnetic resonance imaging (MRI)-neurography are indicated in the management of various musculoskeletal pathologies; however, alternative imaging methods exist and are under-utilized. Advancements in high-resolution ultrasound have proven to be advantageous in the diagnosis and management of traumatic peripheral nerve injury in pediatrics.[
CASE PRESENTATION
A 4-year-old female was diagnosed with a left supracondylar fracture after falling from a bouncy castle. The diagnosis was made at an outside hospital, and at that time, the patient underwent a closed reduction and percutaneous pinning of the left supracondylar fracture. The patient’s cast and pins were removed 1 month later, and it was noted that she was experiencing left hand weakness with associated claw deformity. Nerve conduction studies showed absent potentials on the left median nerve and left ulnar nerve, and she subsequently presented to the outpatient clinic for evaluation of her left upper extremity weakness.
Performing an adequate neurological physical examination to assess for peripheral nerve damage is difficult in any patient population but is especially challenging in the pediatric setting. Factors that contribute to its difficulty in pediatric patients include their low attention span, difficulty understanding cues and commands, increased irritability, and disinterest. Peripheral nerve injury is largely a clinical diagnosis, so it is imperative to conduct an effective and accurate physical exam. In the patient’s initial neurological examination, the right upper extremity demonstrated 5/5 strength throughout, which provided a reliable baseline. Her left upper extremity motor strength examination showed 5/5 deltoid, 5/5 triceps, 5/5 biceps, 2/5 handgrip, 2/5 interosseous, 0/5 wrist flexion, 0/5 wrist extension, 4/5 thumb flexion, and 4/5 finger extensors. She displayed mild swelling of her left fingers with appropriate capillary refill and denied tenderness to the affected limb. The authors also noted the difference between the strength of wrist extension versus finger extension. The radial nerve controls these movements; there was no evidence of damage on surgical exploration and no complaints signaling radial nerve injury. The authors postulate that the wrist extension strength test findings that were documented could be due to local injury to the wrist and surrounding tissue. Physical examination findings suggested potential ulnar and median nerve injuries [
Video 1
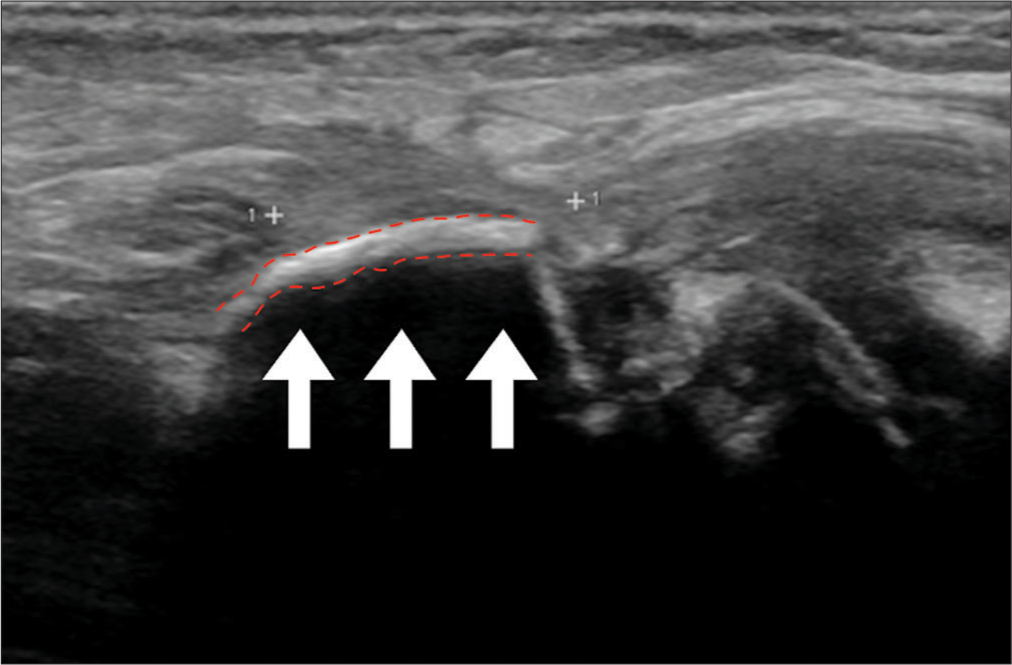
A preoperative ultrasound of the left upper extremity was conducted 9 weeks post-injury to rule out ulnar nerve, median nerve, and/or radial nerve injury. The impression of the preoperative ultrasound was as follows: chronic fracture of the left distal humerus with extensive soft-tissue scarring, mild focal hypoechoic echotexture of the left ulnar nerve, complete discontinuity and scar encasement of the left median nerve at the level of the distal humerus deformity [
The patient’s surgical procedure was performed 12 weeks following her initial injury. Preoperative planning was performed through ultrasound guidance in an interdisciplinary fashion, with neurological surgery and vascular surgery immediately before the operation. The procedure began with an exploration of the left ulnar nerve at the antecubital fossa. Neurolysis of the left ulnar nerve was performed, and the nerve was in continuity. The left median nerve was then identified. The patient was found to have direct penetration and injury of the median nerve secondary to a fracture of the distal humerus [
Figure 3:
Intraoperative image sequence. (a) Depicts severe compression of the left median nerve (yellow) by the distal humerus bone fragment (blue arrow) on initial intraoperative assessment. (b) Decompression and exploration of the left median (yellow) and ulnar (green) nerves in the cubital tunnel to assess for injury. (c) Excision of the left median nerve (yellow) neuroma status-post decompression from bone fragment. (d) Suture of the left median nerve (yellow) to perform primary coaptation.
