- Department of Neurosurgery, School of Medicine, New York Medical College, Valhalla, United States
- Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York City, New York, United States
- Department of Neurosurgery, University of Virginia, Charlottesville, Virginia, United States
- Department of Neurosurgery, Westchester Medical Center, Valhalla, New York, United States.
Correspondence Address:
Sima Vazquez, School of Medicine, New York Medical College, Valhalla, New York, United States.
DOI:10.25259/SNI_360_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sima Vazquez1, John K. Houten2, Zehavya T. Stadlan1, Jacob D. Greisman1, Grigori Vaserman1, Eris Spirollari1, Tolga Sursal3, Jose F. Dominguez4, Merritt D. Kinon4. Thecal sac ligation in the setting of thoracic spondyloptosis with complete cord transection. 01-Sep-2023;14:304
How to cite this URL: Sima Vazquez1, John K. Houten2, Zehavya T. Stadlan1, Jacob D. Greisman1, Grigori Vaserman1, Eris Spirollari1, Tolga Sursal3, Jose F. Dominguez4, Merritt D. Kinon4. Thecal sac ligation in the setting of thoracic spondyloptosis with complete cord transection. 01-Sep-2023;14:304. Available from: https://surgicalneurologyint.com/surgicalint-articles/12527/
Abstract
Background: Traumatic spondyloptosis (TS) with complete spinal cord transection and unrepairable durotomy is particularly rare and can lead to a difficult-to-manage cerebrospinal fluid (CSF) leak.
Methods: We performed a systematic review of the literature on TS and discuss the management strategies and outcomes of TS with cord transection and significant dural tear. We also report a novel case of a 26-year-old female who presented with thoracic TS with complete spinal cord transection and unrepairable durotomy with high-flow CSF leak.
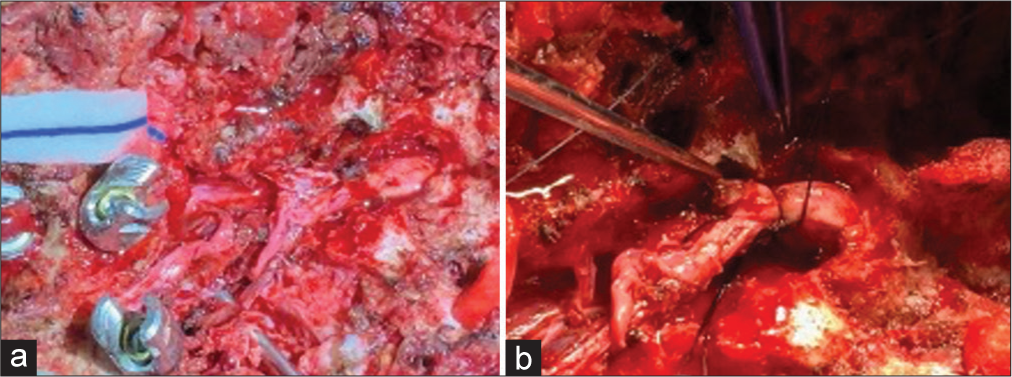
Results: Of 93 articles that resulted in the search query, 13 described cases of TS with complete cord transection. The approach to dural repair was only described in 8 (n = 20) of the 13 articles. The dura was not repaired in two (20%) of the cases. Ligation of the proximal end of the dural defect was done in 15 (75%) of the cases, all at the same institution. One (5%) case report describes ligation of the distal end; one (5%) case describes the repair of the dura with duraplasty; and another (5%) case describes repair using muscle graft to partially reconstruct the defect.
Conclusion: Suture ligation of the thecal sac in the setting of traumatic complete spinal cord transection with significant dural disruption has been described in the international literature and is a safe and successful technique to prevent complications associated with persisting high-flow CSF leakage. To the best of our knowledge, this is the first report of thecal sac ligation of the proximal end of the defect from the United States.
