- Department of Neurosurgery, CHU Ibn Sina Rabat, Morocco,
- Department of thoracic surgery, Chu Ibn Sina Rabat, Rabat, Morocco.
Correspondence Address:
Christine Milena Sayore, Department of Neurosurgery, CHU Ibn Sina Rabat, Morocoo.
DOI:10.25259/SNI_699_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Christine Milena Sayore1, Mustapha Hemama1, Francois de Paule Kossi Adjiou1, Michele Yollande Moune1, Safa Sabur2, Nizare El Fatemi1, Rachid El Maaqili1. Thoracic abscess due to unusual migration of a ventriculoperitoneal shunt and literature review. 13-Sep-2021;12:467
How to cite this URL: Christine Milena Sayore1, Mustapha Hemama1, Francois de Paule Kossi Adjiou1, Michele Yollande Moune1, Safa Sabur2, Nizare El Fatemi1, Rachid El Maaqili1. Thoracic abscess due to unusual migration of a ventriculoperitoneal shunt and literature review. 13-Sep-2021;12:467. Available from: https://surgicalneurologyint.com/surgicalint-articles/11103/
Abstract
Background: Thoracic complications of ventriculoperitoneal (VP) cerebrospinal fluid shunting are rare and the diagnosis is difficult without neurological impairment.
Case Description: We report a case of a 36-year-old woman who had a VP shunt in the right side when she was 13 years for a posterior fossa ependymoma and hydrocephalus. 23 years after surgery, she developed acute yellowfish cough and sputum, and the computed tomography scan found an intrathoracic cyst. She had a thoracotomy for the cyst and during surgery, we found the peritoneal catheter of the VP shunt, with a collected abscess in the left side. The patient was treated for the abscess and the VP shunt was removed. We also review the literature cases of thoracic complications after VP shunts.
Conclusion: Thoracic abscess due to VP shunt migration is extremely rare and could happen after a long time delay VP shunt surgery.
Keywords: Abscess, Migration, Pleural, Pseudocyst, Thoracic, Ventriculoperitoneal shunt
INTRODUCTION
The ventriculoperitoneal (VP) shunts were first introduced in the early 1900s.[
Thoracic complications of VP shunts are rare and rarely reported in the literature, such as pleural effusion, bronchial perforation, pneumothorax, and pneumonia.[
We report the case of a young woman operated for a tumor of the cerebral fossa with hydrocephalus who developed 23 years later a contralateral thoracic abscess due to a migration of the abdominal tip of the VP shunt. We also present a review of the literature.
CASE REPORT
A 36-year-old female patient, with a history of posterior fossa ependymoma, was operated 1997 when she was 13 years old with hydrocephalus. She had prior a VP-Shunt on the right side. No other medical history. The evolution was good with no complications.
In 2020, 8 months ago before her admission, she presented thoracic pains followed by yellowish cough and sputum, without fever and headaches, everything evolving in a context of conservation of general condition.
She was seen prior by the thoracic surgeons, that suspected a hydatic cyst, they performed a thoracic X-ray, that showed a rounded left diaphragmatic collection. She had an abdominal computed tomography (CT) scan that revealed a rounded left diaphragmatic collection with some peripheric calcifications. The dimensions were 31.8 mm × 31.1 mm × 25.5 mm [
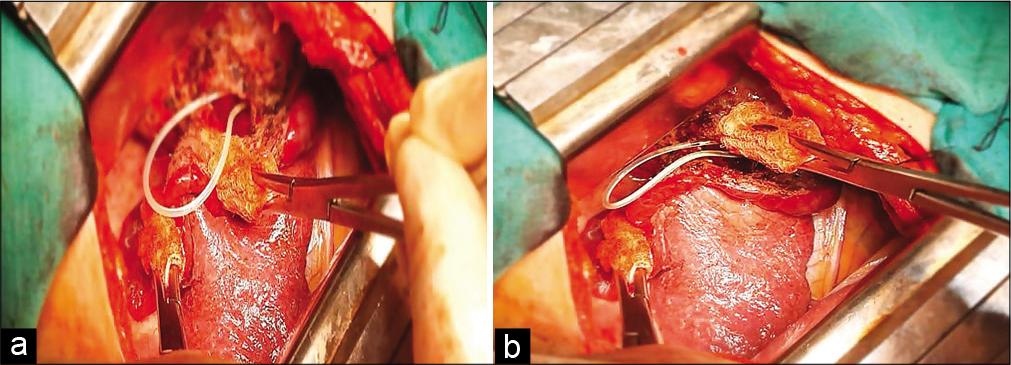
She was turned to the operating room, by thoracic surgeons. She had a thoracotomy and the diaphragm was ruptured, with a mass that they punctured and it was a puriform collection, the wall had been opened and they found a VP Shunt catheter. Then they called the neurosurgeons to the operating room.