After 3 weeks, the patient returned to the clinic for cast removal. Physical examination revealed hypersensitivity to touch at the incision site and along the distribution of the left ulnar nerve, no intrinsic muscle function, left long finger flexor tightness, decreased active flexion of the left thumb and index finger, and mild weakness of wrist extensors. She was subsequently fitted for two left forearm-based orthoses to promote functional positioning and prevent contractures. Six months postoperatively, the patient demonstrated noticeable improvements in wrist strength, hand grip, and pincer grasp. She regained the ability to perform a pincer grasp with her left hand, which was exhibited by fastening buttons. Improved grip strength and wrist movement were also noted, as she was able to brush her teeth with minimal difficulty. At 18 months postoperatively, the patient has regained most of her strength and ability to perform most tasks. Mild sensory impairment is present, as she occasionally experiences intermittent numbness and tingling that radiates from her left hand to her left forearm.
DISCUSSION
In this article, we describe a case of a 4-year-old patient who was seen initially for a left supracondylar fracture but was then found to have accompanying left medial and ulnar nerve lesions leading to profound weakness of her left upper extremity. Preoperative high-resolution ultrasonography was performed 9 weeks post-injury in combination with neurophysiologic studies (i.e., nerve stimulation and action potential generation) to explore the extent of peripheral nerve damage. It was found that this patient had experienced left median and ulnar nerve damage. Twelve weeks post-injury, surgical repair of the left median and ulnar nerves was performed. At 6- and 18-month follow-up, the patient had significant improvement in wrist strength and hand grip.
Trauma is the most common cause of pediatric mononeuropathy, and many of these injuries result in neuroma formation.[
Ultrasound also allows for qualitative analysis of tissues using color elastography. This modality showcases the relative difference in tissue stiffness, with a red color representing increased tissue stiffness and a blue color representing decreased tissue stiffness.[
Historically, MRI has been the imaging modality of choice when diagnosing potential peripheral nerve lesions. However, in the pediatric setting, there are instances during which the use of MRI to evaluate the extent of peripheral nerve damage is potentially contraindicated. Examples include acute-phase multi-trauma, the presence of cardiac pacemakers and neurostimulators, and neonatal age and renal injury if contrast must be used.[
While recognizing the setbacks of MRI in the pediatric population, it is also important to be critical of the limitations of ultrasound. For example, ultrasound cannot see through air, bone or other objects that differ in composition from body tissue.[
CONCLUSION
As described in this article, high-resolution ultrasonography is highly useful in the diagnosis, preoperative management, and surgical decision making of traumatic peripheral nerve injury in pediatric patients. It is a safe and reliable imaging modality that also offers the ability to evaluate damage dynamically and interactively. While studies have previously documented the success of using ultrasound to manage peripheral neuropathy, the application of this strategy remains under-utilized. The benefits of ultrasound are numerous, and it is critical to recognize its role in enhancing the management of pediatric patients with peripheral nerve injury.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
The authors give special thanks to Roberto Suazo and Linda Alberga, Department of Neurological Surgery at the University of Miami Miller School of Medicine, for their figure design and editorial assistance.