Keywords: Cerebrospinal fluid leak, Cord transection, Dural tear, Thecal sac ligation, Traumatic spondyloptosis
INTRODUCTION
Spondyloptosis is a severe form of spondylolisthesis with complete disruption of all structural elements of the spinal column resulting in severe instability. Traumatic spondyloptosis (TS) is rare but may be caused by high-velocity injury or blunt trauma such as motor vehicle collisions (MVC), falls, or building collapse.[
Long-term complications of polytraumatic spinal cord injury are numerous. If the dura is violated, complications regarding cerebrospinal fluid (CSF) leakage may increase the length of stay and impede the rehabilitation process. Complications during the rehabilitation process may be attributed to long hospital stays or long stays in rehabilitation facilities.[
Few cases have been reported of TS with complete spinal cord transection and associated unrepairable traumatic durotomy.[
MATERIALS AND METHODS
Search strategy
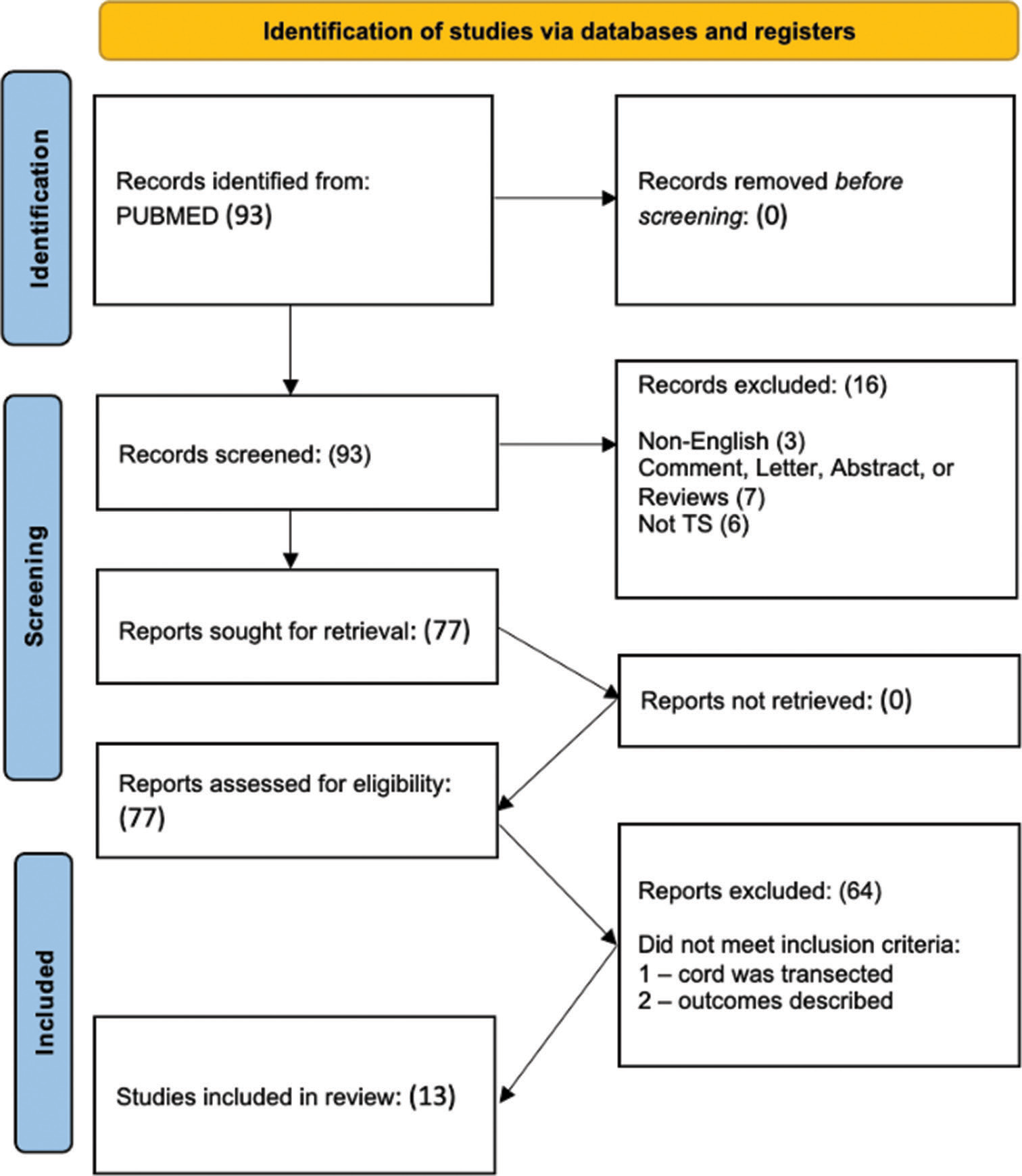
We systematically reviewed the literature in accordance with the preferred reporting items for systematic reviews and meta-analysis guidelines. One author (S.V.) queried PubMed on April 15, 2023, using the search term “traumatic spondyloptosis.” There were no limits on the year of publication. The search query is shown in
Selection process and data collection
After the articles returned in the search were organized, two authors (S.V. and M.D.K.) independently screened the abstracts and titles for relevance. Articles not available in English or articles without full manuscripts were removed. Our inclusion and exclusion criteria were applied to the remaining articles. Articles were included in our study if they met all of the following inclusion criteria: (1) Reported case(s) described TS and (2) complete transection of the cord of dural sac/nerve roots was explicitly stated. Articles were excluded from our study if they met any one of the following exclusion criteria: (1) Article was a literature review, systematic review, or meta-analysis and (2) operative approach to spondyloptosis was not described.