When we came, we saw the herniated catheter in the thorax surrounding the abscess that has been removed and drained. The abdominal tip of the VP Shunt was still permeable and the liquid was citrus then gradually thinned out [
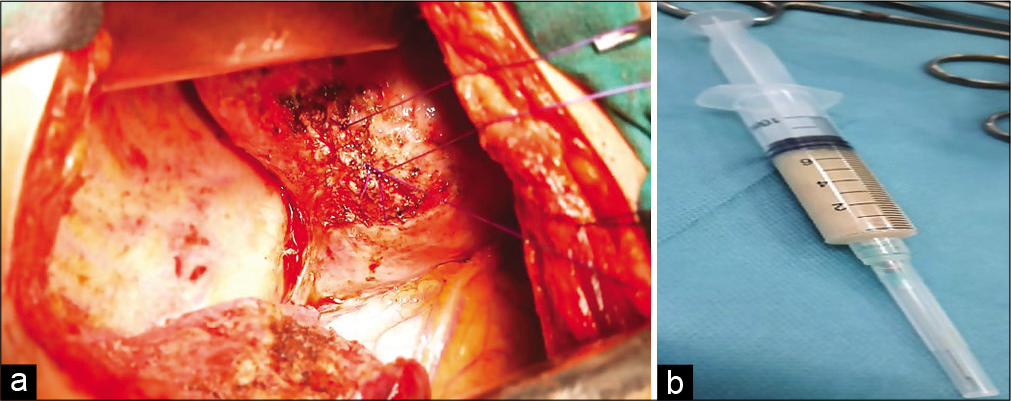
At the same time, we removed the functional VP Shunt after a retro-auricular incision. The ventricular tip was still functional. We removed initially the reservoir and after the distal part in the thorax. We decided to watched her clinically and with a cerebral CT scan and physical examination because of the risk of acute hydrocephalus.
She remained clinically fine with a Glasgow Coma Scale of 15, post-operatively, without headache and vomiting. The biological analysis found a gram-negative bacterium Escherichia coli, and also Beta (2 transferrin a protein-specific of cerebrospinal fluid (CSF) and perilymph was found confirming The CSF Leak treated by Trimethoprim/Sulfamethoxazole and Carbapenem for 14 days and treated as meningitis. The CSF analysis showed a normal dose of glucose and protein but the leukocytes were found 30 cells. The postoperative CT scan was performed and no active dilatation has been observed. The evolution was good without intrathoracic collection and without hydrocephalus. We planned to evaluate her condition 1 month after the infection. Hence, if she remains stable she will not need a shunt again. But if she came with hypertension signs we will choose then to operate.