References
1. Aman M, Zimmermann KS, Boecker AH, Thielen M, Falkner F, Daeschler S. Peripheral nerve injuries in children-prevalence, mechanisms and concomitant injuries: A major trauma center’s experience. Eur J Med Res. 2023. 28: 116
2. Cokluk C, Aydin K, Senel A. Presurgical ultrasound-assisted neuro-examination in the surgical repair of peripheral nerve injury. Minim Invasive Neurosurg. 2004. 47: 169-72
3. Cortes C, Ramos Y, Restrepo R, Restrepo JA, Grossman JA, Lee EY. Practical magnetic resonance imaging evaluation of peripheral nerves in children: Magnetic resonance neurography. Radiol Clin North Am. 2013. 51: 673-88
4. Deshmukh SD, Samet J, Fayad LM, Ahlawat S. Magnetic resonance neurography of traumatic pediatric peripheral nerve injury: Beyond birth-related brachial palsy. Pediatr Radiol. 2019. 49: 954-64
5. Dong SZ, Zhu M, Bulas D. Techniques for minimizing sedation in pediatric MRI. J Magn Reson Imaging. 2019. 50: 1047-54
6. Eljamel MS, Mahboob SO. The effectiveness and cost-effectiveness of intraoperative imaging in high-grade glioma resection; a comparative review of intraoperative ALA, fluorescein, ultrasound and MRI. Photodiagnosis Photodyn Ther. 2016. 16: 35-43
7. Erez O, Khalil JG, Legakis JE, Tweedie J, Kaminski E, Reynolds RA. Ultrasound evaluation of ulnar nerve anatomy in the pediatric population. J Pediatr Orthop. 2012. 32: 641-6
8. Fornage BD. Peripheral nerves of the extremities: Imaging with US. Radiology. 1988. 167: 179-82
9. Gallardo E, Noto Y, Simon NG. Ultrasound in the diagnosis of peripheral neuropathy: Structure meets function in the neuromuscular clinic. J Neurol Neurosurg Psychiatry. 2015. 86: 1066-74
10. Goyal A, Wadgera N, Srivastava DN, Ansari MT, Dawar R. Imaging of traumatic peripheral nerve injuries. J Clin Orthop Trauma. 2021. 21: 101510
11. Koenig RW, Pedro MT, Heinen CP, Schmidt T, Richter HP, Antoniadis G. High-resolution ultrasonography in evaluating peripheral nerve entrapment and trauma. Neurosurg Focus. 2009. 26: E13
12. Lee J, Bidwell T, Metcalfe R. Ultrasound in pediatric peripheral nerve injuries: Can this affect our surgical decision making? A preliminary report. J Pediatr Orthop. 2013. 33: 152-8
13. Missios S, Bekelis K, Spinner RJ. Traumatic peripheral nerve injuries in children: Epidemiology and socioeconomics. J Neurosurg Pediatr. 2014. 14: 688-94
14. Nischal N, Gupta S, Lal K, Singh JP. Performance evaluation of high-resolution ultrasound versus magnetic resonance imaging in diagnosing peripheral nerve pathologies. Indian J Radiol Imaging. 2021. 31: 43-8
15. Noble J, Munro CA, Prasad VS, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma. 1998. 45: 116-22
16. Padua L, Di Pasquale A, Liotta G, Granata G, Pazzaglia C, Erra C. Ultrasound as a useful tool in the diagnosis and management of traumatic nerve lesions. Clin Neurophysiol. 2013. 124: 1237-43
17. Samet JD. Ultrasound of peripheral nerve injury. Pediatr Radiol. 2023. 53: 1539-52
18. Schneider C, Sprenger A, Weiss K, Slebocki K, Maintz D, Fink GR. MRI detects peripheral nerve and adjacent muscle pathology in non-systemic vasculitic neuropathy (NSVN). J Neurol. 2019. 266: 975-81
19. Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, Barr RG. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: Basic principles and terminology. Ultrasound Med Biol. 2015. 41: 1126-47
20. Thukral BB. Problems and preferences in pediatric imaging. Indian J Radiol Imaging. 2015. 25: 359-64
21. Vanderhave KL, Brighton B, Casey V, Montijo H, Scannell B. Applications of musculoskeletal ultrasonography in pediatric patients. J Am Acad Orthop Surg. 2014. 22: 691-8
22. Wee TC, Simon NG. Ultrasound elastography for the evaluation of peripheral nerves: A systematic review. Muscle Nerve. 2019. 60: 501-12
23. Wijntjes J, Borchert A, van Alfen N. Nerve ultrasound in traumatic and iatrogenic peripheral nerve injury. Diagnostics (Basel). 2020. 11: 30
24. Zaidman CM, Seelig MJ, Baker JC, Mackinnon SE, Pestronk A. Detection of peripheral nerve pathology: Comparison of ultrasound and MRI. Neurology. 2013. 80: 1634-40
25. Zeidenberg J, Burks SS, Jose J, Subhawong TK, Levi AD. The utility of ultrasound in the assessment of traumatic peripheral nerve lesions: Report of 4 cases. Neurosurg Focus. 2015. 39: E3