Data items extracted from the included articles were country of origin, year of publication, level of spondyloptosis, approach to the spinal cord or dural repair, presence of postoperative CSF leak, and overall outcomes. A case of TS was also reviewed for presentation.
Study risk of bias assessment
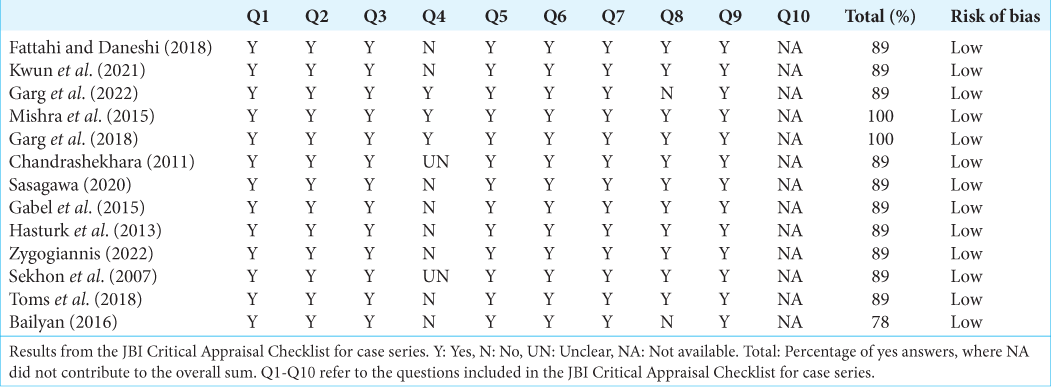
Two reviewers (S.V.) and (E.S.) assessed the risk of bias using the Joanna Briggs Institute Critical Appraisal Checklist for Case Series and Case Reports, respectively. Low risk was defined as an answer of Yes for >75% of the questions [Supplementary
RESULTS
Case presentation
A 26-year-old female was transferred from an outside hospital after sustaining a rollover motor vehicle accident (MVA). She was an unrestrained driver and was violently ejected from the driver’s seat into the back of the car, requiring subsequent extrication by Emergency Medical Services. The patient had no significant past medical history except for a COVID (SARS-CoV-2) infection several months prior and a persistent asymptomatic positive COVID test.