DISCUSSION
VP shunts surgery is a common surgery for neurosurgeons, a well-known procedure but with its complications. Most frequently those complications are mechanical failures and infections.[
Indeed, the mechanism of migration of the peritoneal catheter into the thorax is analyzed in the literature. Three hypotheses are discussed. First, the migration of the catheter in the thoracic cavity by a supradiaphragmatic route (created during the VP shunt surgery on the passage along with the subcutaneous tissue). Second, through transdiaphragmatic hiatuses (through Bochdalek’s foramen or Morgani’s). Moreover, third the inflammatory reactions induced by the shunt tip can erode the diaphragm and then facilitate the shunt migration into the thorax.[
In our case, we supposed that with the long delay of surgery (23 years) the peritoneal tip has moved in the thorax through the diaphragm through natural hiatuses because of an inflammation induced by the catheter and make our case special. After migration, a pseudocyst is formed and got infected. A part of the catheter was seen in the peritoneal cavity.
In definition, a CSF pseudocyst is a loculated fluid collection, which forms around the distal catheter tip, and is a common cause of distal catheter obstruction. Concerning the mechanisms, multiple factors are thought to predispose to pseudocyst formation such as abdominal surgery, multiple shunt revisions, increased CSF protein, and infectious, inflammatory, and other processes which may affect the resorptive capacity of peritoneal or pleural surfaces.[
We performed research using the following MeSH terms: VP shunt and thoracic abscess, VP shunt and thoracic migration, VP shunt, and thoracic complications, on Pubmed, Science Direct, and Google Scholar, Medline. We did not find a thoracic abscess resulting from VP shunt migration. Hence, we considered our case as extremely rare.
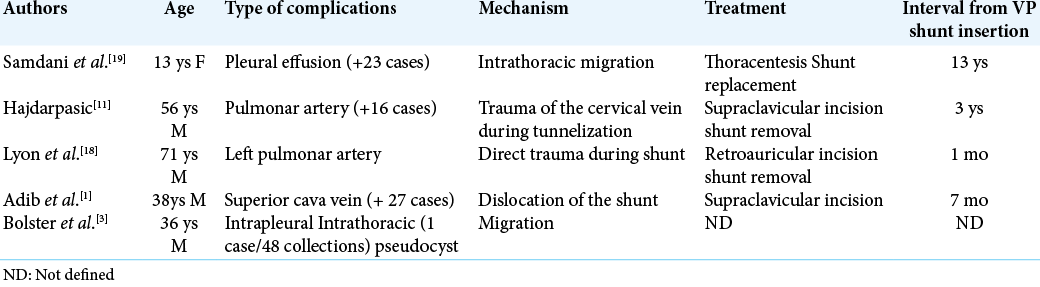
Hence, we reported in the review some of the thoracic complications of a VP shunt migration [
Fewel and Garton[
CONCLUSION
VP shunt complications in the thorax are unusual. Our rare case represented the opportunity to discuss a rare thoracic complication of VP shunt catheter in patients treated for hydrocephalus.
Even if the infected thoracic pseudocyst was not found in the literature yet, some thoracic complications do exist. Hence, patients with respiratory symptoms like respiratory failure, mechanical ventilation, oxygen requirement should get an appropriate examination and imaging with a multidisciplinary discussion before the surgery. This case proved that patients should be followed even after a long time VP shunt surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adib SD, Lescan M, Renovanz M, Schuhmann MU, Trakolis L, Bongers M. Intracardial catheter migration of a ventriculoperitoneal shunt: Pathophysiology and interdisciplinary management. World Neurosurg. 2020. 135: 222-7
2. Andrews EW. An improved technique in brain surgery. Glass tubes versus gold or platinum for subdural drainage of the lateral ventricles in internal hydrocephalus. Q Bull Northwest Univ Med Sch. 1911. 12: 171-9
3. Bolster F, Fardanesh R, Morgan T, Katz DS, Daly B. Cross-sectional imaging of thoracic and abdominal complications of cerebrospinal fluid shunt catheters. Emerg Radiol. 2015. 23: 117-25