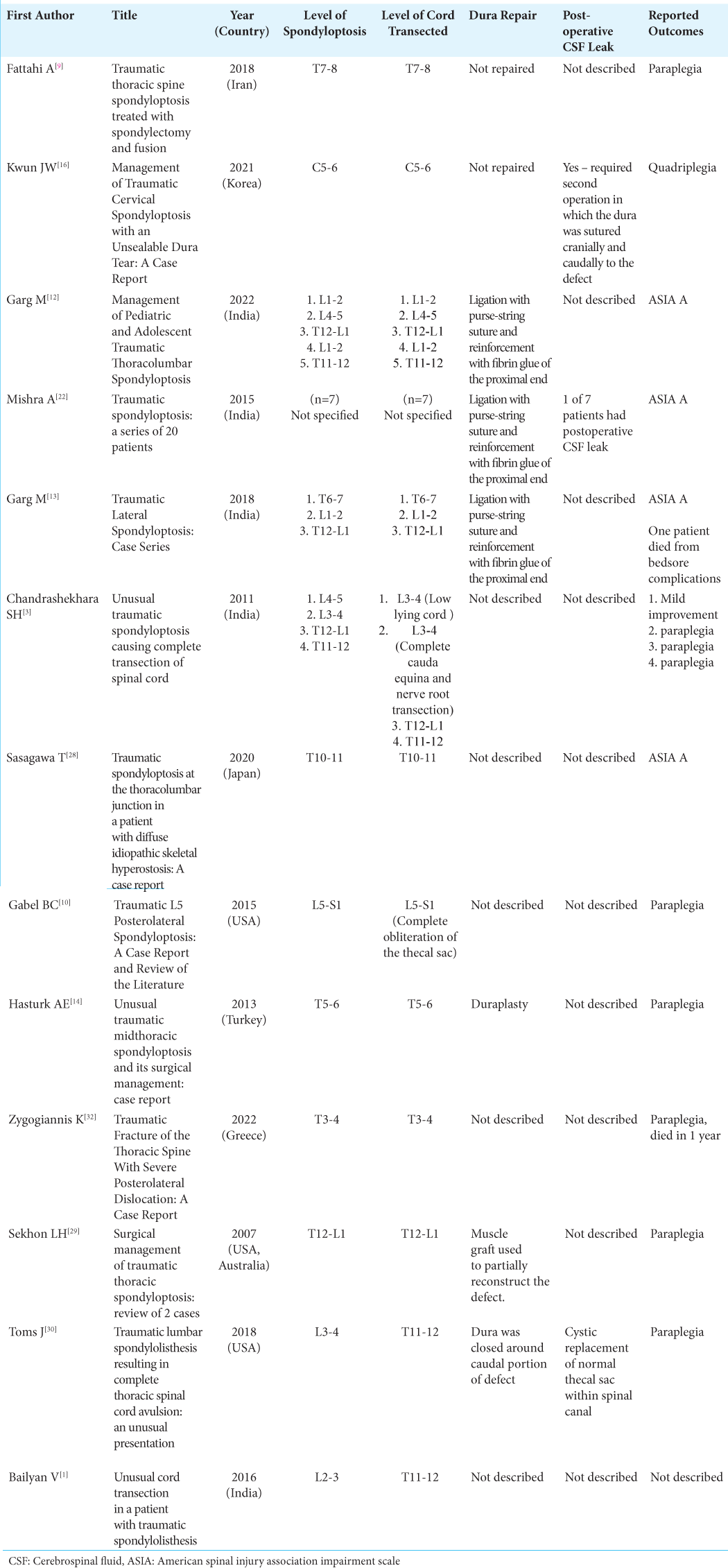
On presentation to our medical center, the patient was awake and talking with normal neurological function in the upper extremities and no motor or sensory function below the T6 level consistent with an ASIA grade A injury. Computed tomography imaging showed bilateral pleural effusions, multiple fractures of the ribs, and traumatic thoracic spondyloptosis of T7 on T8 with anterior and lateral subluxation of the T7 vertebral body compared to the T8 vertebral body [
Figure 2:
Sagittal reconstruction of thoracic computed tomography showing spondyloptosis of T7 on T8 with anterior and lateral subluxation of the T7 vertebral body compared to the T8 vertebral body (a). Sagittal T2-weighted thoracic magnetic resonance imaging showing the disruption and complete transection of the spinal cord at the T7–8 (b).