4. Bolster F, Fardanesh R, Morgan T, Katz DS, Daly B. Cross-sectional imaging of thoracic and abdominal complications of cerebrospinal fluid shunt catheters. Emerg Radiol. 2016. 23: 117-25
5. Chung JJ, Yu JS, Kim JH, Nam SJ, Kim MJ. Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol. 2009. 193: 1311-7
6. Dabdoub CB, Dabdoub CF, Chavez M, Villarroel J, Ferrufino JL, Coimbra A. Abdominal cerebrospinal fluid pseudocyst: A comparative analysis between children and adults. Childs Nerv Syst. 2014. 30: 579-89
7. Davidoff LM. Treatment of hydrocephalus: Historical review and description of a new method. Arch Surg. 1929. 18: 1737-62
8. Doh JW, Bae HG, Lee KS, Yun IG, Byun BJ. Hydrothorax from intrathoracic migration of a ventriculoperitoneal shunt catheter. Surg Neurol. 1995. 43: 340-3
9. Dossani RH, Maiti TK, Patra DP, Nanda A, Cuellar H. Endovascular retrieval of migrated distal end of ventriculoperitoneal shunt from bilateral pulmonary arteries: A technical note. Ann Vasc Surg. 2017. 45: 305-14
10. Fewel ME, Garton HJ. Migration of distal ventriculoperitoneal shunt catheter into the heart. Case report and review of the literature. J Neurosurg. 2004. 100: 206-11
11. Hajdarpasic E. Sepsis caused by bacterial colonization of migrated distal ventriculoperitoneal shunt catheter into the pulmonary artery: A first case report and literature review. World Neurosurg. 2019. 126: 172-80
12. Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F. Long-term follow-up data from the shunt design trial. Pediatr Neurosurg. 2000. 33: 230-6
13. Key CB, Rothrock SG, Falk JL. Cerebrospinal fluid shunt complications: An emergency medicine perspective. Pediatr Emerg Care. 1995. 11: 265-73
14. Lyon K, Ban VS, Bedros N, Aoun SG, El Ahmadieh TY, White J. Migration of a ventriculoperitoneal shunt into the pulmonary vasculature: Case report, review of the literature, and surgical pearls. World Neurosurg. 2016. 92: 585.e5-11
15. Muramatsu H, Koike K. Pleural effusions appearing in the rehabilitation ward after ventriculoperitoneal shunts: A report of two adult cases and a review of the literature. Brain Injury. 2004. 18: 835-44
16. Nfonsam V, Chand B, Rosenblatt S, Turner R, Luciano M. Laparoscopic management of distal ventriculoperitoneal shunt complications. Surg Endosc. 2008. 22: 1866-70
17. Pathi R, Sage M, Slavotinek J, Hanieh A. Abdominal cerebrospinal fluid pseudocyst. Australas Radiol. 2004. 48: 61-3
18. Porcaro F, Procaccini E, Paglietti MG, Schiavino A, Petreschi F, Cutrera R. Pleural effusion from intrathoracic migration of a ventriculo-peritoneal shunt catheter: Pediatric case report and review of the literature. Ital J Pediatr. 2018. 44: 42
19. Samdani AF, Storm PB, Kuchner EB, Garonzik IM, Sciubba D, Carson B. Ventriculoperitoneal shunt malfunction presenting with pleuritic chest pain. Pediatr Emerg Care. 2005. 21: 261-3
20. Taub E, Lavyne M. Thoracic complications of ventriculoperitoneal shunts: Case report and review of the literature. Neurosurgery. 1994. 34: 181-3
21. Vinchon M, Baroncini M, Delestret I. Adult outcome of pediatric hydrocephalus. Childs Nerv Syst. 2012. 28: 847-54
22. Vinchon M, Rekate H, Kulkarni AV. Pediatric hydrocephalus outcomes: A review. Fluids Barriers CNS. 2012. 9: 18
23. Wallace AN, McConathy J, Menias CO, Bhalla S, Wippold FJ. Imaging evaluation of CSF shunts. AJR Am J Roentgenol. 2014. 202: 38-53