Operation
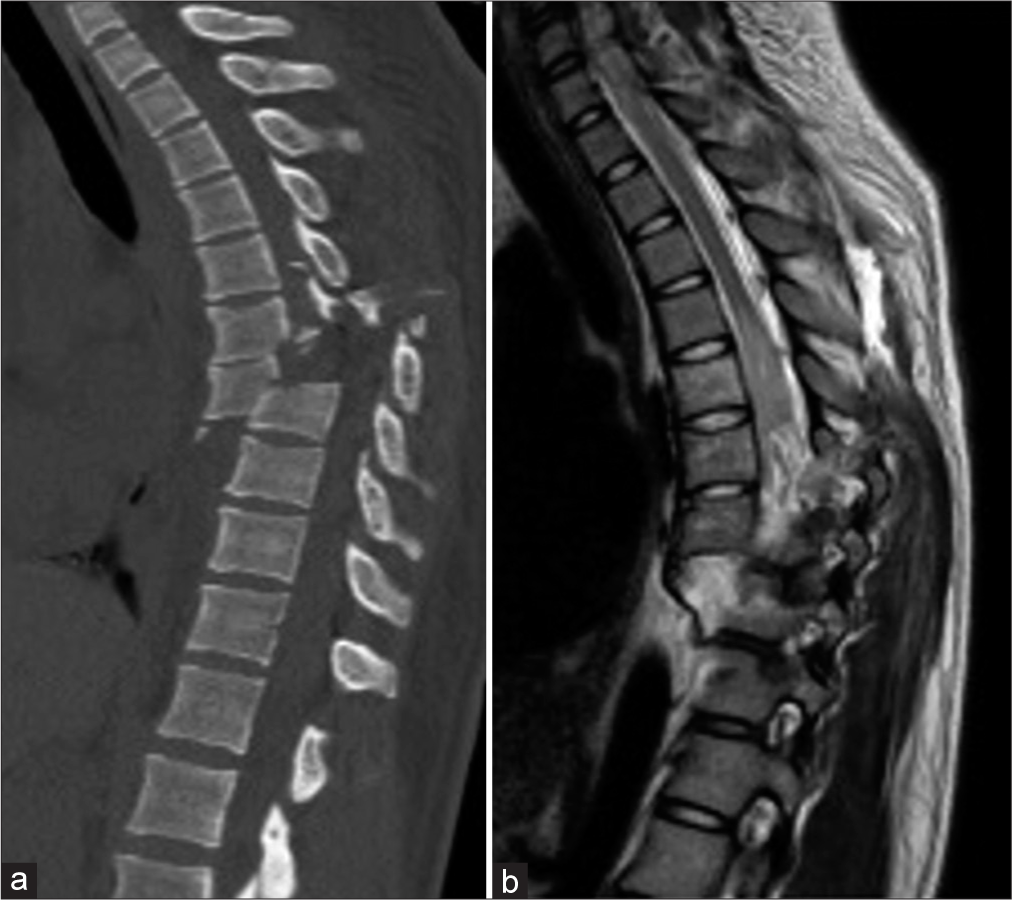
The patient was anesthetized and positioned prone on an open Jackson table (Jackson Spinal Table; Mizuho OSI, Union City, California, USA) with her arms at her sides. Neurophysiologic monitoring was used for this surgery. Prepositioning baseline showed no electrophysiologic signals distal to her injury. Partial closed reduction was performed under fluoroscopy using manual traction and manipulation of the patient’s hips and shoulders. While performing the subperiosteal dissection, several areas of fascial disruption with brisk CSF leakage were encountered. Pedicle screws were placed at T2–T11 with intraoperative stereotactic navigation using the O arm (Medtronic; Minneapolis, Minnesota, USA). After the pedicle screws were placed, attention was turned to exploring the spinal canal. The posterior elements were completely disrupted at T7 and T8. A standard laminectomy was performed from T5 to T8 to expose the spinal canal and examine the dural tube. The dura was severely and circumferentially injured with a large defect of no intervening dura from approximately T6 to T7. From the disrupted ends of the dura, the injured thoracic nerve roots and the transected ends of the spinal cord are shown [
Further reduction of the spine was attempted with the instrumentation. A quad-rod construct was utilized at T7–T8 due to the significant deformity and instability at this level. The posterior lateral fusion was then carried out in the standard fashion with local morselized autograft and allograft protein. The wound was closed in a standard multilayered fashion.
Postoperative course
The postoperative neurologic examination remained unchanged, with no neurologic function below the level of the spinal cord injury but preserved neurologic function above the level of the injury. She made a good recovery from her other traumatic injuries and had no issues from COVID infection. She suffered no CSF leakage or wound healing issues and was ultimately discharged from the hospital to spinal cord rehabilitation.
SYSTEMATIC REVIEW
Search results
Our search query returned 93 articles, of which 13 met the inclusion/exclusion criteria [
Three of the 13 (23.1%) articles were from the USA.[
Repair of durotomy
The dura was deemed nonrepairable and therefore not repaired in two (20%) of the 20 cases.[
Three of the included articles were published from the Department of Neurosurgery of the All India Institute of Medical Science.[
One case describes the repair of a dural defect at T5–6 level with duraplasty and no postoperative CSF leak.[
DISCUSSION
TS is a rare but devastating injury that may occur throughout the spine.[
A retrospective review by Luszczyk et al. analyzed 187 patients at a level 1 trauma center with traumatic dural tears.[
While the specific management of dural traumatic dural tear is case-specific, the general principles involve an attempt to create a watertight primary suture closure or repair using graft material that may be autograft from fascial lata or other sources, or synthetic dural substitute.[
In the case presented in this report, the dural disruption was so extensive that there was a high level of concern for complications associated with persisting, high-flow CSF leak, and ligation of the dura was felt to be the most effective method to avoid complications. Since CSF is produced in the ventricles of the brain proximal to the complete spinal cord transection, we felt thecal sac ligation at the proximal end was sufficient to prevent CSF leakage. Closure of the caudal portion of the defect has been reported and was associated with cystic replacement of the normal thecal sac within the spinal canal. There is precedent for ligation of the dural sac in very specific situations in which satisfactory alternatives are lacking, as in instances of resection of malignancy such as sacral chordoma in which margins are an important goal and very distal.[
CONCLUSION
Suture ligation of the thecal sac in the setting of traumatic complete spinal cord transection with significant dural disruption has been described in the international literature and is a safe and successful technique to prevent complications associated with persisting high-flow CSF leakage. To the best of our knowledge, this is the first report of this technique undertaken in the United States.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
SUPPLEMENTARY MATERIAL
References
1. Baliyan V, Shylendran S, Ajay KY, Kumar A, Gamanagatti S, Sinha S. Unusual cord transection in a patient with traumatic spondylolisthesis. Asian J Neurosurg. 2016. 11: 72
2. Cappuccio M, Corghi A, De Iure F, Amendola L. Traumatic expulsion of T4 vertebral body into the spinal canal treated by vertebrectomy and spine shortening. Spine. 2014. 39: E748-51
3. Chandrashekhara SH, Kumar A, Gamanagatti S, Kapoor K, Mukund A, Aggarwal D. Unusual traumatic spondyloptosis causing complete transection of spinal cord. Int Orthop. 2011. 35: 1671-1675
4. Chen D, Apple DF, Hudson LM, Bode R. Medical complications during acute rehabilitation following spinal cord injury--current experience of the model systems. Arch Phys Med Rehabil. 1999. 80: 1397-401
5. Collins FK. Aseptic resection of intestine: End-to-end anastomosis and immediate restoration of lumen by use of special application of removable looped ligature. Ann Surg. 1922. 76: 739-44
6. Endriga DT, Dimar JR, Carreon LY. Communicating hydrocephalus, a long-term complication of dural tear during lumbar spine surgery. Eur Spine J. 2016. 25: 157-61
7. Fang Z, Tian R, Jia YT, Xu TT, Liu Y. Treatment of cerebrospinal fluid leak after spine surgery. Chin J Traumatol. 2017. 20: 81-3
8. Farooque K, Khatri K, Gupta A. Missed traumatic thoracic spondyloptosis with no neurological deficit: A case report and literature review. Trauma Mon. 2016. 21: e19841
9. Fattahi A, Daneshi A. Traumatic thoracic spine spondyloptosis treated with spondylectomy and fusion. Surg Neurol Int. 2018. 9: 158
10. Gabel BC, Curtis E, Gonda D, Ciacci J. Traumatic L5 posterolateral spondyloptosis: A case report and review of the literature. Cureus. 2015. 7: e277
11. Gandhi J, DiMatteo A, Joshi G, Smith NL, Khan SA. Cerebrospinal fluid leaks secondary to dural tears: A review of etiology, clinical evaluation, and management. Int J Neurosci. 2021. 131: 689-95
12. Garg M, Kumar A, Sawarkar DP, Agrawal M, Singh PK, Doddamani R. Management of pediatric and adolescent traumatic thoracolumbar spondyloptosis. Neurol India. 2022. 70: S182-8
13. Garg M, Kumar A, Sawarkar DP, Singh PK, Agarwal D, Kale SS. Traumatic lateral spondyloptosis: Case series. World Neurosurg. 2018. 113: e166-71
14. Hasturk AE, Ilik K, Coven I, Ozdemir O. Unusual traumatic midthoracic spondyloptosis and its surgical management: Case report. Neurol Med Chir (Tokyo). 2013. 53: 887-9
15. Keynan O, Fisher CG, Boyd MC, O’Connell JX, Dvorak MF. Ligation and partial excision of the cauda equina as part of a wide resection of vertebral osteosarcoma: A case report and description of surgical technique. Spine. 2005. 30: E97-102
16. Kwun JW, Kim SY, Lee SK, Kim YJ. Management of traumatic cervical spondyloptosis with an unsealable dura tear: A case report. Korean J Neurotrauma. 2021. 17: 180-5
17. Lee SE, Chung CK, Jahng TA, Kim CH. Dural tear and resultant cerebrospinal fluid leaks after cervical spinal trauma. Eur Spine J. 2014. 23: 1772-6
18. Li Y, Huang M, Manzano G. Traumatic dorsal spondyloptosis of upper thoracic spine: Case report and novel open reduction technique. Br J Neurosurg. 2020. p. 1-5
19. Lofrese G, Visani J, Cultrera F, De Bonis P, Tosatto L, Scerrati A. Anterior dural tear in thoracic and lumbar spinal fractures: Single-center experience with coating technique and literature review of the available strategies. Life (Basel). 2021. 11: 875
20. Luszczyk MJ, Blaisdell GY, Wiater BP, Bellabarba C, Chapman JR, Agel JA. Traumatic dural tears: What do we know and are they a problem?. Spine J. 2014. 14: 49-56
21. Macki M, Lo SF, Bydon M, Kaloostian P, Bydon A. Post-surgical thoracic pseudomeningocele causing spinal cord compression. J Clin Neurosci. 2014. 21: 367-72
22. Mishra A, Agrawal D, Gupta D, Sinha S, Satyarthee GD, Singh PK. Traumatic spondyloptosis: A series of 20 patients. J Neurosurg Spine. 2015. 22: 647-52
23. Nas K, Yazmalar L, Şah V, Aydın A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015. 6: 8-16
24. Paulo D, Semonche A, Tyagi R. Novel method for stepwise reduction of traumatic thoracic spondyloptosis. Surg Neurol Int. 2019. 10: 23
25. Rao PJ, Lu VM, Sergides IG. Traumatic mid-thoracic spondyloptosis without neurological deficit: A case report and review of literature. ANZ J Surg. 2018. 88: 1083-5
26. Ruggieri P, Angelini A, Ussia G, Montalti M, Mercuri M. Surgical margins and local control in resection of sacral chordomas. Clin Orthop. 2010. 468: 2939-47
27. Ruiz IA, Squair JW, Phillips AA, Lukac CD, Huang D, Oxciano P. Incidence and natural progression of neurogenic shock after traumatic spinal cord injury. J Neurotrauma. 2018. 35: 461-6
28. Sasagawa T, Nakamura T. Traumatic spondyloptosis at the thoracolumbar junction in a patient with diffuse idiopathic skeletal hyperostosis: A case report. J Orthop Sci. 2020. 25: 926-30
29. Sekhon LH, Sears W, Lynch JJ. Surgical management of traumatic thoracic spondyloptosis: Review of 2 cases. J Clin Neurosci. 2007. 14: 770-5
30. Toms J, Boyer DL, Kelman CR, Vega RA. Traumatic lumbar spondylolisthesis resulting in complete thoracic spinal cord avulsion: An unusual presentation. J Neurosurg Spine. 2018. 29: 635-8
31. Yadla S, Lebude B, Tender GC, Sharan AD, Harrop JS, Hilibrand AS. Traumatic spondyloptosis of the thoracolumbar spine. J Neurosurg Spine. 2008. 9: 145-51
32. Zygogiannis K, Manolakos K, Kalampokis A, Thivaios GC, Moschos S. Traumatic fracture of the thoracic spine with severe posterolateral dislocation: A case report. Cureus. 2022. 14: e23830